The pituitary gland is an atypical location of metastases from any tumor, accounting for only 1% of all pituitary neoplasms.1,2 The most common origin of such metastatic lesions is the breast in women and the lung in men,1,3,4 and only 2.5–18.2% are symptomatic, usually manifesting as diabetes insipidus, ocular disorders or headache.3–5 We describe two cases with different forms of presentation.
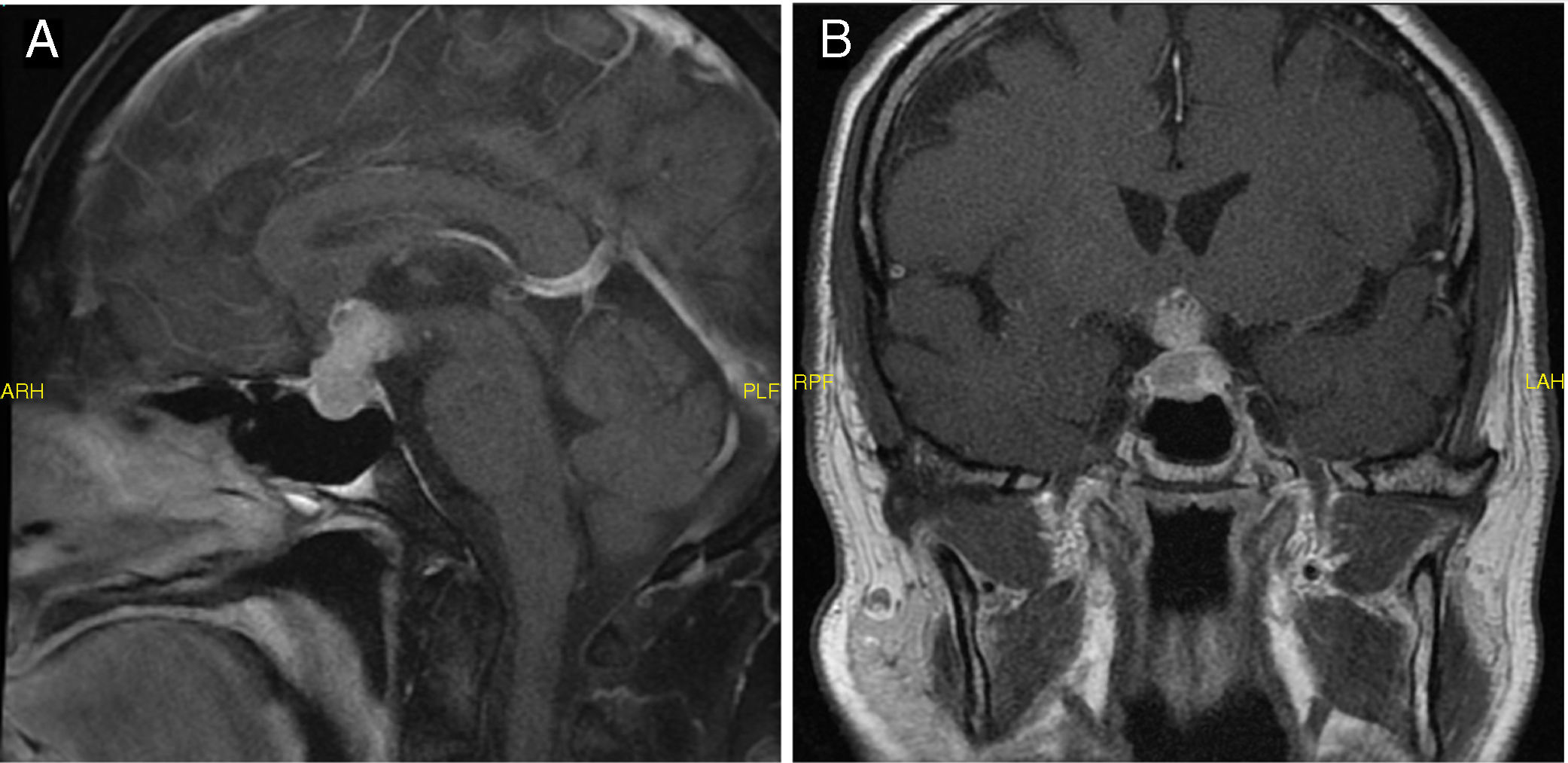
Case 1: A 69-year-old male with no relevant disease history was referred to Endocrinology due to suspected secondary hypothyroidism with decreased TSH (0.15mIU/l) and free T4 levels (0.4ng/dl). He reported fatigue and drowsiness, xerosis, polydipsia and polyuria over the previous month. Expanded laboratory testing confirmed secondary hypothyroidism, with the detection of decreased testosterone (0.03ng/ml) and cortisol (2.3μg/dl), as well as increased urine output (7000ml/day) with low urine osmolality (124mOsm/kg). A diagnosis of adrenal insufficiency, hypogonadotropic hypogonadism, and diabetes insipidus was established. Replacement therapy was started with hydrocortisone, levothyroxine and desmopressin, followed by a considerable clinical improvement and weight recovery. Magnetic resonance imaging (MRI) revealed a pituitary gland tumor measuring 24mm×13mm×14mm in size, with heterogeneous contrast uptake (Fig. 1A). The campimetric findings were normal. The patient was referred to neurosurgery for removal of the tumor. In order to better plan surgery, upon admission MRI was repeated, which revealed that the pituitary tumor had grown considerably in size in one month, with diameters of 32mm×35mm×32mm, compressing the optic chiasm. Campimetry showed bitemporal hemianopsia. Following transsphenoidal surgery, the pathology study showed the lesion to correspond to metastatic tissue. A computed tomography (CT) study of disease spread was performed, and lung adenocarcinoma was identified as the primary tumor.
