DRM is a highly prevalent condition in Spanish hospitals and is associated to increased healthcare costs. Costs associated to DRM were calculated using the methods of the PREDyCES study. The potential savings derived from specialized nutritional treatment were calculated by extrapolating the results of the SNAQ strategy.
ResultsMedian cost per procedure in patients with DRM was €9679.85, with a final cost of €28,700,775.2. The cost of each patient with DRM was 2.63 times higher than the cost of patients with no DRM. The potential cost saving associated to specialized nutritional treatment was estimated at €1,682,317.28 (5.86% of total cost associated to DRM).
ConclusionsPatients with DRM showed a higher consumption of financial resources as compared to well-nourished patients. Specialized nutritional treatment is a potential cost-saving procedure.
La DRE es una entidad con alta prevalencia en nuestro medio hospitalario y conlleva un aumento de los costes sanitarios. Siguiendo la metodología del estudio PREDyCES se estimó el coste asociado a DRE. El ahorro potencial asociado al tratamiento especializado de la DRE se calculó extrapolando los datos de la estrategia SNAQ.
ResultadosLa mediana del coste por proceso en pacientes con DRE ascendió a 9.679,85€/proceso, lo que supuso un coste final de 28.700.775,2 €. Cada paciente con DRE consumió 2,63 veces más recursos económicos que los pacientes sin DRE. El ahorro potencial asociado al tratamiento especializado de la DRE se estimó en 1.682.317,28€ (5,86% del gasto asociado a la DRE).
ConclusionesLos pacientes con DRE presentaron un consumo de recursos muy superior al de pacientes normonutridos. Un tratamiento nutricional especializado supondría un ahorro potencial significativo.
Disease-related malnutrition (DRM) is very common in the Spanish hospital setting, with an estimated prevalence of 20–70%.1 Only one national multicentric study has been published in this regard—the Prevalence of Malnutrition and Associated Costs study (Prevalencia de Desnutrición y Costes Asociados [PREDyCES©])2—which established a prevalence of malnutrition under conditions of routine clinical practice of 23% using the Nutritional Risk Screening 2002 (NRS-2002) tool.3 This study moreover showed patients with malnutrition to be associated to greater resource consumption, referred particularly to a longer mean stay, compared with patients without malnutrition. This observation was particularly notorious among the patients that developed malnutrition during admission, with doubling of the estimated costs vs those patients that maintained normal nutrition during admission (12,237€ vs 6408€). Furthermore, DRM is associated to increased comorbidity and mortality, as acknowledged by the competent European authorities.4,5 The aim of the present study is to establish the economical impact of DRM in a Spanish third-level hospital and to estimate the potential savings derived from its treatment, extrapolating the data published in the literature based on the Short Assessment Nutritional Questionnaire (SNAQ)6,7 strategy.
Material and methodsThree sub-studies were carried out in order to address the following issues: cost of a malnourished patient in the study center; estimated annual total cost derived from DRM in the center; and potential savings if the screening rates and therapeutic objectives of the SNAQ strategy were reached, according to the latest published information.6
Sub-study 1. Quantification of the cost associated to the management of a patient with Nutritional Risk Screening 2002 positivity at some point during hospital admissionType of studyA cross-sectional study was carried out under conditions of routine clinical practice.
Sample size estimationAccording to the PREDyCES© study,2 which defines malnutrition as an NRS-2002 score of >3 points, the mean cost of the 468 malnourished patients included in the sample is 9239€, with a standard deviation (SD) of 1731€. Using the formula n=Zα2∗S2d2, where Zα=1.96, S2=(1731)2 and d=360 (0.4% of the mean price per malnourished patient according to the PREDyCES©), we estimate a necessary sample size of 89 malnourished patients according to the NRS-2002 in order to establish the mean cost of a malnourished patient with a confidence level of 95% and a precision of 4%.
Screening of study candidatesThe patient screening criteria were: prescription of artificial nutrition via the oral, enteral, parenteral or mixed route by the physician in charge of the patient or by the specialist in Endocrinology and Nutrition of the Nutritional Support Unit, after receiving the request from the Department in charge; patient age over 18 years; and the obtainment of informed consent. The patients came from the same Departments in Hospital San Pedro de Alcántara (HSPA), except Pediatrics, Intensive Care and Maternity. Patients rejecting the intervention or who failed to give consent were excluded, in the same way as those patients with stays of under 48h.
Collection of the study dataA total of 210 patients, all admitted to HSPA, were included during the period between September 2013 and June 2014. Nutritional screening with the NRS-2002 tool was performed upon admission (with the collection of sociodemographic data, which could be done retrospectively if nutritional support was started 48h after admission), at the start of specialized nutritional support (if requested), and at hospital discharge. The duration of hospital stay was also recorded. Body weight and height were determined using a scale with a telescopic measuring rod (Seca 769, Seca gmbh & co. Hammer Steindamm. Hamburg, Germany). In those cases where the above anthropometric data could not be obtained, height was estimated from the ankle-knee distance and weight, using the following predictive formula:
- •
Male weight=(CB×1.37)+(0.98×CP)+(0.37×PT)+(1.16×TR)−81.69.
