Endocrinology and Nutrition is a medical specialty covering the study and treatment of diseases of the endocrine system, metabolism and those derived from the nutritional process, including knowledge of diagnostic techniques and dietary and therapeutic measures. In order to develop these activities and plan the management of resources allocated for this purpose, the so-called Portfolio of Services of the specialty has to be defined. A Portfolio of Services is defined as the set of techniques, technologies or procedures through which care services are provided in a healthcare centre, department or institution. It is an essential tool for organization of a hospital Unit or Department by defining the roles and procedures of its healthcare professionals, and also for structuring the resources required to perform the activity. It also allows for defining how to use these resources and identifying the objectives to be achieved, improving the quality of clinical care. Finally, the definition and preparation of the portfolio of services makes it possible to have an inventory of the offer of healthcare services and to detect new healthcare needs.
La Endocrinología y Nutrición es una especialidad médica que abarca el estudio y tratamiento de las enfermedades del sistema endocrino, del metabolismo y las derivadas del proceso nutricional, incluyendo el conocimiento de sus técnicas diagnósticas y medidas dietéticas y terapéuticas. Para desarrollar estas actividades y planificar la gestión de los recursos destinados a este fin, se requiere definir la denominada Cartera de Servicios de la especialidad. Se denomina Cartera de Servicios al conjunto de técnicas, tecnologías o procedimientos, mediante los que se hacen efectivas las prestaciones sanitarias de un centro, servicio o establecimiento sanitario. Es una herramienta fundamental para la organización de una Unidad o Servicio hospitalario al delimitar las funciones y procedimientos de sus profesionales sanitarios, así como para estructurar los recursos que se precisan para la realización de la actividad. Igualmente permite definir cómo utilizar estos recursos e identificar los objetivos a alcanzar, mejorando la calidad de la asistencia clínica. Finalmente, la definición y elaboración de la cartera de servicios posibilita disponer de un inventario de la oferta de servicios asistenciales y detectar nuevas necesidades asistenciales.
The portfolio of services is the set of techniques, technologies or procedures through which care services are provided in a healthcare centre, department or facility. It is a fundamental tool for the organisation of a hospital unit or department, in order to define and distribute the work and to define the functions and procedures of the health professionals of the unit, as well as their interactions with the other hospital departments and the primary care teams. The definition and preparation of the portfolio of services enables us to have an inventory of what services on offer are carried out, and makes it possible to progressively adapt these over time and to detect new healthcare needs.1
The first Endocrinology and Nutrition portfolio of services was negotiated in 1997 by expert members of the Sociedad Española de Endocrinología y Nutrición (SEEN) [Spanish Society of Endocrinology and Nutrition] and the Instituto Nacional de la Salud (INSALUD) [National Institute of Health].2 Subsequently, in 2002, the Ministry of Health published the catalogue of specialised care techniques and procedures,3 among which were those corresponding to Endocrinology and Nutrition. Finally, in 2011 an update of the Portfolio of Services in Endocrinology and Nutrition was published,4 this being the last publication by the ministry regarding this subject to date. However, in 2016 the SEEN produced a new update which was published on its website.5
Based on this latest 2016 update of the portfolio of services, the SEEN, with contributions from professionals from different autonomous Endocrinology and Nutrition societies, has updated it again, taking into account the changes and new additions that have occurred in the specialty over the past few years.
Definition of the specialty of Endocrinology and NutritionEndocrinology and Nutrition is a medical specialty that covers the study and treatment of diseases of the endocrine system, metabolism and those derived from the nutritional process, including theoretical and practical knowledge of the corresponding diagnostic techniques and dietary and therapeutic measures, as well as the promotion of health and the prevention of related diseases in these fields.
Its sphere of activity includes:
- none–
Physiology and pathology of the endocrine system: functional alterations in hormonal production, anatomical, structural or tumoural abnormalities of all endocrine glands.
- none–
Physiology and metabolic disease: study of metabolism and of the different essential nutrients, vitamins and trace elements.
- none–
Clinical nutrition: theoretical foundations of food and nutrition in healthy and ill subjects, and the development and application of oral, enteral and parenteral clinical nutrition.
- none–
Diagnostic and therapeutic procedures and techniques: knowledge and application of the different methods and techniques necessary for the diagnosis and treatment of the diseases that this specialty covers.
- none–
Study of the epidemiological, preventive, rehabilitative and genetic counselling aspects related to the processes dealt with by Endocrinology and Nutrition.
