Dyslipidemia is one of the main risk factors in cardiovascular disease in patients with diabetes mellitus type 2 (DM2). The aim of this study is to evaluate the prevalence and risk factors associated with dyslipidemia in the population with diabetes mellitus type 2 in the region of Cantabria.
Material and methodsThis is a transversal study carried out at Cantabrian primary health care centers (n=680). A representative, random sample of the population with DM2, ranging from 18 to 85, was selected using a multistage procedure. The medical records were obtained, and by means of interviews the data of the risk factors to be studied was secured. The correlation with dyslipidemia was analyzed by means of logistic regression.
ResultsThere were 52.1% of males, the average age was 69.8, the evolution of diabetes was 9.99 years, 84.3% had arterial hypertension, 76.6% were overweight or obese and the average HbA1c was 6.96%. The prevalence of dyslipidemia was 85.3%, and in the bivariate analysis this is associated with a history of peripheral artery disease, controlled diabetes, antihypertensive treatment, glomerular filtration, HbA1c >7%, body fat estimated as being either overweight or obese, a history of cardiovascular disease, age and HbA1c.
In the multivariate analysis the independent factors were being female and a history of cardiovascular disease.
ConclusionThe prevalence of dyslipidemia in our study was 85.3%, and is consistent with figures found in previous published studies. The independent associated risk factors were being female and a past medical history of cardiovascular disease.
La dislipidemia es uno de los principales factores de riesgo de enfermedad cardiovascular en pacientes con diabetes mellitus tipo 2 (DM2). El objetivo de este estudio es evaluar la prevalencia y factores de riesgo asociados a la dislipidemia en la población con DM2 de la Comunidad de Cantabria.
Material y métodosEs un estudio transversal realizado en centros de Atención Primaria del Servicio Cántabro de Salud (n = 680). Se seleccionó una muestra aleatorizada representativa de la población con DM2 de 18 a 85 años mediante un procedimiento polietápico. Se obtuvieron de la historia clínica y mediante entrevista los datos de los factores de riesgo a estudio. Se analizó la asociación con la dislipidemia mediante regresión logística.
ResultadosEl 52,1% eran hombres, la edad media fue de 69,8 años, la evolución de la diabetes de 9,99 años, el 84,3% tenían HTA, el 76,6% sobrepeso/obesidad y la HbA1c media era de 6,96%. La prevalencia de dislipidemia fue del 85,3% y en el análisis bivariado se asoció con antecedente de enfermedad vascular periférica, diabetes controlada, tratamiento antihipertensivo, filtrado glomerular, HbA1c > 7%, grasa corporal estimada en sobrepeso y obesidad, antecedente de enfermedad cardiovascular, edad y HbA1c.
En el análisis multivariante los factores independientes fueron el sexo femenino y el antecedente de enfermedad cardiovascular.
ConclusionesLa prevalencia de dislipidemia en nuestro estudio fue del 85,3% y es consistente con la encontrada en estudios previos publicados. Los factores de riesgo asociados de forma independiente fueron el sexo femenino y el antecedente personal de enfermedad cardiovascular.
Type 2 diabetes mellitus (T2DM) has become a pandemic due to increased life expectancy, resulting in an aging population, increased obesity and non-heart healthy lifestyle changes (lack of physical exercise and bad eating habits).1
According to the di@bet.es study, the prevalence of T2DM is 13.79% in the Spanish adult population.2
According to data from the World Health Organization (WHO) (2016), diabetes is one of the most common causes of death in Spain. The proportional mortality attributable to the disease is 3% of total deaths for all age groups.3
Diabetes mellitus has significant socioeconomic costs. Crespo et al. reported the annual cost of T2DM in 2013 to be 5890 million euros, representing 8.2% of total healthcare expenditure.4
In patients with diabetes, macrovascular complications are the leading cause of morbidity and mortality worldwide. Approximately 75% die from heart or cerebrovascular disease. Likewise, the frequency of death due to cardiovascular causes in adults with diabetes is 2–4 times higher than in individuals without diabetes.
The importance of low-density lipoprotein cholesterol (LDLc) in reducing cardiovascular risk in T2DM has been demonstrated in different studies and meta-analyses.5 An association between dyslipidemia and cardiovascular disease (CVD) was demonstrated in the United Kingdom Prospective Diabetes Study (UKPDS: 23), which found an increase of 38.5mg/dl in LDLc concentration to be associated with a 157% increase in coronary artery disease, while an increase of 4mg/dl in high-density lipoprotein cholesterol (HDLc) was associated with a 15% decrease in cardiovascular events.6 The principal risk factor for developing coronary disease was therefore identified as LDLc, followed by HDLc levels.
Dyslipidemia needs to be diagnosed and treated early in an effective manner in order to reduce the risk of future cardiovascular events.
In Spain, a number of epidemiological studies have analyzed the prevalence of lipid disorders,7–13 with figures ranging from 56.2% in the study published by Domínguez13 to 92.6% in the OBEDIA trial.8 However, little information is available on the prevalence and factors associated with dyslipidemia in patients with T2DM in the Autonomous Community of Cantabria.
The objectives of the present study are to: (1) estimate the prevalence of dyslipidemia; (2) investigate the risk factors associated with dyslipidemia; and (3) evaluate the risk factors independently associated with dyslipidemia.
Material and methodsA cross-sectional population-based study was carried out involving a sample of 680 patients with T2DM between January 2014 and December 2015. A multistage procedure was used, based on a randomized sample of primary care centers, with selection probability proportional to size. Of the 42 primary care centers registered in the Health Service of Cantabria, we randomly selected a third, i.e., 13 centers. A subsequent second random selection yielded a subsample of the patient quotas of the physicians in each of the selected primary care centers. The general criterion was to select both the centers and the patient quotas of the physicians with selection probability proportional to size. If any center declined participation in the study, it was replaced by another center in the same stratum, based on strict randomization.
We estimated that the study could be feasible with a sample of 384 patients, assuming 50% of the diabetic patients to be well controlled (p=0.50%), with a precision of 5% and a confidence level of 95%. Assuming a 15% information loss rate, the calculated necessary sample size was 452 patients. A total of 680 patients were finally included, following the screening criteria described above. The study protocol was approved by the Clinical Research Ethics Committee of Cantabria.
