Disease-related malnutrition (DRM) is underdiagnosed and underreported despite its well-known association with a worse prognosis. The emergence of big data and the application of artificial intelligence in medicine have revolutionized the way knowledge is generated. The aim of this study is to assess whether a big data tool could help us detect the amount of DRM in our hospital.
MethodologyThis was a descriptive, retrospective study using the Savana Manager® tool, which allows for automatically analyzing and extracting the relevant clinical information contained in the free text of the electronic medical record. A search was performed using the term “malnutrition”, comparing the characteristics of patients with DRM to the population of hospitalized patients between January 2012 and December 2017.
ResultsAmong the 180,279 hospitalization records with a discharge report in that period, only 4446 episodes (2.47%) included the diagnosis of malnutrition. The mean age of patients with DRM was 75 years (SD 16), as compared to 59 years (SD 25) for the overall population. There were no sex differences (51% male). In-hospital death occurred in 7.08% of patients with DRM and 2.98% in the overall group. Mean stay was longer in patients with DRM (8 vs. 5 days, p<0.0001) and there were no significant differences in the 72-h readmission rate. The most common diagnoses associated with DRM were heart failure (35%), respiratory infection (23%), urinary infection (20%), and chronic kidney disease (15%).
ConclusionUnderdiagnosis of DRM remains a problem. Savana Manager® helps us to better understand the profile of these patients.
La desnutrición relacionada con la enfermedad (DRE) está infradiagnosticada e infrarreportada, a pesar de su asociación con un peor pronóstico. La irrupción del big data y la inteligencia artificial aplicada en medicina ha revolucionado la forma de generar conocimiento. El presente estudio tiene como objetivo valorar si una herramienta de big data podría ayudarnos a detectar y conocer la DRE en nuestro hospital.
MetodologíaEstudio retrospectivo descriptivo, utilizando la herramienta Savana Manager®, que permite analizar y extraer de forma automática la información clínica relevante contenida en el texto libre de la historia clínica electrónica. Se realiza una búsqueda con el término «desnutrición», comparando las características de los pacientes con DRE frente a la población de pacientes hospitalizados en el periodo comprendido entre enero de 2012 y diciembre de 2017.
ResultadosDe 180.279 registros de hospitalización con informe de alta en dicho periodo, solo 4.446 episodios (2,47%) incluían el diagnóstico de desnutrición. La edad media de los pacientes con DRE fue 75 años (DE 16) frente a 59 (DE 25) años de la población global. No hubo diferencias en género (51% varones). El fallecimiento intrahospitalario se produjo en el 7,08% de los pacientes con DRE frente al 2,98% en el grupo general. La estancia mediana fue superior en los pacientes con DRE (8 vs. 5 días, p<0,0001) y no hubo diferencias significativas en la tasa de reingresos a 72horas. Los diagnósticos más frecuentes asociados a DRE fueron insuficiencia cardíaca (35%), infección respiratoria (23%), infección urinaria (20%) y enfermedad renal crónica (15%).
ConclusiónEl infradiagnóstico de la DRE sigue siendo un problema. Savana Manager® ayuda a conocer mejor el perfil de estos pacientes.
Disease-related malnutrition (DRM) is underdiagnosed and underreported, despite the fact that its correlation to a poorer patient prognosis is well known. In Spain, data from the national PREDYCES study indicated that 23.7% of all people admitted to hospital were at risk of DRM. Disease-related malnutrition was associated with increased hospital stay and costs, particularly in those patients who suffered a worsening of their nutritional status during their hospital stay.1
The economic impact of DRM is very important, the potential cost of the problem in Spain being estimated to exceed 1100 million euros a year.2 Despite these data and the efforts of scientific bodies in the context of the “más nutridos” (“more nourished”) alliance (https://www.alianzamasnutridos.es/) to achieve zero malnutrition in the Spanish National Health System, DRM remains a rarely diagnosed entity.
Medicine is currently changing, as are many other disciplines, with the emergence of big data (BD) and artificial intelligence. Both concepts have revolutionized the way knowledge is generated through the coincidence of two phenomena: the exponential accumulation of data and the computation capacity to process data.3 Due to its volume and availability, the electronic health record (EHR) is the largest big data source in healthcare today. In this context, the present study aims to determine whether a big data tool can help detect and be aware of DRM in our hospital.