- •
Female weight=(0.98×CB)+(1.27×CP)+(0.4×PT)+(0.87×TR)−62.39.
Those patients with NRS-2002 ≥3 points in any of the screenings performed (n=175) were subsequently included. The final sample was selected from this population using a random sampling tool of the SPSS© v. 20 statistical package for MS Windows (SPSS Inc., IL, USA). In order to increase the statistical power of the analysis, we decided to raise the sample size to at least 100 individuals. In order to establish the individual cost of each patient, we classified each subject according to his or her diagnosis-related group (DRG)—the diagnosis being that reflected in the hospital discharge report, using the “All-patients” (AP-DRG v 27.0) and the Alcor© program. The Management Control Department of the health authorities of Extremadura was asked to supply the most current data referred to cost (measured in €) and mean stay (in days) corresponding to each DRG for the Cáceres Hospital Complex (year 2013). We calculated the mean cost of each day of stay for a given DRG by dividing the mean cost of the process by the gross mean stay corresponding to the latter. Based on the mean cost per stay, we calculated the total cost of the process of each individual by multiplying the mean cost of stay of the DRG assigned to the patient by the total stay measured in days of the process.
Statistical analysisThe variable “mean cost” was expressed as the arithmetic mean with the corresponding standard deviation (SD) in the presence of a normal distribution, and as the median and range in the presence of a non-normal distribution. The normal distribution of this variable was assessed using the Kolmogorov–Smirnov test. Data processing was carried out with the SPSS version 20 statistical package for MS Windows (SPSS Inc., IL, USA).
Sub-study 2. Estimation of the total cost of the patients with disease-related malnutrition in the period of one yearThe Management Control Department of the health authorities of Extremadura was asked to supply the total cost (including direct and indirect costs) corresponding to the patients assisted in the Cáceres Hospital Complex (which includes HSPA and Nuestra Señora de la Montaña Hospital) for the year 2013 (latest data available on the date of the study). Knowing the estimated prevalence of DRM in HSPA,8 the mean cost of a patient with DRM in HSPA, and the number of admissions to the Cáceres Hospital Complex during the year 2013 (obtained from the Coding Unit of the center), we calculated the total cost of the patients with DRM as corresponding to: annual total cost ([number of admissions to HSPA during 2013]×[prevalence of DRM in HSPA]×[mean cost of a patient with DRM]). The percentage cost attributable to DRM was calculated as the difference between the annual total cost of the patients with DRM divided by the annual total cost.
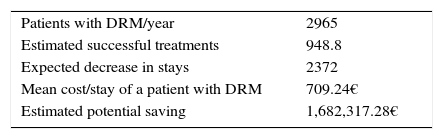
Sub-study 3. Estimated cost savings associated to quality specialized nutritional careThe calculation was based on the results published by the Dutch health authorities within the SNAQ strategy,6 considering that if screening of 80% of the admissions is achieved on an early basis, and the requirements are met in the first year in 40% of the patients with DRM, this would imply a decrease of 2.5 days of stay among the patients with DRM.7 To this effect we estimated the number of patients with DRM in HSPA in the period of one year, with application of the coefficients 0.8 (patients screened) and 0.4 (patients reaching nutritional requirements)—thus obtaining the estimated number of patients with successful nutritional treatments. The expected decrease in stays was calculated by multiplying the number of patients by 2.5. Knowing the cost per stay of a patient with DRM in HSPA in Cáceres, the estimated potential cost saving associated to quality specialized nutritional care (understood as care controlled by a Nutritional Support Unit supervised by a specialist in Endocrinology and Nutrition) was calculated by multiplying cost per stay by the potential number of reducible stays.
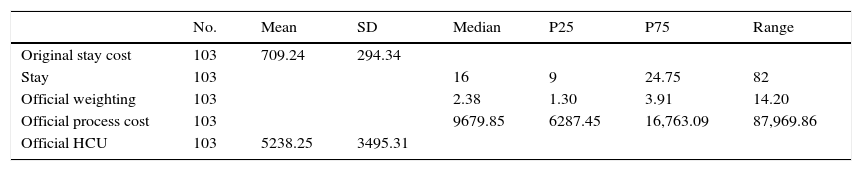
ResultsQuantification of the cost associated to the management of a patient with Nutritional Risk Screening 2002 positivity at some point during hospital admissionA total of 210 patients were assisted during the study period. Of these, 175 presented an NRS-2002 score of over 3 points at some timepoint analyzed during admission. After excluding the patients with stays of under 48h, and those cases in which the information contained in the hospital minimum basic data set and in the discharge report did not allow classification of the patient into any of the established DRGs (therefore being classified as DRG 470, i.e., non-groupable), the sample was reduced to 160 patients. Following randomization, we obtained 104 patients (65 males and 39 females): 63 were admitted to medical Departments, while 41 were admitted to surgical Departments. The median stay in these Departments was 16 days (range 82; interquartile range [IQR] 9–24.5). The median cost per process was 9679.85€ (range 87,969.86; IQR 6287.45–16,763.09). The results are shown in Table 1.
