Permanent hypoparathyroidism is the most common long-term complication after total thyroidectomy, causing significant morbidity and requiring long-term replacement therapy. Our study objective was to assess whether intact parathyroid hormone (iPTH) levels on the first day after total thyroidectomy are a good predictor of permanent hypoparathyroidism.
Patients and methodsA retrospective observational study of all patients undergoing total thyroidectomy between January 2009 and December 2014. iPTH and calcium levels were measured the first day after surgery. Patients were followed up for at least one year after surgery.
ResultsThe study group consisted of 481 patients with a mean age of 53±14 years, 82% of them females. The most common reason for thyroidectomy was multinodular goiter (75%), followed by papillary thyroid cancer (15%). Transient hypocalcemia was the most common early complication after total thyroidectomy (49%), and permanent hypoparathyroidism was the most common long-term complication (6%). ROC curve analysis showed that iPTH level on the first postoperative day was a good predictor of permanent hypoparathyroidism (area under the curve 0.87; 95% CI: 0.84–0.91). Cut-off iPTH levels of 5pg/mL had 95% sensitivity, 77% specificity, 21.6% positive predictive value, and 99.6% negative predictive value.
ConclusionsiPTH level on the first day after total thyroidectomy is a useful predictor of permanent hypoparathyroidism because of its high negative predictive value. Serum iPTH levels >5pg/mL virtually exclude presence of permanent hypoparathyroidism.
El hipoparatiroidismo permanente es la complicación a largo plazo más prevalente tras una tiroidectomía total, siendo responsable de una importante morbilidad y de necesidad de tratamiento sustitutivo a largo plazo. El objetivo de este estudio fue determinar si el valor de la hormona paratiroidea intacta (PTHi) en el primer día postoperatorio tras una tiroidectomía total es un buen predictor de hipoparatiroidismo permanente.
Material y métodosEstudio retrospectivo de observación en el que se analizaron todos los pacientes intervenidos de tiroidectomía total entre enero de 2009 y diciembre de 2014. Se recogieron los valores de PTHi y calcio sérico en el primer día postoperatorio, y todos los pacientes tuvieron un seguimiento mínimo de un año.
ResultadosSe incluyeron 481 pacientes con una edad media de 53±14 años, el 82% de los cuales eran mujeres. La causa más frecuente de tiroidectomía fue el bocio multinodular (75%), seguido del carcinoma papilar de tiroides (15%). La complicación precoz más frecuente fue la hipocalcemia transitoria (49%), y a largo plazo fue el hipoparatiroidismo permanente (6%). El estudio estadístico mediante curvas ROC mostró que la PTHi en el primer día postoperatorio es un buen predictor de hipoparatiroidismo permanente (área bajo la curva de 0,87; IC 95%: 0,84–0,91). Valores de 5pg/ml presentan una sensibilidad del 95%, una especificidad del 77%, un valor predictivo positivo del 21,6% y un valor predictivo negativo del 99,6%.
ConclusionesLa PTHi en el primer día postoperatorio de la tiroidectomía total es un predictor útil de hipoparatiroidismo permanente gracias a su alto valor predictivo negativo. Valores de PTHi>5 pg/ml excluyen prácticamente la presencia de hipoparatiroidismo permanente.
Hypocalcemia, recurrent laryngeal nerve palsy and repeat surgery due to bleeding are the three most common complications associated with thyroid surgery. Permanent hypoparathyroidism is the most prevalent long-term complication, and is responsible for significant morbidity and the need for long-term replacement therapy.
Postoperative permanent hypoparathyroidism is caused by damage to the parathyroid glands when total thyroidectomy is performed, either by inadvertent excision, direct damage or devascularization.1 The associated risk factors reported in the literature include lymphadenectomy associated with thyroidectomy due to malignant disease,2,6 a prolonged duration of surgery (>120min),6 the volume of thyroid surgery performed by the surgeon,3 Graves’ disease,5 patients with thyroiditis,9 repeat surgery due to bleeding, and the identification of less than two parathyroid glands.10
According to the meta-analysis published by Edafe et al. in 2014, transient hypocalcemia has a prevalence of 19–38%, with a permanent hypoparathyroidism rate of 0–3%,10 though these figures vary greatly in the literature due to the different criteria and limiting values used in determining such complications.
Different studies have shown that a decrease in intact parathyroid hormone (iPTH) to below the normal range in the immediate postoperative period (<24h) following total thyroidectomy is a reliable indicator for predicting postoperative transient hypocalcemia.11–14 This is because iPTH has a short half-life (2–5min) with a rapid plasma turnover (through hepatic and renal metabolism), thus making it a good marker of parathyroid function.8
In this regard, a number of protocols have been proposed for the early initiation of replacement therapy in transient hypocalcemia based on calcium and vitamin D, but few studies have analyzed the role of the postoperative measurement of iPTH in predicting the development of permanent hypoparathyroidism.1,7–9
The main objective of this study was to determine whether iPTH levels on the first postoperative day after total thyroidectomy may be useful in predicting which patients will experience permanent hypoparathyroidism, avoiding the risks associated with the development of hyper- or hypocalcemia, and individualizing therapy.