The index of processes that correspond to the specialty of Endocrinology and Nutrition classified according to ICD-10 corresponds to codes E00-E89 (Endocrine, nutritional and metabolic diseases), C73-C75 (Malignant neoplasms of thyroid and other endocrine glands), D34 -D35 (Benign neoplasm of thyroid gland and other endocrine glands), C7A (Malignant neuroendocrine tumours) and D3A (Benign neuroendocrine tumours) and can be consulted at https://eciemaps.mscbs.gob.es/ecieMaps/browser/index_10_mc.html.6
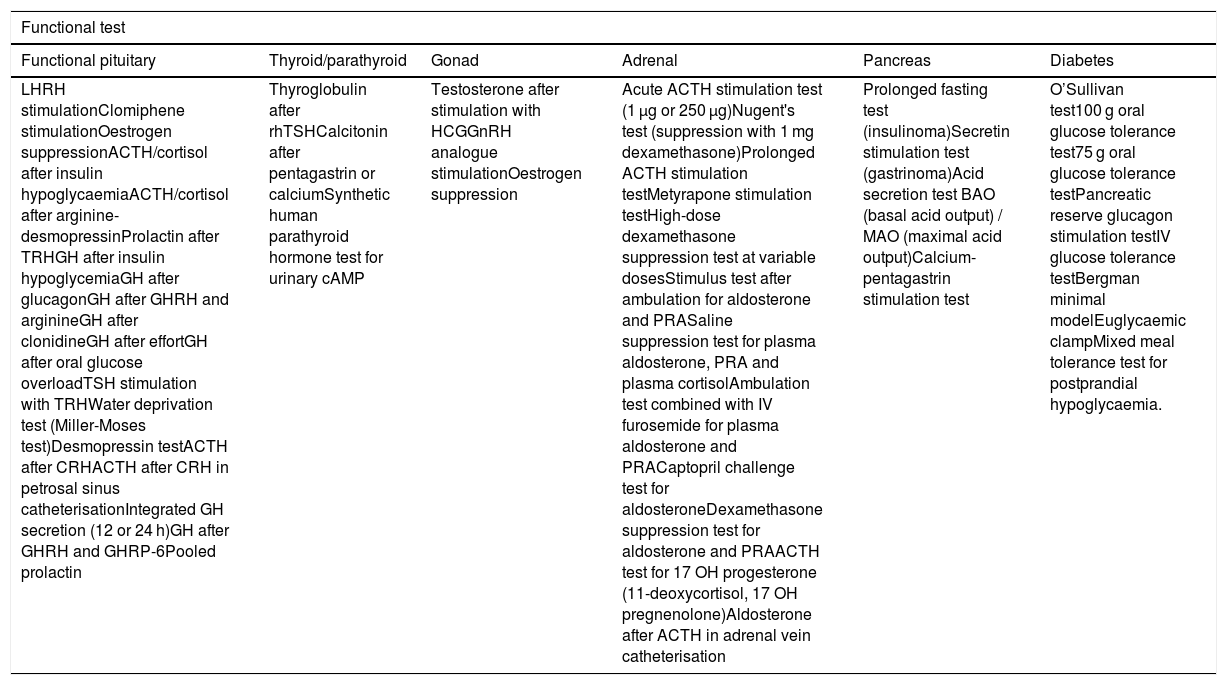
The index of diagnostic and therapeutic procedures and techniques that correspond to the specialty of Endocrinology and Nutrition is shown in Table 1.
Diagnostic procedures and techniques in Endocrinology and Nutrition.
| Functional test | |||||
|---|---|---|---|---|---|
| Functional pituitary | Thyroid/parathyroid | Gonad | Adrenal | Pancreas | Diabetes |
| LHRH stimulationClomiphene stimulationOestrogen suppressionACTH/cortisol after insulin hypoglycaemiaACTH/cortisol after arginine-desmopressinProlactin after TRHGH after insulin hypoglycemiaGH after glucagonGH after GHRH and arginineGH after clonidineGH after effortGH after oral glucose overloadTSH stimulation with TRHWater deprivation test (Miller-Moses test)Desmopressin testACTH after CRHACTH after CRH in petrosal sinus catheterisationIntegrated GH secretion (12 or 24 h)GH after GHRH and GHRP-6Pooled prolactin | Thyroglobulin after rhTSHCalcitonin after pentagastrin or calciumSynthetic human parathyroid hormone test for urinary cAMP | Testosterone after stimulation with HCGGnRH analogue stimulationOestrogen suppression | Acute ACTH stimulation test (1 μg or 250 μg)Nugent's test (suppression with 1 mg dexamethasone)Prolonged ACTH stimulation testMetyrapone stimulation testHigh-dose dexamethasone suppression test at variable dosesStimulus test after ambulation for aldosterone and PRASaline suppression test for plasma aldosterone, PRA and plasma cortisolAmbulation test combined with IV furosemide for plasma aldosterone and PRACaptopril challenge test for aldosteroneDexamethasone suppression test for aldosterone and PRAACTH test for 17 OH progesterone (11-deoxycortisol, 17 OH pregnenolone)Aldosterone after ACTH in adrenal vein catheterisation | Prolonged fasting test (insulinoma)Secretin stimulation test (gastrinoma)Acid secretion test BAO (basal acid output) / MAO (maximal acid output)Calcium-pentagastrin stimulation test | O’Sullivan test100 g oral glucose tolerance test75 g oral glucose tolerance testPancreatic reserve glucagon stimulation testIV glucose tolerance testBergman minimal modelEuglycaemic clampMixed meal tolerance test for postprandial hypoglycaemia. |
| Nutritional status assessment |
|---|
| Nutritional screening questionnaires: MNA, MUST, NRS-2002, VGS and others |
| Dietary history |
| Semi-quantitative questionnaires for nutrition survey |
| 24 -h dietary recall for nutrition survey |
| Food frequency questionnaire |
| Diet diary |
| Computer programs for preparing diets and evaluating dietary records/diaries |
| Photo album for portion size estimation |
| Anthropometry and functionality |
| Assessment of body composition using anthropometry, bioimpedance, DEXA or other techniques |
| Determination of muscle mass and adipose tissue by ultrasound |
| Assessment of muscle function using dynamometry or other techniques |
| Evaluation of energy expenditure by calorimetry |
| Assessment of dysphagia |
| Structured questionnaires |
| Method of clinical volume-viscosity (MECV-V) |
| Endoscopic examination of swallowing |
| Fibreoptic endoscopic evaluation of swallowing |
| Diagnostic procedures |
|---|
| Cervical ultrasound: for the diagnosis of thyroid diseases, detection of adenopathies, parathyroid and vascular diseases |
| Fine needle aspiration of thyroid nodules and cervical lymphadenopathy |
| Echo Doppler for carotid intima-media thickness |
| Echo Doppler of lower extremities |
| Digital retinography |
| Continuous blood glucose monitoring systems |
| Continuous blood pressure monitoring systems |
| Vascular function study: ABI, arterial stiffness, pulse-wave |
| Somatic and autonomic neuropathy test |
| FibroScan |
| Calculation of requirements in patients who are candidates for artificial nutritional support |
| Indirect calorimetry |
| Computer programs/apps for estimating requirements |
| Procedures that use changes in temperature/accelerometry (arm-band) to estimate total energy expenditure |
| Therapeutic procedures |
|---|
| Treatment with continuous insulin ports |
| Diabetes education. Specific material |
| Enolisation of thyroid nodules, neoplastic remnants of thyroid carcinomas and cervical lymphadenopathy |
| Radiofrequency ablation of thyroid nodules |