Following patient identification and signing of the informed consent, a conventional examination was made to record the clinical parameters and free assignment to treatment (according to standard clinical practice).
Three laboratory tests were performed under fasting conditions (at least 12h): at entry to the study, and after 6 and 12 months, with calculation of the mean of the three values. On site follow-up was performed at 1% of the randomly selected centers, and the protection of personal data was ensured.
Information was collected corresponding to each patient in the study, including age, gender, race, year of diagnosis of T2DM, place of residence, educational level, family income, occupational status, smoking habit, weight, height, waist circumference, estimated body fat, the body mass index (BMI), systolic and diastolic blood pressure, abdominal obesity, a history of CVD, arterial hypertension (AHT), antihypertensive treatment, dyslipidemia, lipid-lowering therapy, renal failure and retinopathy. In addition, laboratory parameters were recorded in the form of the albumin/creatinine ratio, the glomerular filtration rate (GFR), glycosylated hemoglobin (HbA1c), plasma glucose, total cholesterol (TC), LDLc, HDLc, triglycerides (TGs) and creatinine concentration.
For blood pressure recording, three measurements of systolic and diastolic blood pressure were made on three successive visits, using a validated blood pressure monitor. The mean of the three measurements was used for analysis.
Dyslipidemic individuals were defined as: (a) patients not receiving lipid-lowering treatment and with LDLc≥160mg/dl, HDLc<40mg/dl in men and <50mg/dl in women, or TG≥150mg/dl; and (b) patients receiving lipid-lowering treatment (even in the presence of lipid levels below those cited above). In defining hypertriglyceridemia, and for reasons that are difficult to explain, both TG>150mg/dl (upper limit according to the ATP III and the criterion used for defining metabolic syndrome) and TG>200mg/dl (high values according to the ATP III) are used.14 The American Diabetes Association and European bodies have established that in the high cardiovascular risk population, adequate TG levels are <150mg/dl, while adequate HDLc levels are taken to be >40/50mg/dl, depending on whether the individual is male or female.15 We calculated LDLc based on the Friedewald formula (LDLc mg/dl=TC (mg/dl)−HDLc (mg/dl)−TG (mg/dl)/5) – a method that proves inaccurate when the TG levels are high (≥ 400mg/dl)1.
Arterial hypertension in turn was defined as blood pressure ≥140/90mmHg or as the prescription of antihypertensive medication. The criterion for good blood pressure control was <140/90mmHg or <150/90mmHg for individuals ≥80 years of age.16,17
Controlled diabetes was defined as HbA1c<7%, or <8% for individuals ≥80 years of age, according to the criteria of the American Diabetes Association and the recommendations of the Diabetes and Cardiovascular Disease Working Group of the Spanish Society of Diabetes (Sociedad Española de Diabetes [SED], 2015).17
The evaluation of microalbuminuria was based on the calculation of the albumin/creatinine ratio (mg/g) in an isolated first morning urine sample. Microalbuminuria was defined as a ratio of 30–300mg/g, and proteinuria as >300mg/g.
Renal failure was defined as a GFR<60ml/min/1.73m2 on a persistent basis for at least three months, according to the criteria of the Kidney Disease Outcomes Quality Initiative (KDOQI). The estimated glomerular filtration rate (eGFR) was calculated using the equation derived from the Modification of Diet in Renal Disease (MDRD) study.
A smoker was defined as a person who at the time of entry to the study was an active smoker of cigarettes, cigars or pipe tobacco in any amount, was an occasional smoker, or had quit smoking in the 12 months prior to entry to the study. An ex-smoker in turn was defined as a person who had not smoked for more than 12 months.
The body mass index (BMI) expressed in kg/m2 was used to define obesity. Specifically, overweight was defined as a BMI≥25kg/m2 and obesity as a BMI≥30kg/m2, in line with the consensus document of the Spanish Society for the Study of Obesity (Sociedad Española para el Estudio de la Obesidad). We likewise defined central obesity according to the cut-off points proposed by the NCEP-ATP-III,14 namely a waist circumference >88cm in women and >102cm in men. The waist circumference was measured in the standing position, at the midpoint between the iliac crest and the rib margin, on the mid-axillary line.
The University of Navarra Body Adiposity Estimator (CUN-BAE) was used to define estimated body fat. The CUN-BAE cut-off point was based on the criteria established by the authors of this equation. Accordingly, overweight was defined as an estimated percentage body fat of >20% and ≤25% in males, and of >30% and ≤35% in females. Obesity in turn was defined as an estimated percentage body fat of ≥25% in men and of >35% in women.
A history of CVD was defined as the presence of ischemic heart disease, cerebrovascular disease or peripheral arterial disease.
A sedentary lifestyle was defined as less than 150min/week of physical exercise, in accordance with the criteria proposed by the American College of Sports Medicine.
Retinopathy was evaluated from the last available retinographic study corresponding to the previous year. If not available, retinography was requested at the time of inclusion in the study.
The SPSS version 23 statistical package was used for data analysis. Qualitative variables were expressed as absolute values and percentages, with estimation of the corresponding 95% confidence interval (95% CI). Quantitative variables were reported as the mean±standard deviation (SD) and 95% CI. Analysis of the relationships referring to quantitative and qualitative variables was based on bivariate analyses (chi-squared test, Fisher's exact test, maximum likelihood estimation, Student t-test, analysis of variance [ANOVA], Mann–Whitney U-test, Kruskal–Wallis test, depending on the nature of the variables). Unconditional multivariate binary logistic regression analysis was performed with dyslipidemia as the dependent variable, taking into account the parameters which in the bivariate analysis were found to be associated with the presence of dyslipidemia or proved clinically relevant, namely patient age, gender, arterial hypertension, a history of peripheral vascular disease, controlled diabetes, antidiabetic treatment, HbA1c≥7%, the albumin/creatinine ratio, the glomerular filtration rate, a history of CVD, years since diabetes onset, basal blood glucose, creatinine, and retinopathy. All statistical analyses were two-tailed, and statistical significance was considered for p<0.05.