Material and methodsPatients and methodsAll patients undergoing total thyroidectomy at Hospital Universitario Puerta de Hierro (Majadahonda, Madrid, Spain) between January 2009 and December 2014 were included in the study. The baseline data and follow-up data were recorded from the case history, including demographic characteristics, the preoperative diagnosis, and postoperative complications.
Total thyroidectomy using the standard technique was performed in all cases, completed with central and/or lateral lymphadenectomy in patients with thyroid carcinoma, as indicated according to the medical criterion. The procedure was performed by surgeons who specialized in endocrine surgery, or by general surgical residents under the supervision of such surgeons.
The following inclusion criteria were established: all patients in our center subjected to total thyroidectomy due to benign or malignant thyroid disease, or on a prophylactic basis due to RET oncogene mutation. Patients with prior hemithyroidectomy who completed total thyroidectomy in second surgery, or individuals subjected to any other previous neck surgery, were excluded from the study.
Transient hypoparathyroidism was defined as serum iPTH below the normal range (<15pg/ml) at 24h postsurgery, while postoperative hypocalcemia was defined as serum calcium <8mg/dl at 24h postsurgery, and permanent hypoparathyroidism as the need for calcium and vitamin D supplementation more than 12 months after surgery. The serum calcium values used in the study were not corrected for albumin.
Blood samples for calcium and iPTH determination were collected from the first day after surgery at 7:00a.m. (16–20h after surgery), while on the subsequent days only calcium was recorded during the hospitalization period.
Calcium measurements were performed using the Arsenazo III colorimetric method (ADVIA® XPT – Siemens Healthineers), while iPTH was measured by chemiluminescent immunoassay (ADVIA® Centaur – Siemens Healthineers). The manufacturer-reported iPTH reference range was 4.4–1900pg/ml, with a test sensitivity <2.5pg/ml and functional sensitivity <6.4pg/ml.