MethodologyA retrospective, observational non-interventional study was conducted using the Savana Manager® clinical platform. This tool reuses data from the EHRs of Hospital Universitario de León (León, Spain).
Savana Manager®, using EHRead technology, is an innovative system able to automatically analyze and extract the relevant clinical information contained in the free text of EHRs using natural language processing (NLP) and BD processing techniques, and to transform it into ordered information for research purposes.4
The present study was carried out after a retrospective search through Savana Manager® of the hospital discharge reports, using the search term “malnutrition”. We then compared the characteristics of patients with DRM versus hospitalized patients without DRM, corresponding to the period between January 2012 and December 2017.
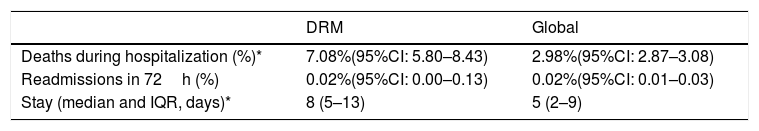
The results referring to in-hospital deaths and readmissions after 72h are presented in table form with percentages, medians and the respective 95% confidence interval (95%CI). In order to identify possible statistically significant differences between groups, we calculated the 95%CI for the difference of two proportions of independent samples, a statistically significant difference being considered to exist when the interval did not contain 0. Since hospital stay is a variable with a non-normal distribution, it was recorded as the median (interquartile range [IQR]), the observed outliers above 1.5 days of percentile 75 and below 1.5 days of percentile 25 of the distribution being excluded. Comparisons were made using the nonparametric Mann–Whitney U-test.
ResultsOut of 180,279 hospitalization records with a discharge report in that period, 4446 episodes (2.47%), corresponding to 1453 patients (1.4% of all patients hospitalized in that period) included the diagnosis of DRM in the hospitalization report. During the same period, the nutrition unit attended 2.3% of the admissions (unpublished proprietary data from the ‘Annual report of the clinical nutrition and dietetic unit’).
The mean age of the patients with DRM was 75 years (standard deviation [SD] 16) versus 59 years (SD 25) for the global hospital population. No gender differences were observed (51% males). The in-hospital mortality rate was 7.08% (95%CI: 5.80–8.43) among the patients with DRM versus 2.98% (95%CI: 2.87–3.08) in the general group (95%CI of the difference 2.78–5.42; p<0.0001). The mean stay was longer in the patients with DRM (p<0.0001), and there were no significant differences in the readmissions rate at 72h (Table 1) or in late readmissions (between 8 and 30 days, 24.6% in patients with DRM vs. 28.2% in the rest of the population; p=0.421), though a difference was noted in the readmission rate in the first week after discharge (3.5% in patients with DRM vs. 11.3% in the rest of the population; p=0.014).
Hospital indicators in relation to the presence of DRM versus the general group of hospitalized patients.
The diagnoses most commonly associated with those patients who according to the clinical history had presented malnutrition at some time or other were heart failure (35% vs. 12% in the global patients), respiratory infection (23% vs. 7%), urinary infection (20% vs. 5%) and chronic kidney disease (15% vs. 4%). As regards cardiovascular risk factors, patients with DRM more often presented arterial hypertension (61% vs. 38%), diabetes (34% vs. 20%), dyslipidemia (32% vs. 16%) and smoking (16% vs. 9%).
DiscussionDisease-related malnutrition remains an underdiagnosed entity in our hospitals, despite its impact and the related healthcare costs. In a study conducted in our own department of Internal Medicine,5 the prevalence of DRM upon admission was 26.9%, though 18% of the patients with good initial nutritional status also developed malnutrition during their hospital stay.
Since approximately 2.3% of all hospitalized patients are seen in our unit, our prevalence data referring to DRM suggest that we should detect such malnutrition in a much larger number of hospitalized patients. Since Savana Manager® detected the diagnosis of DRM in 2.47% of all hospitalization episodes, it can be affirmed that our unit is dealing with practically all the patients with DRM, though the number remains far from optimum. We are probably only dealing with the most severe cases, in which the diagnosis of DRM is most evident and attracts the attention of the physicians. This means that a considerable number of patients are neither assessed nor treated, despite the fact that simple and low-cost measures such as dietetic and clinical interventions could result in patient improvement and potential cost savings.