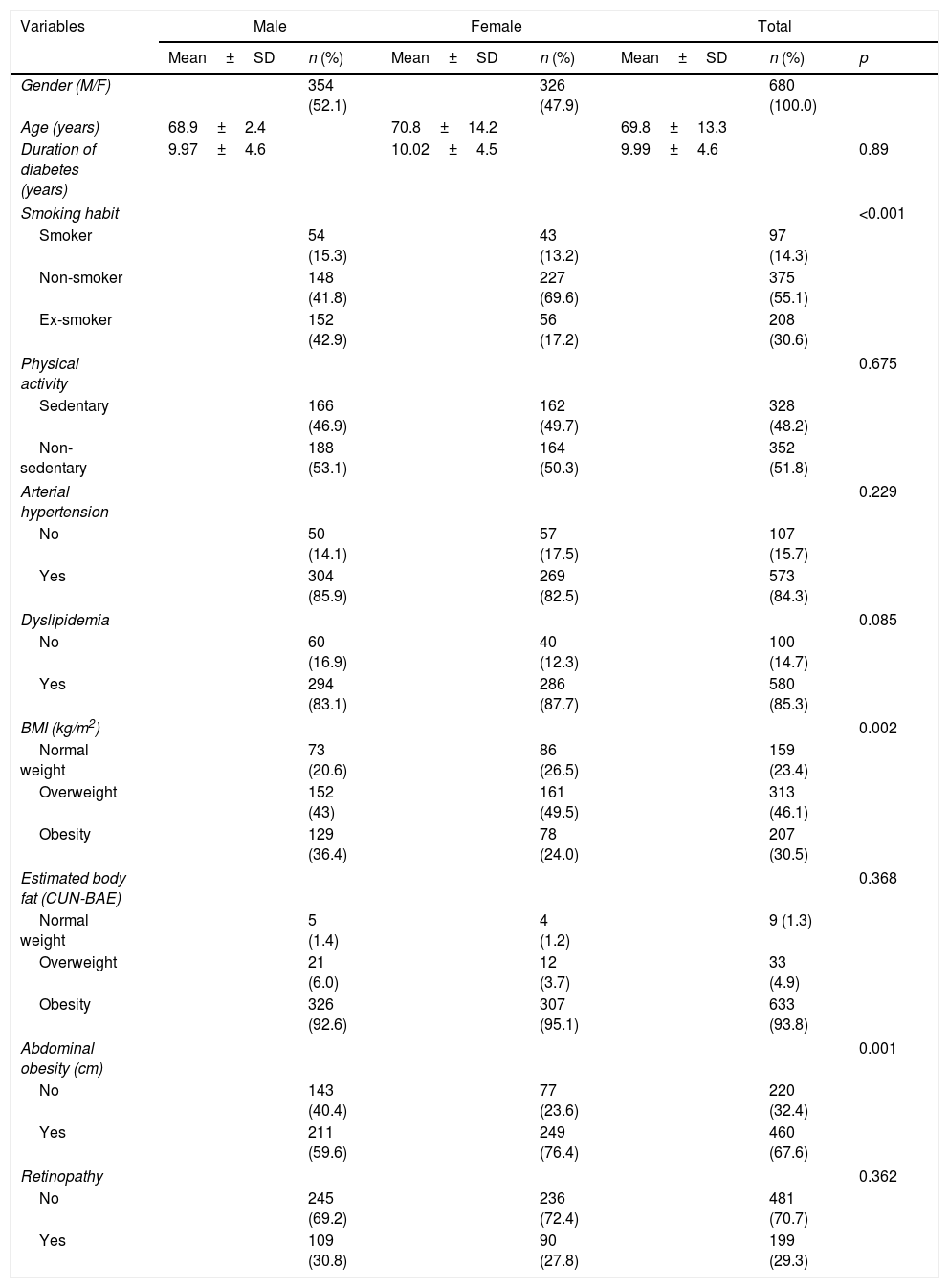
ResultsThe baseline characteristics are summarized in Table 1. Of the 680 patients included in the study, 68.9% were ≥65 years of age (mean 69.84 years), 96.6% were Caucasian, and the mean duration of diabetes was 9.99 years. A total of 68.2% of the participants lived in an urban setting, 50% had primary education, 74% were retired, and 75% had an annual income of less than 18,000 euros. There was a slight predominance of men (52.1%), and the women were comparatively older (70.8 years).
General characteristics of the study population according to gender.
| Variables | Male | Female | Total | ||||
|---|---|---|---|---|---|---|---|
| Mean±SD | n (%) | Mean±SD | n (%) | Mean±SD | n (%) | p | |
| Gender (M/F) | 354 (52.1) | 326 (47.9) | 680 (100.0) | ||||
| Age (years) | 68.9±2.4 | 70.8±14.2 | 69.8±13.3 | ||||
| Duration of diabetes (years) | 9.97±4.6 | 10.02±4.5 | 9.99±4.6 | 0.89 | |||
| Smoking habit | <0.001 | ||||||
| Smoker | 54 (15.3) | 43 (13.2) | 97 (14.3) | ||||
| Non-smoker | 148 (41.8) | 227 (69.6) | 375 (55.1) | ||||
| Ex-smoker | 152 (42.9) | 56 (17.2) | 208 (30.6) | ||||
| Physical activity | 0.675 | ||||||
| Sedentary | 166 (46.9) | 162 (49.7) | 328 (48.2) | ||||
| Non-sedentary | 188 (53.1) | 164 (50.3) | 352 (51.8) | ||||
| Arterial hypertension | 0.229 | ||||||
| No | 50 (14.1) | 57 (17.5) | 107 (15.7) | ||||
| Yes | 304 (85.9) | 269 (82.5) | 573 (84.3) | ||||
| Dyslipidemia | 0.085 | ||||||
| No | 60 (16.9) | 40 (12.3) | 100 (14.7) | ||||
| Yes | 294 (83.1) | 286 (87.7) | 580 (85.3) | ||||
| BMI (kg/m2) | 0.002 | ||||||
| Normal weight | 73 (20.6) | 86 (26.5) | 159 (23.4) | ||||
| Overweight | 152 (43) | 161 (49.5) | 313 (46.1) | ||||
| Obesity | 129 (36.4) | 78 (24.0) | 207 (30.5) | ||||
| Estimated body fat (CUN-BAE) | 0.368 | ||||||
| Normal weight | 5 (1.4) | 4 (1.2) | 9 (1.3) | ||||
| Overweight | 21 (6.0) | 12 (3.7) | 33 (4.9) | ||||
| Obesity | 326 (92.6) | 307 (95.1) | 633 (93.8) | ||||
| Abdominal obesity (cm) | 0.001 | ||||||
| No | 143 (40.4) | 77 (23.6) | 220 (32.4) | ||||
| Yes | 211 (59.6) | 249 (76.4) | 460 (67.6) | ||||
| Retinopathy | 0.362 | ||||||
| No | 245 (69.2) | 236 (72.4) | 481 (70.7) | ||||
| Yes | 109 (30.8) | 90 (27.8) | 199 (29.3) | ||||
Values:
HDLc<40mg/dl in men and <50mg/dl in women or TG>150mg/dl.