Results of the economical indicators referred to the treatment costs study in patients with an NRS-2002 score of >3 points.
| No. | Mean | SD | Median | P25 | P75 | Range | |
|---|---|---|---|---|---|---|---|
| Original stay cost | 103 | 709.24 | 294.34 | ||||
| Stay | 103 | 16 | 9 | 24.75 | 82 | ||
| Official weighting | 103 | 2.38 | 1.30 | 3.91 | 14.20 | ||
| Official process cost | 103 | 9679.85 | 6287.45 | 16,763.09 | 87,969.86 | ||
| Official HCU | 103 | 5238.25 | 3495.31 |
SD: standard deviation; HCU: Hospitalization Costs Unit.
The Departments participating in the study assisted 13,575 patients during the year 2013, with a total of 19,825 patients assisted in the Cáceres Hospital Complex over that period, according to the data supplied by the Coding Unit.
Of these patients, 21.84% (2965 subjects, representing 14.95% of the total patients assisted in the Cáceres Hospital Complex) presented criteria of malnutrition according to the NRS-2002 tool, based on the data estimated by the authors (Doctoral Thesis).
The total cost of the care of these patients, calculated as the median cost associated to the care of a malnourished patient multiplied by the total malnourished patients, corresponded to 28,700,755.2€, while the total cost for the Cáceres Hospital Complex was 100,895,278.75€ (figure supplied by the Management Control Department of the health authorities of Extremadura).
The cost of the care of malnourished patients in the studied Departments (14.95% of the global cost) represented 28.45% of the resources of the Cáceres Hospital Complex during the year 2013, i.e., each malnourished patient of the HSPA consumed 2.628 times more resources than those who were not malnourished.
Estimated cost savings associated to quality specialized nutritional careThe data are shown in Table 2.
DiscussionOn estimating the cost of a malnourished patient using the NRS-2002 tool, the difference between the mean cost in the PREDyCES© study (9239€)1 and the median cost in our own study (9679.85€) is seen to be comparable and therefore plausible.
The total cost of the care of these patients, calculated as the median cost associated to the care of a malnourished patient multiplied by the total malnourished patients, corresponded to 28,700,755.2€, while the total cost for the Cáceres Hospital Complex was 100,895,278.75€. The estimation was made with the standardized prices referred to 2013. On extrapolating the data to the current period based on the variation of the National General Index according to the base Consumer Prices Index System 2016, from January 2013 to March 2017 (1.1% increment),9 the cost of the care of a malnourished patient would be 10,647.83€ per patient, with a global cost for the Cáceres Hospital Complex of 31,570,830.72€. In the light of these figures, it can be extrapolated that each patient with DRM according to the NRS-2002 consumes 2.628 times more resources than a patient without DRM. Higher resource consumption among patients with DRM is consistent with the data found in the literature.
The economical benefits of nutritional therapy with success targets published in the literature and determined in the routine clinical practice setting would represent a potential saving of 5.86% of the costs generated by patients with DRM and 1.67% of the annual budget destined to a hospital of this category.
ConclusionsThe cost associated to a patient with DRM in HSPA was estimated to be 9679.85€.
The cost associated to DRM in HSPA was 28,700,755.2€, which represents a resource consumption 2.628 times greater than in the population of patients without DRM. On updating the economical data to the current period, these costs were seen to increase, reaching 10,647.83€ per patient with DRM and 31,570,830.72€ globally for DRM in the Cáceres Hospital Complex.
The economical impact of a global specialized nutritional intervention in the mentioned center would imply an estimated cost saving of 5.86% of the expenditure of the Cáceres Hospital Complex destined to patients with DRM and 1.67% of the annual total expenditure.
Conflict of interestThe authors state that they have no conflicts of interest.
Please cite this article as: Morán López JM, Enciso Izquierdo FJ, Luengo Pérez LM, Beneítez Moralejo B, Piedra León M, de Luis DA, et al. Impacto económico de la desnutrición relacionada con la enfermedad en el hospital San Pedro de Alcántara. Estimación del ahorro asociado a una atención nutricional especializada de calidad. Endocrinol Diabetes Nutr. 2017;64:446–450.