| Laser, ultrasound or microwave ablation of thyroid nodules |
| Hospital and home artificial nutrition: peripheral and central parenteral and enteral |
| Placement, replacement and monitoring of all the material required for nutritional support |
| Telemedicine systems applied to diabetes mellitus care and nutritional support |
| Monitoring of the food distribution system in the hospital area |
|---|
| Coding of baseline and therapeutic hospital diets |
| Planning of baseline and therapeutic hospital diets |
| Centralised plating monitoring in the hospital kitchen |
| Control of the organoleptic characteristics of the hospital diet, including measurement of the viscosity necessary for dysphagia |
| Allergen control |
| Control of the acquisition, reception, storage, preparation and distribution of food |
| Bromatological tests |
| Microbiological tests |
Endocrinology and Nutrition care is framed within the organisation of Specialised Care in the Public Health System, so that each Endocrinology and Nutrition department is responsible for the care provided to the population of its Health District with regard to its specialty. The functions to be performed by the Endocrinology and Nutrition departments/units are as follows:
A. Care functionA.1. In the hospital areaEndocrinology and Nutrition in-hospital functionality is established with end-service and central-service characteristics, and includes:
- –
Care for patients admitted under the care of the Endocrinology and Nutrition department due to specialty processes.
- –
Cooperation with other hospital departments for patients admitted under their care who have endocrinological, metabolic and nutritional diseases, at the request of their attending doctor, and with special care for people with diabetes for which treatment protocols for glycaemic control will be developed, both during their hospital admission, as well as at discharge.
- –
Detection and therapeutic approach for patients with malnutrition related to disease: nutritional screening protocols and assessment of the nutritional status of patients admitted whether or not they receive a nutritional intervention.
- –
Prescription, monitoring and follow-up of patients with nutritional treatment (oral, enteral, parenteral) in the hospital.
- –
Creation of a Codified manual of hospital diets, under a continuous process of revision, which must include: a) planning of the baseline diet and optional menus at reasonable costs, in collaboration with the managing director; b) planning of therapeutic diets for each pathological process; c) preparation of special diets or specific menus outside of the diet code for those patients who require it; and d) design of diets and recommendations for out-of-hospital use.
- –
Follow-up for patients treated with special diets, collaborating with the therapeutic procedures indicated by the clinical department responsible for the patient.
- –
Authorising all modifications that may for any reason (clinical, supply difficulties, health emergencies) need to be introduced to any baseline or therapeutic diet.
- –
Planning of enteral and parenteral nutrition formulas in collaboration with the Pharmacy department.
- –
Management of approaches for the administration of artificial nutrition (venous and gastrointestinal approaches).
- –
Centralised control of the hospital centre's food distribution system. Preparation of the codified diet manual, planning of codified optional and therapeutic baseline diets including special diets. Control and supervision of compliance with the dietary code.
- –
Collaboration with the management of the hospitality area of the hospital through the technical specifications for the acquisition, reception, storage, preparation and distribution of food.
Patients who need treatment via diagnostic or treatment methods that require continuous medical or nursing care for a few hours, but not hospital admission, are treated in the day hospital.7 In the day hospital environment, the following services can be performed:
- –
Endocrine-metabolic functional tests.
- –
Continuous monitoring assessment of BP or glucose.
- –
Treatment of onset of type 1 and type 2 diabetes without ketoacidosis.
- –
Treatment of decompensated diabetes that does not require hospital admission.
- –
Gestational diabetes follow-up.
- –
Follow-up of patients in intensive treatment with insulin or with insulin pump.
- –
Assessment and treatment of diabetic foot.
- –
Screening for chronic complications of diabetes: mydriatic retinography, vascular study by lower extremity echo Doppler, assessment of diabetic neuropathy.
- –
Patients with unstable DM due to steroid use, chemotherapy or recent hospital discharge.
- –
Steroid (or monoclonal antibody) treatment for thyroid-associated ophthalmopathy.