CUN-BAE: normal weight: men<20 and women<30; overweight: men 20–25 and women 30–35; obesity: men >25 and women >35.
Arterial hypertension under drug treatment or blood pressure >140/90mmHg Dyslipidemia: patients under lipid-lowering treatment or those without lipid-lowering treatment but with LDLc>160mg/dl.
BMI: normal weight <25; overweight 25–29.99; obesity >30.
Abdominal obesity: waist circumference >102cm in men and >88cm in women.
HDLc: high density lipoprotein cholesterol; LDLc: low density lipoprotein cholesterol; TC: total cholesterol; CUN-BAE: University of Navarra Body Adiposity Estimator; SD: standard deviation; M: male; HbA1c: glycosylated hemoglobin; BMI: body mass index; F: female; BP: blood pressure; TG: triglycerides.
Active smoking and obesity according to the BMI proved significantly greater in men, while abdominal obesity was significantly greater in women.
The prevalence of dyslipidemia was 85.3%, arterial hypertension 84.3%, renal failure 22.9%, sedentary lifestyle 48.2%, microalbuminuria and proteinuria 31.3%, overweight and obesity according to the BMI 76.6%, obesity based on body fat estimated with the CUN-BAE 93%, abdominal obesity 67.6%, and retinopathy 29.3% (Table 1).
The prevalence of dyslipidemia was similar in women and men (87.7% versus 83.1%, respectively; p=0.085) (Table 1). Of the dyslipidemic subjects, 79.5% were defined as having dyslipidemia due to the prescription of lipid-lowering treatment, while 20.5% not receiving lipid-lowering treatment were considered to be dyslipidemic due to LDLc>160mg/dl, HDLc<40mg/dl in men or <50mg/dl in women, or TG≥150mg/dl.
A total of 75.3% of the subjects received lipid-lowering treatment: 71.1% received statins; 5.4% ezetimibe; 3.3% fibrates; 0.8% ion exchange resins and 0.5% received omega-3 fatty acid ethyl esters. Most of the patients (69.6%) received monotherapy while 5.7% received dual therapy.
Of the dyslipidemic subjects under lipid-lowering treatment, 96.5% received statins or ezetimibe, 4.3% received fibrates and 2% received statins and fibrates. Of the subjects diagnosed with dyslipidemia but not receiving lipid-lowering treatment, 14.3% presented LDLc>160mg/dl; 79% HDLc<40mg/dl in men or <50mg/dl in women, and 51.3% TG>150mg/dl.
Mean basal glycemia was 137.85±46.59mg/dl, while TC concentration was 178.17±38.18mg/dl, HDLc 47.09±12.10mg/dl, LDLc 108.10±36.44mg/dl, TG 136.6±66.3mg/dl and creatinine 0.96±0.55mg/dl.
A total of 68.7% of the patients had normoalbuminuria, 23.8% microalbuminuria and 7.5% had overt proteinuria.
In turn, 77.1% of the patients presented an estimated glomerular filtration rate (eGFR) (MDRD) of >60ml/min/1.73m2 and 22.9% suffered renal failure (eGFR<60ml/min/1.73m2). Of the patients with renal failure, 19.1% had an eGFR 30–59ml/min/1.73m2, 2.9% an eGFR 15–29ml/min/1.73m2 and 0.9% an eGFR<15ml/min/1.73m2.
Mean basal glycemia, TG and creatinine levels were significantly higher in males, while the mean TC, HDLc and LDLc levels were significantly higher in females. Microalbuminuria and proteinuria were significantly more prevalent in men.
Full lipid parameters were obtained from 680 patients registering one or more parameters. Of these subjects, 26.6% did not reach the TC objectives (<200mg/dl), and 54.9% did not reach the LDLc objectives (<100mg/dl). Elevated TG concentrations (≥150mg/dl) were documented in 33.7% of the cases and low HDLc (<40mg/dl in males and <50mg/dl in females) in 46%. As regards the combined alterations, off-target LDLc levels and low HDLc were recorded in 23.7% of the cases, off-target LDLc levels, low HDLc or elevated TG levels in 14%; and off-target LDLc and TC levels, low HDLc or elevated TG levels in 6.6%.