Initial monitoring and treatment during hospital admission were jointly conducted by the general surgery and endocrinology team, while outpatient monitoring was carried out in the endocrinology clinic.
Study design and statistical analysisA retrospective observational study was carried out. Data are reported as the mean and standard deviation (SD), or as the median and interquartile range (IQR). Statistical significance was considered for p<0.05.
The comparison of two independent continuous variables was based on the Student t-test for unpaired samples, or on the nonparametric Mann–Whitney U-test, depending on the characteristics of the variables. The chi-squared test with continuous correction was used to compare discrete variables.
The receiver operating characteristic (ROC) curves and AUC (area under the curve) were used to assess the diagnostic accuracy of the iPTH value on the first postoperative day or of the differential serum calcium value between the first postoperative day and presurgery as predictors of permanent hypoparathyroidism.
The statistical analysis was performed using the SPSS version 20.0 statistical package (SPSS Inc., Chicago, IL, USA).
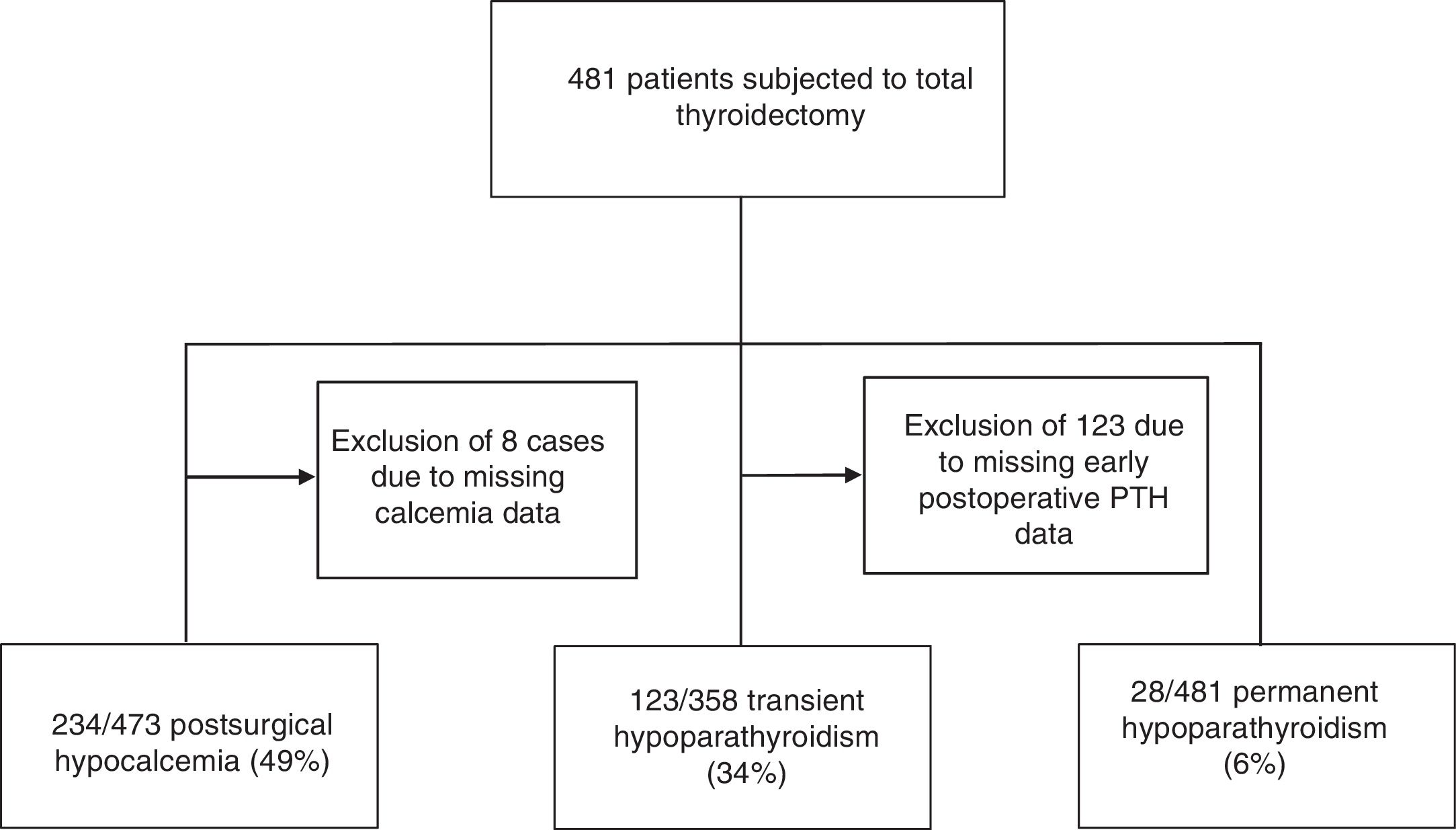
ResultsA total of 481 patients with a mean age of 53±14 years (82% women) were included in the study. In the analysis of transient hypoparathyroidism, 123 patients (26%) with no postoperative iPTH measurements were excluded, due to the impossibility of analyzing this parameter at our center at weekends. The number of patients studied in relation to this analysis was therefore restricted to 358 (Fig. 1).
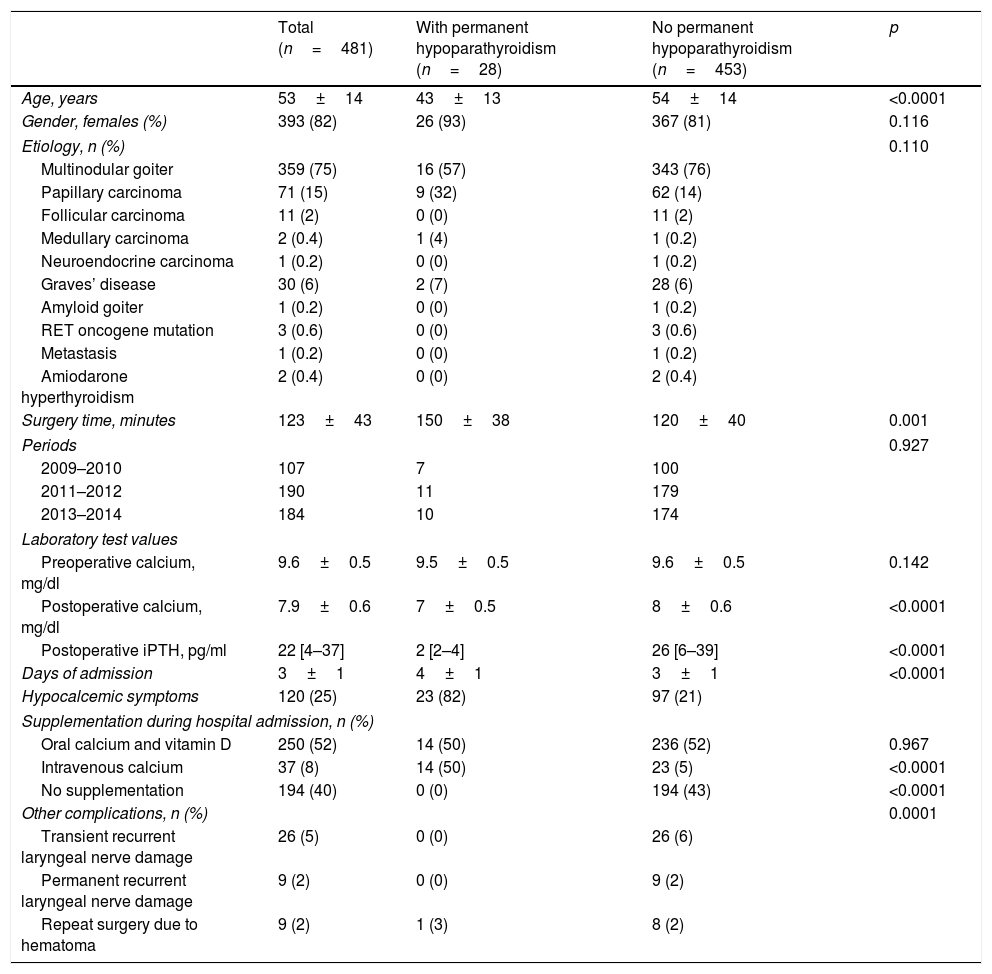
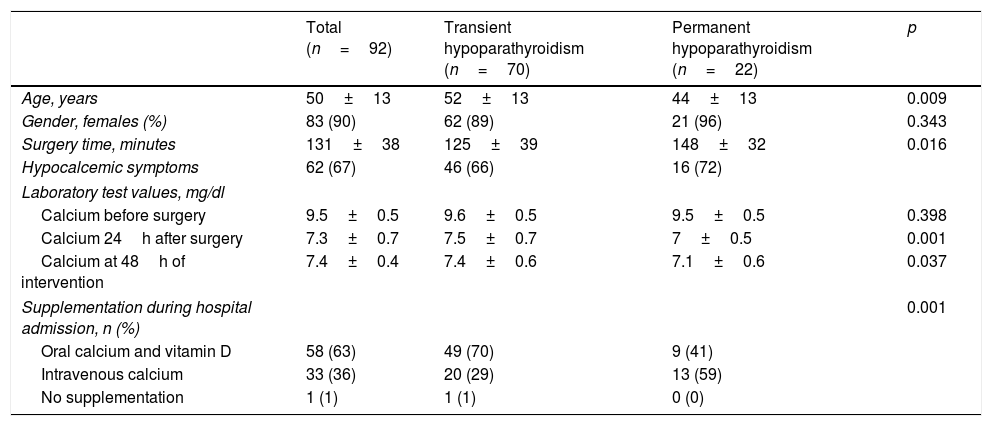
Table 1 describes the main baseline clinical and laboratory test characteristics, and the postoperative complications. To summarize the findings, the most common cause of thyroidectomy was multinodular goiter (75%), followed by papillary thyroid carcinoma (15%), Graves’ disease (6%) and follicular carcinoma (2%).
Clinical, laboratory test and follow-up data of the patients according to whether permanent hypoparathyroidism developed or not.
| Total (n=481) | With permanent hypoparathyroidism (n=28) | No permanent hypoparathyroidism (n=453) | p | |