- –
Percutaneous treatment by cervical ultrasound-guided enolisation, thermal ablation or ultrasound of thyroid nodules, and parathyroid disease and cervical lymphadenopathy.
- –
Assessment and treatment of acute decompensations of neuroendocrine, adrenal, thyroid or parathyroid disease, including patients who have had surgery.
- –
Functional metabolic-nutritional assessment: performance of functional, body composition and metabolic tests.
- –
Assessment of dysphagia.
- –
Home enteral or parenteral nutrition that requires hospital infrastructure (initiation of treatment, follow-up or management of complications).
- –
Replacement of ostomy tubes, placement and removal of nasogastric tubes, etc.
- –
Treatment of specific nutritional deficiencies (administration of intravenous iron, vitamins, trace elements, etc.).
- –
Follow-up of patients with eating disorders (ED) (ED day hospital).
- –
Treatment of decompensations of endocrinological diseases that do not require hospitalisation (adrenal insufficiency, fluid and electrolyte disorders, hyper and hypocalcaemia).
- –
Health education (individual or group) aimed at patients with metabolic and nutritional disorders, mainly DM, adrenal insufficiency, obesity and home artificial nutrition.
Hospital outpatient consultations are preferably carried out as monographic consultations whereby specific diseases are treated within the specialty of Endocrinology and Nutrition, as well as more complex diseases that require treatment by multidisciplinary teams with longer consultation times.
Although the number of monographic consultations will depend on the organisation and human resources of each hospital/health district, the following are recommended: a) Neuroendocrinology (pituitary tumours; neuroendocrine tumours); b) Thyroid cancer; c) High resolution thyroid nodule consultation; d) Type 1 DM; e) Diabetes and pregnancy; f) Type 2 DM with special therapeutic complexity or with associated comorbidity; g) Dyslipidaemia and vascular risk; h) Diabetic foot; i) Adrenal pathology; j) Pathology of calcium and bone metabolism, k) Infertility; l) Adult metabolic diseases unit; m) Morbid obesity and bariatric surgery; n) Eating disorders; o) Gender identity consultation; p) Home enteral and parenteral nutrition consultation; q) Dysphagia consultation, and r) ALS consultation.
As far as possible, these consultations should be part of multidisciplinary units dedicated to each pathology.
In these outpatient consultations, the following will be carried out: a) clinical history and physical examination; b) indication or performance of diagnostic tests and procedures; c) indication, application and follow-up of the treatments or therapeutic procedures that the patient requires; d) information about the diagnostic procedures performed and the treatments prescribed to facilitate their correct compliance ensuring continuity and safety of care, and e) drafting of follow-up or discharge reports.
Health education is part of the care for endocrinological patients, with health education consultations carried out and aimed at all patients assessed and followed up at outpatient clinics, with special attention to metabolic and nutritional disorders. Development of educational programmes at different levels:
- –
Specific education on the use of tubes, systems, access routes, type of administration and infusion pumps for enteral or parenteral nutrition.
- –
Education on the prevention of complications and resolution of problems at home derived from enteral and parenteral nutrition.
- –
Individual and group education (obesity, diabetes, bariatric surgery, cardiac rehabilitation).
These take place in the outpatient setting at outpatient clinics/specialist centres.
Their purpose is to: a) treat the less complex diseases of the specialty; b) manage the referral of patients to the hospital; c) bring Endocrinology and Nutrition closer to the environment of each patient; d) collaborate with prevention and education tasks in endocrine-metabolic and nutritional diseases, mainly the most prevalent ones, such as DM, obesity, dyslipidaemia, hypertension, osteoporosis, etc., and e) facilitate the connection with primary care.
To this last end, virtual consultations with a GP and other specialists will be encouraged.
Just as with hospital consultations, the following will be carried out: a) clinical history and physical examination; b) indication or performance of diagnostic tests and procedures; c) indication, application and follow-up of the treatments or therapeutic procedures that the patient requires; d) information on the diagnostic procedures performed and the treatments prescribed, and e) drafting of follow-up or discharge reports.
Group and individual educational programmes mainly aimed at patients with metabolic disease (diabetes and obesity) will also be carried out.
A 3.3. Teleconsultation in Endocrinology and NutritionThe increasing implementation of new technologies that facilitate remote communication, both with endocrinology patients and with other professionals involved in their care, allow clinical activity in Endocrinology and Nutrition to be carried out, in certain circumstances and under specific protocols, in a virtual way, via a conventional phone call, video call or specific platforms.
According to the Organización Médica Colegial [Collegiate Medical Organisation], this type of care is considered a medical action that supplements the face-to-face medical action, which can, in certain circumstances, substitute it.8 The different modalities of teleconsultation, the requirements that must be met in order for it to be carried out and its main indications in endocrinological and nutritional diseases are included in a specific document published by the SEEN.9
This type of care must be agreed upon by all those involved and a specific time, similar to that of face-to-face consultations, must be reserved in the consultation diary, in order for it to be carried out.
B. Teaching functionB.1. Undergraduate and postgraduate training in the medical areas of Endocrinology and Nutrition and Human Nutrition and Dietetics.
B.2. Training of resident doctors in the specialty of Endocrinology and Nutrition and other specialties (residents of Internal Medicine, Family and Community Medicine, Cardiology, Nephrology, Geriatrics, Gastroenterology, Hospital Pharmacy, etc.) from the hospital itself or from other hospitals in the National Health System Network.