The Savana Manager® affords a better understanding of the profile of patients with DRM, and confirms that the latter is associated with older patients and implies a higher mortality rate and a longer mean stay, as was also recorded in the PREDYCES study1 and in our previous study. Patients who experienced a worsening of their nutritional status during admission presented a significant 2.5-day prolongation of stay, for the same comorbidity.5 The Savana Manager® also shows an increase in stay from 5 to 8 days. The very early (<72h) and late (8–30 days) readmission rates were similar in patients with and without DRM, though, curiously, patients with DRM had fewer admissions in the first week after discharge. The higher mortality rate and longer mean hospital stay may have played a role in this apparently discordant observation.
In addition, the findings of our study have allowed us to become aware of the conditions most commonly associated with DRM in our patients. Heart failure was the most frequently associated condition, thus confirming current evidence regarding the high prevalence of DRM in patients with this cardiac disease.6
The underdiagnosis of DRM is not only seen in our setting. A recent study in Switzerland7 established that DRM was present in 0.32% of all hospitalization episodes in 1998, and increased to 3.97% in 2014. This study also found an association between the diagnosis of DRM and increased mortality, mean stay and complications. Training and enhanced awareness is therefore still required among the healthcare professionals regarding the importance of detecting and treating DRM, based on both healthcare management and clinical criteria.
The patients who develop DRM in our hospital generate an excess cost of 767€ per admission (+35%), which in turn implies an excess cost related to malnutrition of 646,419.93€ a year in a department of Internal Medicine. On the other hand, adequate coding of the malnutrition diagnoses, and the procedures used to revert the malnutrition in the patients included in our previous studies,5,8 have resulted in an increase in weight of the diagnosis-related group (DRG) in the studied hospitalization unit from 130.92 to 174.4 points, which implies a mean weight increment of from 2.11 to 2.81.
With regard to the clinical impact of adequate detection and treatment, recent data from the EFFORT study,9 a randomized clinical trial in over 2000 patients, have shown intensive nutritional management during the hospital stay to result in a 21% decrease in serious adverse effects during admission, including mortality, Intensive Care Unit admissions, 30-day readmissions, major complications and functional impairment (adjusted odds ratio [OR] 0.79 [95%CI: 0.64–0.97]; p=0.023), as well as a 35% decrease in mortality (OR 0.65 [0.47–0.91]; p=0.011). Thus, the detection of DRM and an adequate approach to the problem are increasingly seen to be necessary in our hospitals.
One of the limitations of our study is the source of the data analyzed. Registries in the form of hospital discharge reports have been used, since our hospital is currently in transition from paper format to electronic medical records. This means that we have not had access to variables such as body weight or weight loss in each hospitalization episode, because such information is rarely recorded in discharge reports. The universalization of electronic health records (EHRs), together with an increased awareness of the significance of these data, may allow for better understanding of DRM data in the future.
The use of big data tools and artificial intelligence, such as Savana Manager®, has allowed us to confirm the findings of previous studies, with less time being needed to obtain the different patient profiles. In this regard, it is an instrument that facilitates the evaluation of our population when we are establishing an initial diagnosis of the situation or assessing possible changes in patient profiles according to the impact of the adoption of organizational changes or new situations.
However, it must be taken into account that the reliability of the results of big data tools is strongly conditioned by adequate diagnostic coding and good clinical judgment. This limits the conclusions drawn, and specific studies are thus needed to confirm the findings obtained.
In sum, it can be concluded that the underdiagnosis of DRM remains a problem. Disease-related malnutrition occurs in elderly patients and is related to higher mortality rates and a longer hospital stay. Big data tools such as Savana Manager® can help us to better understand and evaluate the profile of the affected patients.
Conflicts of interestThe authors state that they have no conflicts of interest in relation to this study.
Thanks are due to the whole Savana team, in particular to Yolanda González, for logistic support in the conducting of this study.
Please cite this article as: Ballesteros Pomar MD, Pintor de la Maza B, Barajas Galindo D, Cano Rodríguez I. Persiguiendo la desnutrición relacionada con la enfermedad mediante herramientas de big data. Endocrinol Diabetes Nutr. 2020;67:224–227.
The data in this study were originally presented in verbal format at the 6 best communications of the 34th National Congress of the Spanish Society of Clinical Nutrition and Metabolism (SENPE), held in Santiago de Compostela (Spain), from 30 May to 1 June 2019.