|---|---|---|---|---|
| Age, years | 53±14 | 43±13 | 54±14 | <0.0001 |
| Gender, females (%) | 393 (82) | 26 (93) | 367 (81) | 0.116 |
| Etiology, n (%) | 0.110 | |||
| Multinodular goiter | 359 (75) | 16 (57) | 343 (76) | |
| Papillary carcinoma | 71 (15) | 9 (32) | 62 (14) | |
| Follicular carcinoma | 11 (2) | 0 (0) | 11 (2) | |
| Medullary carcinoma | 2 (0.4) | 1 (4) | 1 (0.2) | |
| Neuroendocrine carcinoma | 1 (0.2) | 0 (0) | 1 (0.2) | |
| Graves’ disease | 30 (6) | 2 (7) | 28 (6) | |
| Amyloid goiter | 1 (0.2) | 0 (0) | 1 (0.2) | |
| RET oncogene mutation | 3 (0.6) | 0 (0) | 3 (0.6) | |
| Metastasis | 1 (0.2) | 0 (0) | 1 (0.2) | |
| Amiodarone hyperthyroidism | 2 (0.4) | 0 (0) | 2 (0.4) | |
| Surgery time, minutes | 123±43 | 150±38 | 120±40 | 0.001 |
| Periods | 0.927 | |||
| 2009–2010 | 107 | 7 | 100 | |
| 2011–2012 | 190 | 11 | 179 | |
| 2013–2014 | 184 | 10 | 174 | |
| Laboratory test values | ||||
| Preoperative calcium, mg/dl | 9.6±0.5 | 9.5±0.5 | 9.6±0.5 | 0.142 |
| Postoperative calcium, mg/dl | 7.9±0.6 | 7±0.5 | 8±0.6 | <0.0001 |
| Postoperative iPTH, pg/ml | 22 [4–37] | 2 [2–4] | 26 [6–39] | <0.0001 |
| Days of admission | 3±1 | 4±1 | 3±1 | <0.0001 |
| Hypocalcemic symptoms | 120 (25) | 23 (82) | 97 (21) | |
| Supplementation during hospital admission, n (%) | ||||
| Oral calcium and vitamin D | 250 (52) | 14 (50) | 236 (52) | 0.967 |
| Intravenous calcium | 37 (8) | 14 (50) | 23 (5) | <0.0001 |
| No supplementation | 194 (40) | 0 (0) | 194 (43) | <0.0001 |
| Other complications, n (%) | 0.0001 | |||
| Transient recurrent laryngeal nerve damage | 26 (5) | 0 (0) | 26 (6) | |
| Permanent recurrent laryngeal nerve damage | 9 (2) | 0 (0) | 9 (2) | |
| Repeat surgery due to hematoma | 9 (2) | 1 (3) | 8 (2) | |
The most common complication in our series was transient postoperative hypocalcemia, observed in up to 49% of the patients (234 out of 473 cases, as postoperative calcemia was not determined in the remaining cases). Of these patients, 25% had symptoms associated with hypocalcemia such as perioral and limb paresthesias, muscle spasms, or positive Trousseau or Chvostek signs.