B.3. Continuous training of the professionals of the section or department through organised clinical sessions, attendance at courses, conferences, etc.
B.4. Continuous training of healthcare personnel in the health district: training of primary care physicians in continuous training programmes and internal continuous training of the unit.
B.5. Professional training for the Degree in Dietetics. Collaboration in undergraduate training, nursing specialties (community nursing) and the Degree in Human Nutrition and Dietetics.
B.6. Collaboration with the associations of patients with diseases typical of the specialty in the training regarding their disease.
C. Management functionThe management of the Endocrinology and Nutrition departments, sections or units will be adapted to the structure of each centre, depending on the specificities of each autonomous community. The management of the activity, in all its areas, will cater to the total quality model, maximising efficiency. For this, the members of the Endocrinology and Nutrition departments, sections or units will commit to working with the management of the centre to:
- –
Define care, teaching, research and quality objectives and processes (activity, complexity of care, use of resources, expenditure per process, pharmaceutical expenditure, etc.).
- –
Define indicators in each of the areas of activity and their corresponding standards.
- –
Monitor compliance with the indicators.
- –
Define operating standards for the unit that integrates all its components.
- –
Organise multidisciplinary units/committees in collaboration with other specialties.
- –
Plan care and teaching activity.
- –
Coordinate with primary care: establishment of agreed criteria for continuity of care, implementation of common protocols for the diagnosis and treatment of very prevalent diseases (obesity, hyperlipidaemia, thyroid dysfunction, type 2 DM and osteoporosis), establish the figure of "consultant specialist" and carry out training courses aimed at primary care professionals.
- –
Develop telecare programmes.
- –
Coordinate with other specialties.
- –
Participate in programmes for the care of chronic patients.
- –
Control spending and cost-effectiveness and sustainability of the department/unit budget (if any).
- –
Control quality. Establish indicators, look for areas for improvement and evaluate their degree of compliance.
- –
Promote and participate in improvement groups. Promote the certification of units/departments following standards such as ISO 9001:2015, EFQM, UNE (179009: 2018).
- –
Participate in hospital clinical committees, especially in the Tumours Committee and in the Nutrition Committee (which should be led by a doctor specialising in Endocrinology and Nutrition), as well as the Food Committee, the Pharmacy Committee, the Clinical Trials Committee, the Research Committee, the Teaching/Continuing Education Committee, the Bioethics Committee and the New Technologies Committee.
- –
Collaborate with scientific societies in the creation of national registries for endocrine-metabolic diseases.
- –
Collaborate with professional colleges and universities.
- –
Collaborate with associations of patients with endocrinological or nutritional diseases.
- –
Clinical research associated with healthcare practice.
- –
Epidemiological studies in relation to endocrinological and nutritional topics.
- –
Participation in clinical trials for Endocrinology and Nutrition and translational research.
- –
Participation in public health campaigns mainly related to endocrinological and nutritional diseases.
Once the functions of the Endocrinology and Nutrition departments have been established, it is necessary to establish the human and material resources required to provide effective, efficient and quality services.
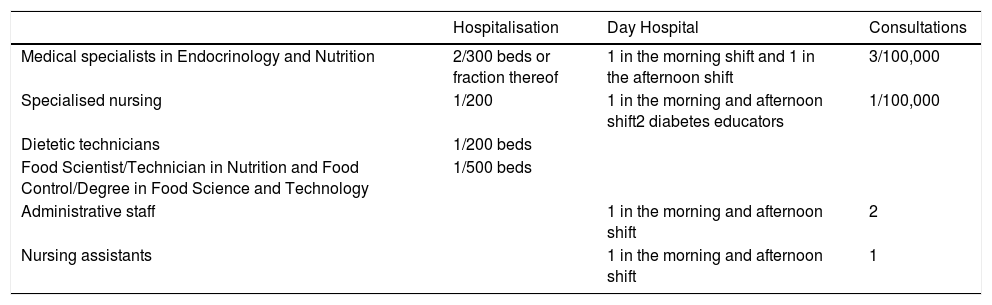
The human resources necessary to provide effective, efficient and quality care in an Endocrinology and Nutrition department/unit are summarised in Table 2.
Human resources needed in an Endocrinology and Nutrition department/unit.
| Hospitalisation | Day Hospital | Consultations | |
|---|---|---|---|
| Medical specialists in Endocrinology and Nutrition | 2/300 beds or fraction thereof | 1 in the morning shift and 1 in the afternoon shift | 3/100,000 |
| Specialised nursing | 1/200 | 1 in the morning and afternoon shift2 diabetes educators | 1/100,000 |
| Dietetic technicians | 1/200 beds | ||
| Food Scientist/Technician in Nutrition and Food Control/Degree in Food Science and Technology | 1/500 beds | ||
| Administrative staff | 1 in the morning and afternoon shift | 2 | |
| Nursing assistants | 1 in the morning and afternoon shift | 1 |
The Endocrinology and Nutrition specialist is responsible for supporting all the processes listed in Annex 1 and performing the previously described procedures.