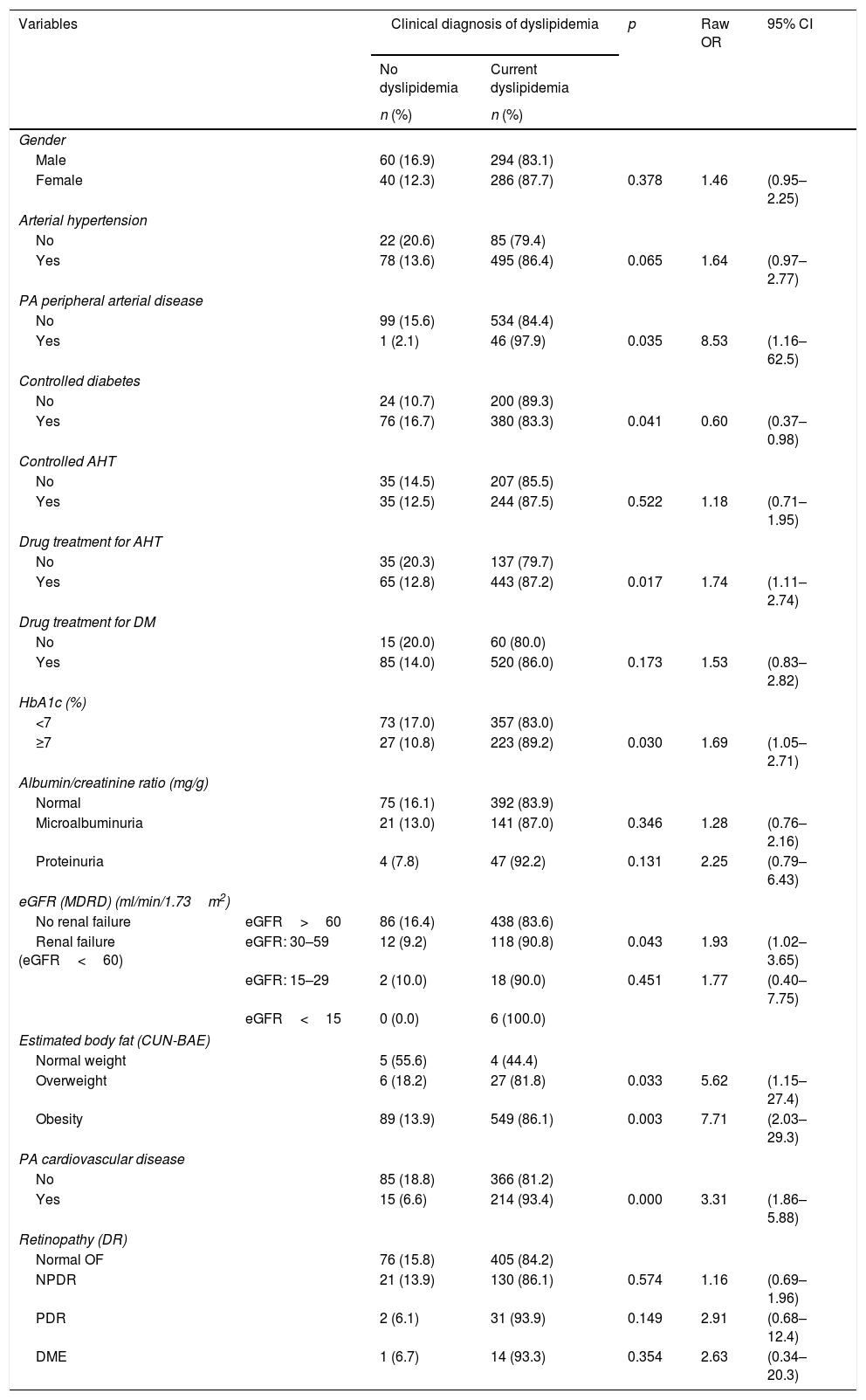
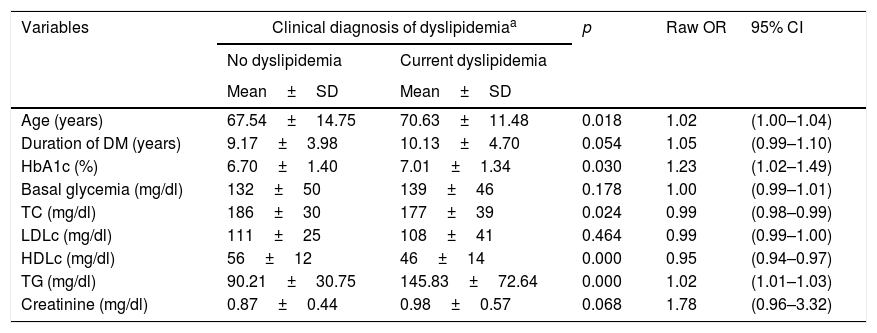
In the bivariate analysis, the variables associated with the presence of dyslipidemia were a history of peripheral vascular disease, controlled diabetes, drug treatment for arterial hypertension, HbA1c≥7%, the GFR, the estimated body fat in overweight and obese individuals, a history of CVD, age and HbA1c concentration (Tables 2 and 3). A history of peripheral vascular disease is included within the variable history of CVD.
Qualitative variables associated with the presence of dyslipidemia.