Postoperative hypoparathyroidism was another associated complication, and proved transient in 123 patients (34%) and permanent in 28 (6%) (Fig. 1).
The patients who developed long-term permanent hypoparathyroidism were significantly younger, and the surgery time was longer, than in the group that did not develop hypoparathyroidism. However, no significant differences were observed between the different causes of thyroidectomy.
In order to determine whether the incidence of postoperative permanent hypoparathyroidism could be related to the learning curve of the surgical team during the study period, we analyzed the number of procedures and complications in three periods, with no significant differences being observed (Table 1).
Table 2 shows the clinical characteristics of the patients with suppressed iPTH in the early postoperative period (<5pg/ml), according to whether they developed permanent hypoparathyroidism over the long term or not.
Characteristics and laboratory test parameters of the patients with postoperative PTH under 5pg/ml according to the development of transient or permanent hypoparathyroidism over the long term.
| Total (n=92) | Transient hypoparathyroidism (n=70) | Permanent hypoparathyroidism (n=22) | p | |
|---|---|---|---|---|
| Age, years | 50±13 | 52±13 | 44±13 | 0.009 |
| Gender, females (%) | 83 (90) | 62 (89) | 21 (96) | 0.343 |
| Surgery time, minutes | 131±38 | 125±39 | 148±32 | 0.016 |
| Hypocalcemic symptoms | 62 (67) | 46 (66) | 16 (72) | |
| Laboratory test values, mg/dl | ||||
| Calcium before surgery | 9.5±0.5 | 9.6±0.5 | 9.5±0.5 | 0.398 |
| Calcium 24h after surgery | 7.3±0.7 | 7.5±0.7 | 7±0.5 | 0.001 |
| Calcium at 48h of intervention | 7.4±0.4 | 7.4±0.6 | 7.1±0.6 | 0.037 |
| Supplementation during hospital admission, n (%) | 0.001 | |||
| Oral calcium and vitamin D | 58 (63) | 49 (70) | 9 (41) | |
| Intravenous calcium | 33 (36) | 20 (29) | 13 (59) | |
| No supplementation | 1 (1) | 1 (1) | 0 (0) | |
A total of 287 patients (60%) required calcium supplementation with or without vitamin D supplements during admission, and of these 37 (8%) required intravenous calcium. In 53 patients (11%), prophylactic treatment with calcium supplements was started at the discretion of the treating medical team after surgery because the postoperative PTH levels were not available and the serum calcium levels were at the lower limit of normal.