The study carried out by the SEEN in 1997 and the surveys subsequently carried out at the request of the Comisión Asistencial de la SEEN (CASEEN) [SEEN Healthcare Commission] in 1999, 2003 and 200610,11 estimated that to cover the functions of an Endocrinology and Nutrition department/unit (care, teaching, research and management), both in the hospital and outpatient settings, the following are necessary:
- 1
A minimum of three physicians specialising in Endocrinology and Nutrition to provide outpatient care for every 100,000 inhabitants.
- 2
Two specialists in Endocrinology and Nutrition for hospital care for every 300 beds.
Additionally, it is recommended that there be an endocrinologist within 100 km of any inhabitant. These needs are established for all types of hospitals, including referral hospitals, area hospitals and regional hospitals.
In 2019, the Ministry of Health published a document according to which the rate of specialists in Endocrinology and Nutrition in the public sector was 2.59/100,000 inhabitants, although with a very irregular distribution in the different autonomous communities, and in the projections made, it was determined that the needs in the specialty will remain the same or increase to the year 2030.12
Specialised nursingIt is essential that specialised nursing exists in order to develop the specialty and cover the entire spectrum of health education, which is so important in our field, especially in matters of diabetes education, clinical nutrition and diet therapy. The high level of specialisation required by this type of nursing means it is necessary to stabilise these professionals within the units/departments.
Specialised nursing in the area of diabetes is the main feature in the care of patients with DM, and must be present both at the hospital level and in external consultations.
One outpatient diabetes educator is recommended for every 100,000 inhabitants and one for every 200 hospital beds. The functions of the diabetes educator are:
- –
Hospitalisation: diabetes education for the patient with onset of diabetes, re-education of the person with diabetes who is admitted due to a decompensation, training for the patient after a change in treatment, such as the initiation of insulinisation, planning at discharge and follow-up, coordination with a consultant educator or primary care nurse, developing consensual educational protocols and programmes in the area to train people with diabetes in the knowledge and management of their disease at various levels.13
- –
Outpatient consultation: knowledge and skills training for the person with diabetes, education in the implantation of an insulin pump and a continuous glucose monitor. Follow-up of the diabetic patient via face-to-face or telehealth consultation. Coordination with the medical team, hospital educator and primary care nurse in care and follow-up.
Nursing staff with knowledge in the area of nutrition is important for proper nutritional assistance. One nurse is recommended for every 200 hospital beds and one outpatient nurse for every 100,000 inhabitants. The functions to be performed will include:
- –
During hospitalisation: data collection derived from nutritional screening, initial nutritional assessment at hospital admission - nutritional history, assessment of oral intake, body composition studies and assessment of energy expenditure, functional tests (dynamometry, evaluation of dysphagia at the bedside) and monitoring of specialised nutritional support - oral nutritional supplements, enteral nutrition and parenteral nutrition.
- –
Outpatient consultation: health education for adapting natural and artificial nutrition for patients with malnutrition related to disease, obesity, eating disorders, errors of metabolism, etc. Placement and replacement of nasogastric and gastrostomy tubes, and performance of anthropometric and other nutritional tests.
The profession of dietitian-nutritionist, despite having regulated undergraduate studies and being recognised in Spain as a health profession, is a minority profession in the public health system. At the present time, according to the RECALSEEN13 study, they are present in 54% of hospitals with more than 500 beds and in 48% of those with less than 500 beds. From the SEEN, we would like to recommend and request their full inclusion in Clinical Nutrition and Dietetics units.
It is advisable to have one for every 200 hospital beds, assigned to the Endocrinology and Nutrition department/unit, with the following basic functions:
- –
Collaborate in adapting the food systems established in each centre and in preparing the manual or code of hospital diets.
- –
Design, create and monitor special or personalised diets at the request of the specialist in Endocrinology and Nutrition of the Clinical Nutrition Unit.
- –
Contribute to the development of informational-educational dietary, preventive or therapeutic programmes.
- –
Contribute to the prevention of hospital malnutrition by assessing nutritional status, within the multidisciplinary team.
- –
Participate in the coordination and relationship of the Endocrinology and Nutrition department/unit with the Food/Hospitality department and hospital administration.
- –
Supervise the functions of dietetic technicians.
Their functions would be:
- –
Serve as a liaison in the coordination and relationship of the Endocrinology and Nutrition department/unit with the Food/Hospitality department and hospital administration.
- –
Collaborate in the adaptation of the food systems established in each centre and in the preparation of the manual or code of hospital diets.
- –
Develop informational-educational dietary, preventive or therapeutic programmes.
- –
Contribute to the prevention of hospital malnutrition, by assessing nutritional status.
In charge of food safety through the correct application and evaluation of the Análisis de Peligros y Puntos de Control Críticos (APPCC) [Hazard Analysis and Critical Control Points] system14 with all the functions defined for this. In the event of a foodborne illness, this person will collaborate with the Preventive Medicine department in the investigation and control of the outbreak. Following our previous recommendations, we believe it is advisable to have one for every 500 hospital beds or fraction thereof.
Other professionals: podiatrist, clinical psychologist, speech therapist, physical educatorThere are a number of professionals who are going to be necessary to carry out adequate care in the Endocrinology and Nutrition units, and their assignment to these units is recommended, although not essential, especially in highly complex tertiary hospitals. Their part-time collaboration or contribution within the scope of multidisciplinary units will be very valuable. These would be: podiatrist in the prevention of diabetic foot, speech therapist in the context of dysphagia care, clinical psychologist in the care of DM, obesity and oncological diseases of the specialty. Physical educator in the care of obesity, sarcopaenia, ageing, etc.