Case 2: A 51-year-old woman was referred due to pituitary macroadenoma. The patient history included infiltrating ductal carcinoma of the breast with lymph node and bone metastases at diagnosis. Treatment was thus provided with tamoxifen, goserelin, surgical castration and palliative radiotherapy, after which stable disease was observed with tamoxifen alone. Prior to cancer treatment she had regular menstrual periods, and after castration showed amenorrhea. The patient reported to Ophthalmology due to diminished visual acuity, and after showing bitemporal hemianopsia, she was sent to the emergency room. She reported headache, asthenia and weight loss, with no galactorrhea or polyuria or polydipsia. Upon admission, MRI revealed a pituitary tumor measuring 22mm×19mm×13mm in size, displacing the optic chiasm and consistent with pituitary macroadenoma (Fig. 1B). Laboratory tests revealed marked hyperprolactinemia (prolactin [PRL] 228 and 211ng/ml) and low cortisol (4.1μg/dl), TSH (0.29mIU/l), free T4 (0.52ng/dl), FSH (2.2mIU/ml) and LH (0.8mIU/ml). A differential diagnosis between macroprolactinoma and metastasis was therefore considered. The deficits were corrected, and treatment was started with cabergoline. The patient showed a considerable improvement of her asthenia and gained weight. The MRI study was repeated, with no changes in the lesion. The patient was therefore referred to neurosurgery for surgical removal, followed by a clear improvement of her problems with vision. The pathology study showed the excised tissue to correspond to metastatic breast carcinoma. Radiotherapy was subsequently provided (21Gy).
Pituitary gland metastases account for 3–5% of all intracranial metastases.1,2 The most common origin is the breast (20–30%) and lung (30–50%),1,3,4,6 and such lesions may constitute the first presentation of the underlying primary tumor.5 Only 2.5–18.2% of all pituitary metastases are symptomatic,5 the most common manifestation being central diabetes insipidus (case 1), though they may also manifest as headache, visual field abnormalities, anterior pituitary dysfunction and hyperprolactinemia1,3,7 (case 2). Clinically, and as in our first case, disease progression is typically much faster for metastases than for adenomas.8
Determining whether a pituitary tumor is primary or secondary is important for treatment, but it is difficult to do so without pathological confirmation. Since diabetes insipidus is a very rare symptom in pituitary adenoma (<1%)4 and is more common in metastatic forms (42%),5 it is the most important clinical manifestation differentiating metastasis from adenoma,1 as occurred in case 1. However, in case 2 there were no clinical signs of diabetes insipidus, and the prolactin levels were so high that a differential diagnosis between prolactinoma and metastasis was considered. On the one hand, treatment with tamoxifen should cause a decrease in prolactin and an increase in LH and FSH,9 in contrast to what was seen in the laboratory tests in case 2. On the other hand, previous studies report that hyperprolactinemia is present in 6.3% of all pituitary metastases, with a mean value of <160ng/ml due to stem compression,2 while levels of >200ng/ml are more suggestive of prolactinoma.8,10 The cases reported in the reviewed literature confirm this pattern, with prolactin between 35 and 152ng/ml.3,8,10 By contrast, in our case the prolactin concentration was 228ng/ml, which complicated the diagnosis. Finally, visual field changes are not useful for distinguishing between adenoma and metastasis, though rapid vision impairment and its association with weight loss or diabetes insipidus may be an interesting differentiating factor,5 as occurred in case 1.
Once the pituitary tumor is confirmed to be of metastatic origin, treatment should be decided upon. This is usually palliative and dependent upon the extent of the disease and the symptoms.2 Exploration and surgical decompression alone or in combination with radiotherapy are essential if the pathological diagnosis guides treatment, or for providing relief from symptoms and improved quality of life if the spread of the tumor toward the suprasellar region is causing compressive clinical signs or vision problems,3,4,10 as in case 2 at onset and in case 1 prior to surgery. The pituitary lesion is the cause of death in only 13% of the patients.5
Pituitary gland metastases are uncommon. However, the diagnosis of metastasis should be suspected in the presence of rapid onset diabetes insipidus, ocular disease, headache and hyperprolactinemia, as well as in rapidly progressing adenomas, with a view to establishing an early diagnosis and appropriate treatment.
Please cite this article as: Cardona-Rovira MG, Casañ-Fernández R, Sanz-Gallur J, Almonacid-Folch E, Nadal-Máñez A. Metástasis hipofisarias de tumores sólidos: 2 casos de diferente presentación. Endocrinol Diabetes Nutr. 2019;66:202–203.