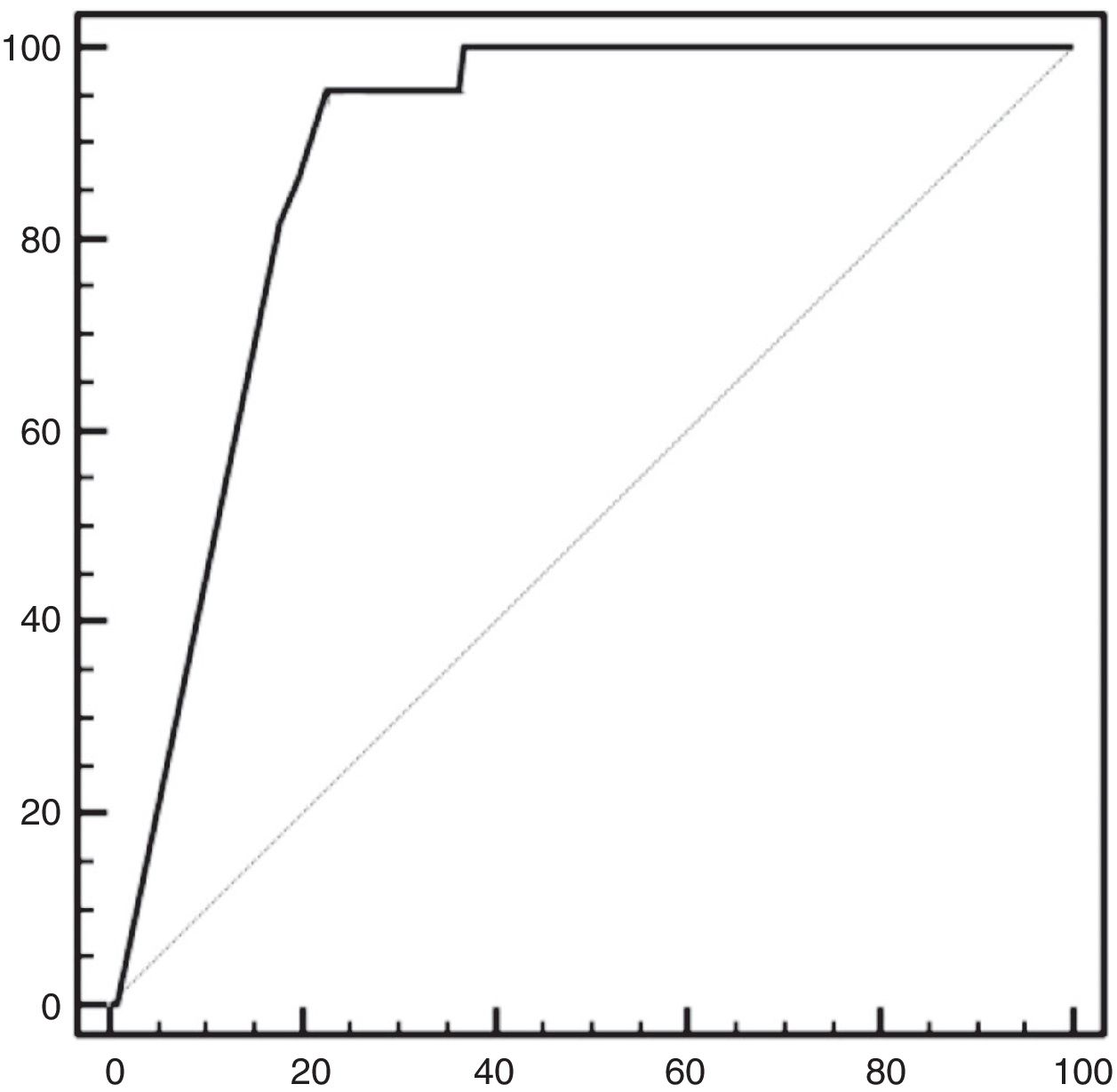
In the statistical analysis of iPTH after 24h as a predictor of permanent hypoparathyroidism, the ROC curves showed iPTH 5pg/ml to exhibit a sensitivity of 95.4% and a specificity of 77.4%, with an increase in the latter as the iPTH levels decreased (Fig. 2). The positive predictive value (PPV) was 21.6% and the negative predictive value (NPV) 99.6%.
Sensitivity did not reach 100% because one patient in the series had a normal iPTH value (15pg/ml) on the first postoperative day, though he subsequently developed permanent hypoparathyroidism.