Administrative staffTheir presence is particularly necessary for the management of appointments, telephone assistance and all the administrative work of the department/unit.
Nursing assistantsTheir presence in consultations is required to support the specialist, to weigh and measure the patient's height, take the BP, measure the waist, take care of, maintain and request the necessary material for the proper functioning of the consultations.
Material resourcesGiven that hospital activity in the field of Endocrinology and Nutrition covers hospitalisation, day hospital, emergency and outpatient clinics, the following are essential:
- –
Hospital beds. The number of beds required is around 1% of hospital beds. However, in the latest survey conducted by the CASEEN11 the data reflect the importance of outpatient care in our specialty, with the number of beds assigned to Endocrinology and Nutrition only 0.58% of the total hospital beds. The opening of day hospitals for Endocrinology and Nutrition, by improving outpatient control of endocrine-nutritional diseases, with the consequent reduction in acute decompensations, has meant that, at least in part, the percentage of real hospital beds is lower than that calculated to meet the needs.
- –
Hospital offices. At least one office in the hospital ward.
- –
Multi-purpose classrooms. For diabetes education and clinical nutrition.
- –
Physical space for day hospital.
- o
It is estimated that the number of places (beds or chairs) necessary to cover the care demand of patients who require hospitalisation during the day would be between two and six.
- o
Physical space for carrying out metabolic and nutritional functional tests (calorimetry, body composition techniques, etc.)
- o
Physical space for performing endocrinological functional tests.
- o
Physical space for carrying out the planned treatments at the day hospital.
- o
Warehouse.
- o
- none–
Physical space for Nutrition and Dietetics:
- o
Clean physical space, dirty physical space and physical storage space depending on Clinical Nutrition and Diet, clearly differentiated for the preparation of enteral nutrition prescriptions. A sink, worktop, dishwasher, metal shelves, refrigerator, work table (consultation or office type), chairs and office shelves will be distributed across the different spaces.
- o
Office located next to the Kitchen Service units, depending on Clinical Nutrition and Dietetics, for kitchen dietitians or dietetic technicians to carry out their previously mentioned dietary control activity.
- o
Laminar flow hood area, dependent on the Pharmacy Service, for the preparation of parenteral nutrition mixtures.
- o
- none–
Physical space for outpatient hospital consultations:
- o
At least one physical space of 12 m2 for every 50,000 inhabitants.
- o
At least one physical space for a nurse educator.
- o
Patient waiting room
- o
Consultation times for patients seen in the outpatient clinic at the hospital: 30 min for new consultations and 20 min for follow-up consultations. For certain highly complex monographic consultations, these times can be extended.
- o
- none–
Physical space for out-of-hospital outpatient visits:
- o
At least one clinic for every 50,000 inhabitants or fraction thereof. Minimum space 12 m2.
- o
At least one clinic for diabetes education.
- o
Patient waiting room.
- o
Consulting time: 20 min for new consultations and 15 min for follow-up consultations.
- o
- none–
Diagnostic and therapeutic examinations area. Space to perform minimally invasive techniques (enolisations, laser ablation, radiofrequency or ultrasound) and techniques for assessing body composition and muscle function.
- none–
Physical space in non-healthcare area. The departments and units must have non-care space where the office of the head of department, individual offices for section heads and senior deputies, and common work rooms for deputies, residents and interns are located. Additionally, there must be a meeting room where clinical sessions and internal department meetings can be held, with audiovisual support for them and for videoconferences, as well as an office for the secretary and a space for materials storage.