| Variables | Clinical diagnosis of dyslipidemia | p | Raw OR | 95% CI | ||
|---|---|---|---|---|---|---|
| No dyslipidemia | Current dyslipidemia | |||||
| n (%) | n (%) | |||||
| Gender | ||||||
| Male | 60 (16.9) | 294 (83.1) | ||||
| Female | 40 (12.3) | 286 (87.7) | 0.378 | 1.46 | (0.95–2.25) | |
| Arterial hypertension | ||||||
| No | 22 (20.6) | 85 (79.4) | ||||
| Yes | 78 (13.6) | 495 (86.4) | 0.065 | 1.64 | (0.97–2.77) | |
| PA peripheral arterial disease | ||||||
| No | 99 (15.6) | 534 (84.4) | ||||
| Yes | 1 (2.1) | 46 (97.9) | 0.035 | 8.53 | (1.16–62.5) | |
| Controlled diabetes | ||||||
| No | 24 (10.7) | 200 (89.3) | ||||
| Yes | 76 (16.7) | 380 (83.3) | 0.041 | 0.60 | (0.37–0.98) | |
| Controlled AHT | ||||||
| No | 35 (14.5) | 207 (85.5) | ||||
| Yes | 35 (12.5) | 244 (87.5) | 0.522 | 1.18 | (0.71–1.95) | |
| Drug treatment for AHT | ||||||
| No | 35 (20.3) | 137 (79.7) | ||||
| Yes | 65 (12.8) | 443 (87.2) | 0.017 | 1.74 | (1.11–2.74) | |
| Drug treatment for DM | ||||||
| No | 15 (20.0) | 60 (80.0) | ||||
| Yes | 85 (14.0) | 520 (86.0) | 0.173 | 1.53 | (0.83–2.82) | |
| HbA1c (%) | ||||||
| <7 | 73 (17.0) | 357 (83.0) | ||||
| ≥7 | 27 (10.8) | 223 (89.2) | 0.030 | 1.69 | (1.05–2.71) | |
| Albumin/creatinine ratio (mg/g) | ||||||
| Normal | 75 (16.1) | 392 (83.9) | ||||
| Microalbuminuria | 21 (13.0) | 141 (87.0) | 0.346 | 1.28 | (0.76–2.16) | |
| Proteinuria | 4 (7.8) | 47 (92.2) | 0.131 | 2.25 | (0.79–6.43) | |
| eGFR (MDRD) (ml/min/1.73m2) | ||||||
| No renal failure | eGFR>60 | 86 (16.4) | 438 (83.6) | |||
| Renal failure (eGFR<60) | eGFR: 30–59 | 12 (9.2) | 118 (90.8) | 0.043 | 1.93 | (1.02–3.65) |
| eGFR: 15–29 | 2 (10.0) | 18 (90.0) | 0.451 | 1.77 | (0.40–7.75) | |
| eGFR<15 | 0 (0.0) | 6 (100.0) | ||||
| Estimated body fat (CUN-BAE) | ||||||
| Normal weight | 5 (55.6) | 4 (44.4) | ||||
| Overweight | 6 (18.2) | 27 (81.8) | 0.033 | 5.62 | (1.15–27.4) | |
| Obesity | 89 (13.9) | 549 (86.1) | 0.003 | 7.71 | (2.03–29.3) | |
| PA cardiovascular disease | ||||||
| No | 85 (18.8) | 366 (81.2) | ||||
| Yes | 15 (6.6) | 214 (93.4) | 0.000 | 3.31 | (1.86–5.88) | |
| Retinopathy (DR) | ||||||
| Normal OF | 76 (15.8) | 405 (84.2) | ||||
| NPDR | 21 (13.9) | 130 (86.1) | 0.574 | 1.16 | (0.69–1.96) | |
| PDR | 2 (6.1) | 31 (93.9) | 0.149 | 2.91 | (0.68–12.4) | |
| DME | 1 (6.7) | 14 (93.3) | 0.354 | 2.63 | (0.34–20.3) | |
CUN-BAE: normal weight: men<20 and women<30; overweight: men 20–25 and women 30–35; obesity: men>25 and women>35.
Controlled diabetes: HbA1c<7% or<8% in subjects >80 years.
Dyslipidemia: patients under lipid-lowering treatment or those without lipid-lowering treatment but with LDLc>160mg/dl, HDLc<40mg/dl in men and <50mg/dl in women, or TG>150mg/dl.
Cardiovascular disease: stroke, ischemic heart disease, peripheral arterial disease.
Arterial hypertension: subjects under drug treatment or blood pressure>140/90mmHg
Controlled AHT: BP<140/90mmHg or<150/90mmHg if >80 years of age.
BMI: normal weight<25; overweight 25–29.99; obesity>30.
Renal failure: eGFR<60ml/min/1.73m2.
Normoalbuminuria<30mg/g; microalbuminuria 30–300mg/g; proteinuria>300mg/g.
Abdominal obesity: waist circumference>102cm in men and >88cm in women.
PA: peripheral arterial disease; IHD: ischemic heart disease; CUN-BAE: University of Navarra Body Adiposity Estimator; DME: diabetic macular edema; OF: ocular fundus; HbA1c: glycosylated hemoglobin; AHT: arterial hypertension; BMI: body mass index; BP: blood pressure; DR: diabetic retinopathy; NPDR: non-proliferative diabetic retinopathy; PDR: proliferative diabetic retinopathy; eGFR: estimated glomerular filtration rate.
Quantitative variables associated with the presence of dyslipidemia.
| Variables | Clinical diagnosis of dyslipidemiaa | p | Raw OR | 95% CI | |
|---|---|---|---|---|---|
| No dyslipidemia | Current dyslipidemia | ||||
| Mean±SD | Mean±SD | ||||
| Age (years) | 67.54±14.75 | 70.63±11.48 | 0.018 | 1.02 | (1.00–1.04) |
| Duration of DM (years) | 9.17±3.98 | 10.13±4.70 | 0.054 | 1.05 | (0.99–1.10) |
| HbA1c (%) | 6.70±1.40 | 7.01±1.34 | 0.030 | 1.23 | (1.02–1.49) |
| Basal glycemia (mg/dl) | 132±50 | 139±46 | 0.178 | 1.00 | (0.99–1.01) |
| TC (mg/dl) | 186±30 | 177±39 | 0.024 | 0.99 | (0.98–0.99) |
| LDLc (mg/dl) | 111±25 | 108±41 | 0.464 | 0.99 | (0.99–1.00) |
| HDLc (mg/dl) | 56±12 | 46±14 | 0.000 | 0.95 | (0.94–0.97) |
| TG (mg/dl) | 90.21±30.75 | 145.83±72.64 | 0.000 | 1.02 | (1.01–1.03) |
| Creatinine (mg/dl) | 0.87±0.44 | 0.98±0.57 | 0.068 | 1.78 | (0.96–3.32) |
Dyslipidemia: patients under lipid-lowering treatment or those without lipid-lowering treatment but with LDLc>160mg/dl, HDLc<40mg/dl in men and <50mg/dl in women, or TG>150mg/dl.
HDLc: high density lipoprotein cholesterol; LDLc: low density lipoprotein cholesterol; TC: total cholesterol; DM: diabetes mellitus; HbA1c: glycosylated hemoglobin; CI: confidence interval; OR: odds ratio; TG: triglycerides.
No significant differences in the presence of dyslipidemia were recorded in relation to the following variables: gender, race, family income, educational level, occupational status, place of residence, smoking habit, AHT, controlled AHT, drug treatment for DM, the albumin/creatinine ratio, the BMI, abdominal obesity, diabetic retinopathy, years since onset, basal glycemia or creatinine. Although no significant differences were found, the subjects with dyslipidemia presented a longer duration of DM, higher basal glycemia and creatinine levels, and higher BMI values. In turn, female gender, the Negro race, a family income of less than 18,000 euros, a low educational level (illiterate or primary education only), retired status, and urban residence were more prevalent in the dyslipidemic subjects. Smoking habit (smoker and ex-smoker status), AHT, microalbuminuria, proteinuria and diabetic retinopathy were also more prevalent in dyslipidemic than in non-dyslipidemic patients. We likewise found the prevalence of dyslipidemia to be greater as microalbuminuria and diabetic retinopathy increased, and when eGFR decreased.