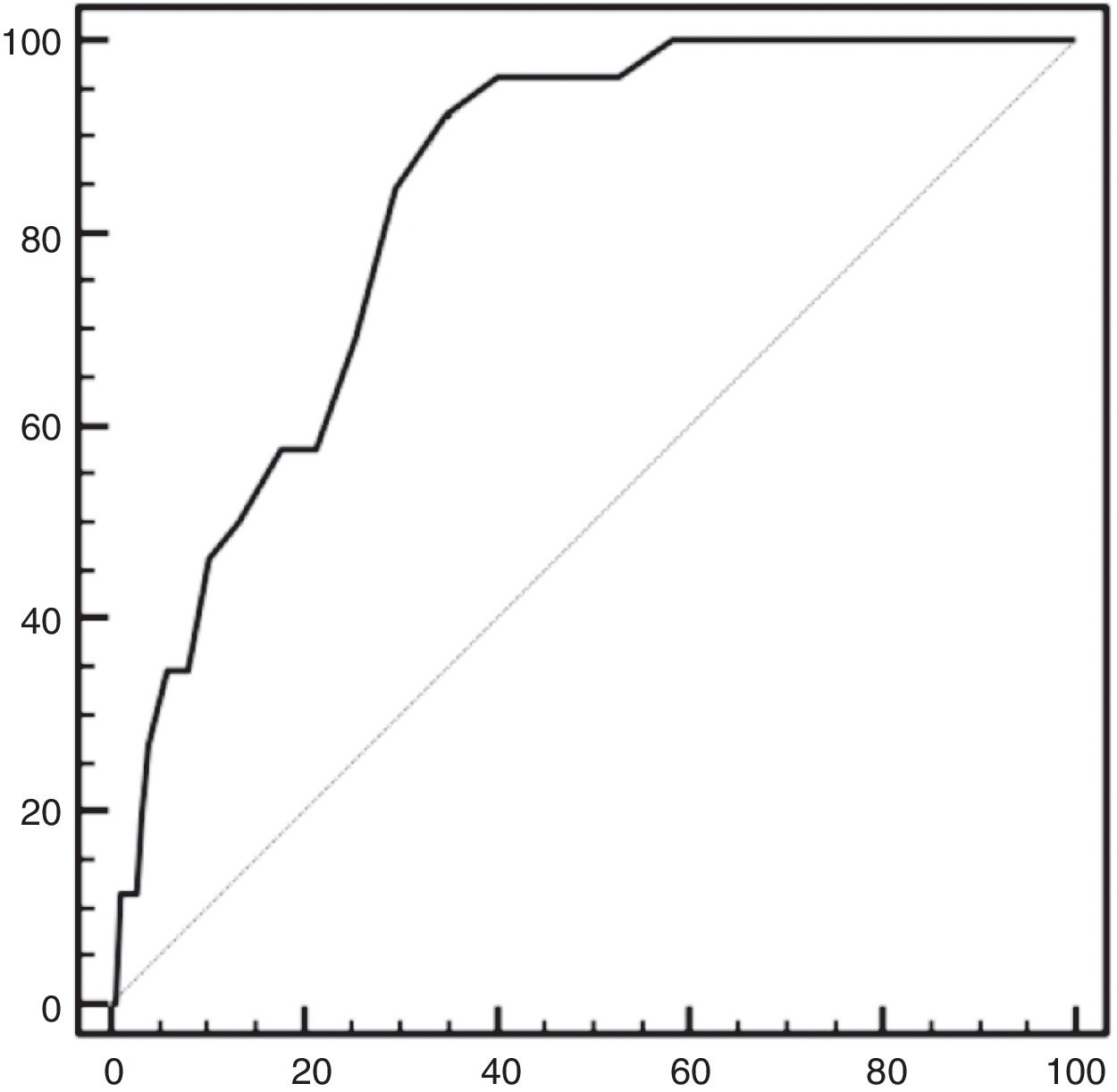
The differential serum calcium value (postoperative versus preoperative) was also evaluated. Based on the analysis of the ROC curves, a decrease of 1.8mEq/l exhibited a sensitivity of 92% and a specificity of 65% in predicting permanent hypoparathyroidism (Fig. 3).
DiscussionThe results of this study show permanent hypoparathyroidism after total thyroidectomy to be an uncommon complication when performed by an experienced surgical team, and that postoperative iPTH levels >5pg/ml may help predict which patients will not develop this complication.
The development of postoperative permanent hypoparathyroidism is associated with increased morbidity and healthcare costs. In order to reduce this complication, the preservation of as many parathyroid glands as possible is important, in the same way as the prevention of direct gland damage and devascularization during surgery, since as demonstrated by Lorente-Poch et al., the prevalence of hypocalcemia, and of transient and permanent hypoparathyroidism is inversely correlated to the number of preserved parathyroid glands.4
The permanent hypoparathyroidism rate reported in the literature is highly variable, one of the reasons for this being the lack of unified biochemical and time criteria. The permanent hypoparathyroidism rate ranges from 1 to 11%.1,4,6–8,15 In our series the prevalence was 6%.
Intact PTH is an excellent marker of parathyroid function thanks to its short half-life. Its fundamental physiological role is based on calcium homeostasis through calcium resorption by the renal tubules, the stimulation of calcium absorption at intestinal level, and the stimulation of bone resorption.
In our study, an iPTH level of 5pg/ml on the first postoperative day after total thyroidectomy exhibited a sensitivity of 95% and a specificity of 77% in predicting permanent hypoparathyroidism, with a PPV of 21.6% and an NPV of 99.6%. These results suggest that if the iPTH levels obtained on the first postoperative day are >5pg/ml, the likelihood of developing long-term permanent hypoparathyroidism is negligible, and that approximately one in every 5 individuals who develop iPTH<5pg/ml will suffer permanent hypoparathyroidism.