- none–
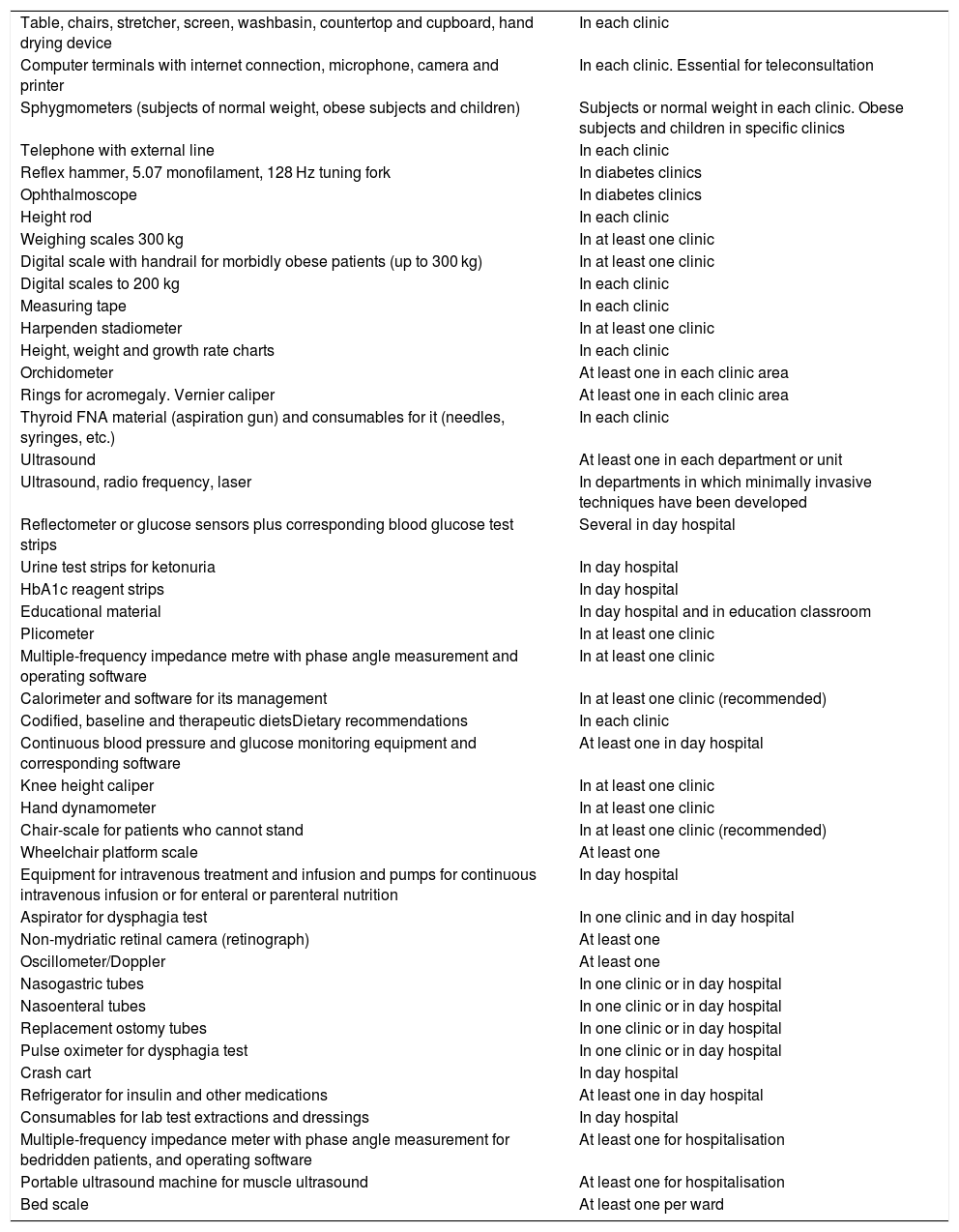
Equipment. The equipment requirements for Endocrinology and Nutrition hospital consultations and the Endocrinology and Nutrition day hospital, as well as additional equipment in the hospitalisation area, are shown in Table 3.
Table 3.Equipment needed in clinics and in the Endocrinology and Nutrition day hospital.
Table, chairs, stretcher, screen, washbasin, countertop and cupboard, hand drying device In each clinic Computer terminals with internet connection, microphone, camera and printer In each clinic. Essential for teleconsultation Sphygmometers (subjects of normal weight, obese subjects and children) Subjects or normal weight in each clinic. Obese subjects and children in specific clinics Telephone with external line In each clinic Reflex hammer, 5.07 monofilament, 128 Hz tuning fork In diabetes clinics Ophthalmoscope In diabetes clinics Height rod In each clinic Weighing scales 300 kg In at least one clinic Digital scale with handrail for morbidly obese patients (up to 300 kg) In at least one clinic Digital scales to 200 kg In each clinic Measuring tape In each clinic Harpenden stadiometer In at least one clinic Height, weight and growth rate charts In each clinic Orchidometer At least one in each clinic area Rings for acromegaly. Vernier caliper At least one in each clinic area Thyroid FNA material (aspiration gun) and consumables for it (needles, syringes, etc.) In each clinic Ultrasound At least one in each department or unit Ultrasound, radio frequency, laser In departments in which minimally invasive techniques have been developed Reflectometer or glucose sensors plus corresponding blood glucose test strips Several in day hospital Urine test strips for ketonuria In day hospital HbA1c reagent strips In day hospital Educational material In day hospital and in education classroom Plicometer In at least one clinic Multiple-frequency impedance metre with phase angle measurement and operating software In at least one clinic Calorimeter and software for its management In at least one clinic (recommended) Codified, baseline and therapeutic dietsDietary recommendations In each clinic Continuous blood pressure and glucose monitoring equipment and corresponding software At least one in day hospital Knee height caliper In at least one clinic Hand dynamometer In at least one clinic Chair-scale for patients who cannot stand In at least one clinic (recommended) Wheelchair platform scale At least one Equipment for intravenous treatment and infusion and pumps for continuous intravenous infusion or for enteral or parenteral nutrition In day hospital Aspirator for dysphagia test In one clinic and in day hospital Non-mydriatic retinal camera (retinograph) At least one Oscillometer/Doppler At least one Nasogastric tubes In one clinic or in day hospital Nasoenteral tubes In one clinic or in day hospital Replacement ostomy tubes In one clinic or in day hospital Pulse oximeter for dysphagia test In one clinic or in day hospital Crash cart In day hospital Refrigerator for insulin and other medications At least one in day hospital Consumables for lab test extractions and dressings In day hospital Multiple-frequency impedance meter with phase angle measurement for bedridden patients, and operating software At least one for hospitalisation Portable ultrasound machine for muscle ultrasound At least one for hospitalisation Bed scale At least one per ward
The authors declare that they have no conflicts of interest.
Please cite this article as: Sandi JS, González EN, Ruiz AH, Nivela OB, Pomar MB, Martín FJES, et al. Cartera de servicios en Endocrinología y Nutrición. Actualización 2020. Endocrinol Diabetes Nutr. 2021;68:577–588.