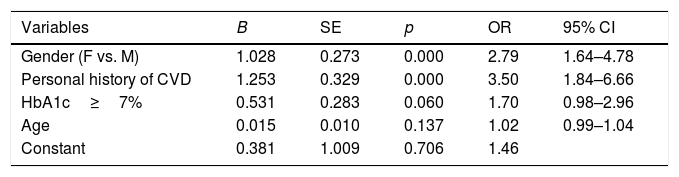
In the multivariate analysis, the variables seen to be independently associated with dyslipidemia were female gender and a personal history of CVD (Table 4).
Multivariate model. Variables independently associated with dyslipidemia.
| Variables | B | SE | p | OR | 95% CI |
|---|---|---|---|---|---|
| Gender (F vs. M) | 1.028 | 0.273 | 0.000 | 2.79 | 1.64–4.78 |
| Personal history of CVD | 1.253 | 0.329 | 0.000 | 3.50 | 1.84–6.66 |
| HbA1c≥7% | 0.531 | 0.283 | 0.060 | 1.70 | 0.98–2.96 |
| Age | 0.015 | 0.010 | 0.137 | 1.02 | 0.99–1.04 |
| Constant | 0.381 | 1.009 | 0.706 | 1.46 |
The model contains the following variables: gender (female vs. male), a personal history of CVD (stroke, ischemic heart disease, peripheral arterial disease), HbA1c>7% and age (continuous, for each additional year).
B: regression coefficient; CVD: cardiovascular disease; SE: standard error of B; M: males; HbA1c: glycosylated hemoglobin; CI: confidence interval; F: females; OR: odds ratio.
The results obtained suggest that the prevalence of dyslipidemia in patients with T2DM in the Autonomous Community of Cantabria (Spain) is high, and that less than 15% of the patients show normal lipid values or the values recommended by the main clinical practice guidelines.1,15,16,18–21 This is consistent with results recorded in other studies both in Spain and elsewhere.7–13,22–25
On comparing these results with those of other publications, great variability is observed. In most studies, the prevalence of dyslipidemia is over 50%, with a range from 56.2% according to Domínguez13 to 92.6% in the OBEDIA study.8 However, this variability in the prevalence of dyslipidemia may be attributable to heterogeneity in the way it is diagnosed and to the use of different diagnostic criteria. In this context, the greater prevalence observed in the OBEDIA study8 could be related to the LDLc cut-off point considered in defining dyslipidemia, which was lower than that used in our study.
These discrepancies are common in the medical literature, because the methodology used to carry out the studies (with diverse diagnostic criteria, laboratory methods, or different cut-off points for determining the various lipidemic factors and their associated cardiovascular risk), as well as population diversity, influences the results obtained. It is also important to emphasize that despite their randomness in selecting the subjects, studies involving population-based samples might not be representative of the reference population, or may be quite delimited in space and time, thereby precluding comparison with the data from other studies.
Such a high prevalence could be related to the profile of the patients studied (high obesity rates, kidney disease, poor metabolic control of diabetes, etc.), since 69% of the study sample was over 65 years of age. These analytical values are not dependent upon the records made by the healthcare professionals and are a genuine reflection of the real life situation. However, we cannot overlook selection bias, which may be related to patients presenting previously altered laboratory test values or to very frequently visiting patients.
Although multiple cross-sectional epidemiological studies have analyzed the prevalence of dyslipidemia in diabetic populations with different levels of cardiovascular risk,7–13,22 this is the first study in Spain to analyze the characteristics, prevalence and factors associated with dyslipidemia in a representative sample of patients with T2DM in Cantabria. In addition, on assessing the prevalence of dyslipidemia, the previous studies usually focused on isolated alterations of TC or LDLc according to the recommendations of the NCEP ATP III,14 with no full lipid profile analysis and without considering patients receiving lipid-lowering treatment. The present study adopts a broader perspective and includes the following individuals in the analysis of the prevalence of dyslipidemia: (a) those not receiving lipid-lowering treatment but presenting altered LDLc, HDLc and TG values; and (b) those receiving lipid-lowering treatment.
Of the dyslipidemic subjects, 79.5% were classified as dyslipidemic because they were receiving lipid-lowering treatment, and 20.5% were classified as dyslipidemic on the basis of lipid parameter criteria. This high prevalence of individuals considered to have dyslipidemia due to the prescription of lipid-lowering treatment is probably related to the indication of lipid-lowering therapy as a cardiovascular protective measure in patients with prior CVD or at high cardiovascular risk without CVD, even in the absence of dyslipidemia. This is consistent with the association dyslipidemia-a history of CVD and the trend with disease duration and age.
In the subjects diagnosed with dyslipidemia that were not receiving lipid-lowering treatment, low HDLc levels were found to be the most common lipid disorder (79%). Likewise, we observed a considerable increase in TG (51.3%), together with a discrete increase in LDLc (14.3%). These results are consistent with the quantitative alterations reported in dyslipidemia among patients with DM (“atherogenic dyslipidemia”). Atherogenic dyslipidemia is a characteristic element of the residual vascular risk of lipid origin not associated with changes in LDLc levels; it is a highly prevalent form of dyslipidemia in people with T2DM, in patients at high or very high risk, visceral obesity, or metabolic syndrome.