As reported in the results, one patient developed permanent hypoparathyroidism with an iPTH value of 15pg/ml. Promberger et al.16 described this phenomenon in a series of 8 patients, suggesting the probable existence of a minimum number of functioning parathyroid cells intensely stimulated by persistent hypocalcemia, but with insufficient iPTH production to restore normal serum calcium levels. Thus, the authors considered that in these cases it would be more appropriate to speak of parathyroid insufficiency rather than permanent hypoparathyroidism.
Only a few previous studies have analyzed the same variable, and the results have been similar to our own. Almquist et al. reported a permanent hypoparathyroidism rate of 19% in patients with iPTH<6.6pg/ml on the first postoperative day.1 Julian et al. in turn found iPTH≤5.8pg/ml recorded 24h after total thyroidectomy to exhibit 100% sensitivity and 82% specificity in predicting permanent hypoparathyroidism, with a PPV of 30% and an NPV of 100%.7 Hermann et al. found that iPTH<6pg/ml recorded 3h after surgery exhibited a PPV of 15% and an NPV of 100% in predicting permanent hypoparathyroidism, and that iPTH>6pg/ml ruled out the presence of permanent hypoparathyroidism.8 Lastly, Wang et al. found iPTH<7pg/ml on the first postoperative day to be predictive of permanent hypoparathyroidism, with a sensitivity of 100% but a specificity of 70%.9
Another variable analyzed as a possible predictor of permanent hypoparathyroidism was the decrease in serum calcium recorded at 24h postsurgery versus the preoperative serum calcium value. The statistical study based on the ROC curves found a decrease of 1.8mEq/l to exhibit a sensitivity of 92% and a specificity of 65% in predicting permanent hypoparathyroidism, i.e., this variable is a comparatively poor indicator. Serum calcium as an indicator was also analyzed by Julian et al., who found a serum concentration ≤1.95mmol/l to exhibit a sensitivity of 60% and a specificity of 79% in predicting permanent hypoparathyroidism, with a PPV of 18% and an NPV of 96%.7
Our study has limitations. Given the retrospective design involved, no firm causal relationships could be established, and since the study was carried out at a single center with concrete treatment criteria, generalization of the results might not be warranted. In addition, the percentage of parathyroid glands removed at surgery and/or autotransplanted was likewise not analyzed. Despite these limitations, however, and thanks to the large number of patients analyzed, our study provides relevant clinical information about the complications associated with total thyroidectomy.
In conclusion, although there is no specific iPTH value after total thyroidectomy allowing for the highly reliable prediction of the development of permanent hypoparathyroidism, the measurement of this parameter is useful because of its high NPV. Thus, postoperative serum iPTH>5pg/ml means we can practically discard the development of permanent hypoparathyroidism over the long term, and this in turn can contribute to establishing both optimal treatment and individualized outpatient follow-up.
Conflicts of interestThere are no conflicts of interest.
Please cite this article as: Calvo Espino P, Rivera Bautista JÁ, Artés Caselles M, Serrano González J, García Pavía A, García-Oria MJ, et al. Uso del valor de la hormona paratiroidea intacta en el primer día postoperatorio tras tiroidectomía total como predictor de hipoparatiroidismo permanente. Endocrinol Diabetes Nutr. 2019;66:195–201.
This study was presented as an Oral Communication at the XXXI National Congress of Surgery, 7–10 November 2016, in Madrid (Spain).






![The receiver operating characteristic (ROC) curve shows the precision of the PTH concentration on the first postoperative day in predicting permanent hypoparathyroidism. Area under the curve 0.87 (0.91–0.84 with 95% confidence interval [95%CI]). The receiver operating characteristic (ROC) curve shows the precision of the PTH concentration on the first postoperative day in predicting permanent hypoparathyroidism. Area under the curve 0.87 (0.91–0.84 with 95% confidence interval [95%CI]).](https://static.elsevier.es/multimedia/25300180/0000006600000003/v1_201904190633/S2530018019300393/v1_201904190633/en/main.assets/thumbnail/gr2.jpeg?xkr=ue/ImdikoIMrsJoerZ+w96p5LBcBpyJTqfwgorxm+Ow=)
![Receiver operating characteristic (ROC) curve of differential serum calcium (preoperative versus the concentration recorded on the first postoperative day) as a predictor of permanent hypoparathyroidism. Area under the curve 0.83 (0.87–0.8 with 95% confidence interval [95%CI]). Receiver operating characteristic (ROC) curve of differential serum calcium (preoperative versus the concentration recorded on the first postoperative day) as a predictor of permanent hypoparathyroidism. Area under the curve 0.83 (0.87–0.8 with 95% confidence interval [95%CI]).](https://static.elsevier.es/multimedia/25300180/0000006600000003/v1_201904190633/S2530018019300393/v1_201904190633/en/main.assets/thumbnail/gr3.jpeg?xkr=ue/ImdikoIMrsJoerZ+w96p5LBcBpyJTqfwgorxm+Ow=)