A large proportion of patients in our sample did not reach the LDLc objectives or targets. We also found that a significant proportion of individuals presented high TG and low HDLc levels, which agrees with the literature, where elevated TG levels and decreased HDLc are found in approximately half of all patients with T2DM.26 These data are indicative of an important residual risk (suboptimal LDLc, HDLc and TG levels) that should probably be controlled more intensively than is done in routine clinical practice, and which may be related to therapeutic compliance and inertia. In patients with T2DM, the non-compliance rates are very high (32%, 36% and 38% for lipid-lowering, antidiabetic and antihypertensive drugs, respectively).9
On examining compliance with the objectives according to the recommendations of the clinical practice guides, we found two-thirds of the patients to have adequate TG levels (67.2%), and less than 50% failed to reach optimum LDLc (45.1%) and HDLc levels (46%). On comparing these results with those obtained in a cross-sectional study carried out in the 17 Spanish Autonomous Communities,27 the studied subjects were seen to more frequently reach the recommended lipid targets. In patients with T2DM and dyslipidemia, the global therapeutic approach should focus not only on LDLc but also on the control of HDLc and TG levels as secondary therapeutic objectives. This may entail a change in therapeutic approach in order to reach these objectives.15
The main contribution of our study is knowledge of the high prevalence of dyslipidemia (85.3%) in patients with T2DM in Cantabria, and identification of the female gender and a history of CVD as the factors independently associated with dyslipidemia. This knowledge can serve as the first step toward implementing the necessary means to improve the overall lipid profile. It should therefore prove useful for defining continuous improvement strategies, implicating all those involved (medical and nursing staff, and the health authorities) in the application of the clinical guidelines and in improving patient adherence.
Our results indicate that there is often more than a single alteration in plasma lipid values. In effect, 23.7% of the patients presented joint alterations of LDLc and HDLc; 14.7% of LDLc, HDLc and TG; and 6.6% of all four lipid parameters. The TC, HDLc and LDLc concentrations were significantly higher in females, while the TG levels were significantly higher in males. These findings are similar to those recorded in a study conducted in Catalonia.7 In the United Kingdom Prospective Diabetes Study (UKPDS: 23) 27, TC, HDLc and LDLc were seen to be significantly higher in women, this being consistent with our own observations.28
The multivariate analysis identified the female gender and a personal history of CVD as being independently associated with dyslipidemia, beyond age and the HbA1c level.
The prevalence of dyslipidemia was associated with the female gender, in line with the observations of other studies.28,29 As regards the association between gender and dyslipidemia, the women in our study were most affected by dyslipidemia, despite the fact that males predominated in the sample (52.1%). The association between the two categorical variables revealed by the multivariate analysis suggests that being female in this group of patients increased the risk of developing dyslipidemia almost three-fold. An altered lipid profile is a characteristic feature of DM and confers a greater risk of developing CVD, particularly coronary artery disease. The relative risk of fatal coronary heart disease associated with DM is 50% higher in women than in men.30 The cause of the increased risk of coronary heart disease in women with DM is not yet fully known. However, the changes induced by T2DM in some cardiovascular risk factors such as LDLc, HDLc, TG and blood pressure have been more marked in women as compared to men, and this may explain the greater increase in arteriosclerosis risk among diabetic women.28,30 In addition, gender differences in lipid profile may play a role in the more negative impact of diabetes upon cardiovascular risk in women as compared to men.30 Likewise, it has been postulated that the increased prevalence of dyslipidemia in elderly women may be related to hormonal changes before and after menopause.
The prevalence of dyslipidemia was associated with a personal history of CVD. In the present study, a history of CVD was significantly more prevalent in males (39.5%), and almost four out of every 10 patients with dyslipidemia had a history of CVD (35.8%). The association between both categorical variables shown by the multivariate analysis suggests that a personal history of CVD in this group of patients increased the risk of presenting dyslipidemia 3.5-fold. In this regard, it is important to emphasize that hypercholesterolemia is a highly prevalent risk factor in patients with CVD and confers a special risk of suffering such disease, particularly ischemic heart disease. Furthermore, high TC and LDLc levels are among the most important CVD risk factors; low HDLc and high TG levels are independent CVD risk factors; and statin therapy exerts a beneficial effect upon the incidence of atherosclerotic CVD.21
Our study has a number of limitations and strengths. The main limitations include those inherent to the study design (cross-sectional) and to information analysis. Specifically, mention must be made of the presence of time bias, the impossibility of generalizing the results to populations with characteristics different from those of our study, and the fact that the findings of the bivariate and multivariate analyses are unable to establish causal relationships or predictions. In this regard, prospective studies are needed to confirm these findings and to allow for more detailed analyses of the variables associated with the prevalence of dyslipidemia.
Of note in relation to our study is the randomized sampling strategy on which it is based, comprising a representative sample from the Autonomous Community of Cantabria, as well as the fact that it has been implemented by a single observer, thereby avoiding confusion in data collection due to the interaction of different investigators. However, it cannot be discarded that the data from those patients who refused to participate could have affected our results, or that the diabetic patients from the primary care centers in Cantabria might not be representative of Spain as a whole. In any case, the comparison of our results with the studies published at national and international level demonstrates the consistency of the data obtained. In addition, other variables may be valid predictors of dyslipidemia. Our study did not take into account possible changes in lipid-lowering therapy and patient adherence to therapy. Lastly, cross-sectional designs are widely used, because the associated costs are relatively lower than those of other epidemiological designs, such as cohort studies, and they rapidly afford relevant information for healthcare management.
Due to the relevance of the subject under study, we believe it necessary to emphasize the importance of conducting further research in this field.
ConclusionsThe present study shows that there is a high prevalence of dyslipidemia in patients with T2DM in the Autonomous Community of Cantabria. The independently associated risk factors were female gender and a personal history of CVD. The results obtained show that there is a need for the integral and intensive management of dyslipidemia. In this regard, attempts should be made to improve the metabolic control of diabetes, reduce obesity and promote lifestyle changes (smoking cessation, physical exercise, and a decreased consumption of saturated fats and alcohol), with the purpose of curbing CVD and improving the individual and collective quality of life of this patient population.
FundingThis study has received no funding.
Conflicts of interestNone.
Please cite this article as: Díaz Vera AS, Abellán Alemán J, Segura Fragoso A, Martínez de Esteban JP, Lameiro Couso FJ, Golac Rabanal MS, et al. Prevalencia y factores de riesgo asociados a la dislipidemia en pacientes diabéticos tipo 2 de la Comunidad de Cantabria. Endocrinol Diabetes Nutr. 2020;67:102–112.