Newborn infants from mothers with Graves’ disease may suffer from hyper- or hypothyroidism depending on the balance reached between thyrotropin (TSH)-receptor stimulating and binding antibodies, and antithyroid drugs in their passage across the placenta.1,2
These alterations are unusual. Neonatal hyperthyroidism may appear in 1–5% of the offspring of mothers with Graves’ disease; and since Graves’ disease itself occurs in approximately 0.2% of all women, neonatal hyperthyroidism may occur in 1 out of 25,000–50,000 newborns, with no differences regarding sex. Transient hypothyroidism due to the transplacental passage of TSH-receptor binding antibodies is even rarer, affecting 1 in 180,000 newborn infants.3
Even though neonatal hyperthyroidism is frequently self-limiting and resolves during the first 6 months (generally between weeks 3 and 13), it may be life-threatening and determine important sequelae, so early diagnosis and correct treatment are essential.
We report the cases of 2 newborn infants who were diagnosed with neonatal hyperthyroidism late in their third week of life. Both cases presented symptoms from birth, but previous maternal thyroid disturbances had not been noted. Both women had suffered from Graves’ disease and had been treated with radioiodine thyroid ablation some years earlier, but their clinical records only stated that they were hypothyroid and were receiving levothyroxine treatment.
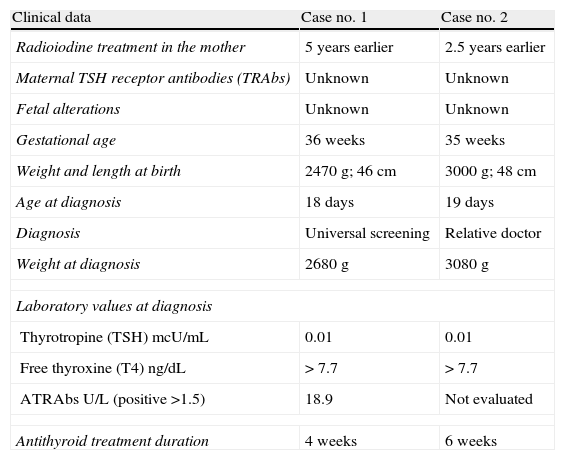
Both infants were premature and presented irritability, insomnia and insufficient body weight gain. Moreover, case number 1 had to be admitted to hospital from day 5 to day 16 due to hyperthermia and hypernatremic dehydration, and persistent sinus tachycardia was observed during a cardiological examination. A diagnosis of hyperthyroidism was not established until day 18, when thyroid function screening-test results were known (suppressed TSH). Case number 2 was diagnosed by a relative who was a doctor. Table 1 summarizes further information.
Clinical data of the patients presented.
| Clinical data | Case no. 1 | Case no. 2 |
| Radioiodine treatment in the mother | 5 years earlier | 2.5 years earlier |
| Maternal TSH receptor antibodies (TRAbs) | Unknown | Unknown |
| Fetal alterations | Unknown | Unknown |
| Gestational age | 36 weeks | 35 weeks |
| Weight and length at birth | 2470g; 46cm | 3000g; 48cm |
| Age at diagnosis | 18 days | 19 days |
| Diagnosis | Universal screening | Relative doctor |
| Weight at diagnosis | 2680g | 3080g |
| Laboratory values at diagnosis | ||
| Thyrotropine (TSH) mcU/mL | 0.01 | 0.01 |
| Free thyroxine (T4) ng/dL | > 7.7 | > 7.7 |
| ATRAbs U/L (positive >1.5) | 18.9 | Not evaluated |
| Antithyroid treatment duration | 4 weeks | 6 weeks |
Both children were prescribed oral metimazole 0.5mg/kg/day/8h and were monitored weekly with physical and laboratory evaluation. Propranolol 2mg/kg/day/8h was prescribed during the first two weeks, which was the period of time it took for the symptoms to disappear and hormone levels to normalize. Metimazole doses were tapered weekly, making a total duration of treatment of 6 and 4 weeks, respectively.
Newborns from mothers with Graves’ disease are only affected when the levels of TSH-receptor antibodies (TRAb) are as high as 3–5 times the normal reference value during the third term of pregnancy.4 This may occur in women with active hyperthyroidism and in those already treated with thyroidectomy or radioiodine, since it takes years for these TRAbs to disappear. Conversely, it is not observed in women who achieve spontaneous remission, in whom TRAb levels are reduced.3,5,6 Children of mothers with chronic autoimmune thyroiditis who have never been hyperthyroid may exceptionally be affected.2
The fetus may present goiter, hyperkinesia, tachycardia and bone maturity acceleration, which may lead to microcephaly, frontal bossing and triangular facies. There is a high risk of prematurity and intrauterine growth retardation.7,8
The newborn infant presents symptoms starting at birth. However, the clinical picture becomes more evident after 48h, when there is increased activity of the 5-monodesiodinase enzyme, which converts T4 (thyroixine) to T3 (triiodothyronine). If the mother is taking antithyroid drugs, the child may be born with hypothyroidism and develop hyperthyroidism 10–20 days later, when these drugs, which have a shorter half-life than TRAbs, are excreted. The clinical presentation is similar to that of other age groups: hyperthermia, sweating, irritability, hyperactivity, insomnia, hyperphagia, weight loss, diarrhea, tachycardia, arrhytmias, cardiac insufficiency, diffuse goiter, ocular opening and exophthalmos.2
When clinical hyperthyroidism is observed, oral antithyroid treatment should be started, preferably metimazole or carbimazole 0.2–1mg/kg/day. Propylthiouracil is contraindicated in children due to its potential hepatotoxicity. Depending on weekly levels of T4 and T3, doses are tapered until withdrawal. Neither TSH or TRAb levels are useful for monitoring treatment, because the former can remain suppressed for prolonged periods of time and the latter may remain elevated even for several weeks after disease remission. Additionally, beta-blockers are usually prescribed during the first two weeks of treatment to control symptoms, until thyroid function has been normalized.5
If hyperthyroidism is diagnosed prenatally by means of ultrasonography, the prescription of antithyroid drugs is required, taking into account their transplacental passage; furthermore, combined treatment with levothyroxine is also recommended to avoid maternal hypothyroidism. Treatment monitoring is carried out by controlling fetal cardiac frequency by ultrasonography, and not by obtaining fetal hormone levels by cordocentesis, which is risky.3
The long-term consequences of fetal and neonatal hyperthyroidism include mental retardation, conductive and behavior alterations, hyperactivity, growth retardation and cranial synostosis,9 as well as secondary hyperthyroidism, especially in cases with severe and persistent fetal hyperthyroidism.10 There are no reports that show whether cases from mothers treated with surgery or radioiodine previously are less severe or are related to fewer complications.
Pregnant women with active Graves’ disease, as well as those treated previously with thyroidectomy or radioiodine, should be evaluated for TRAb levels at 22–26 weeks of gestation. If laboratory results are three times over the normal reference value, women should be advised of the possible risk of neonatal transient hyperthyroidism, and should be monitored accordingly. Ideally, a previous evaluation during the first trimester will also have been recommended in order to anticipate fetal alterations.3,5 Obstetricians, pediatricians and matrons should be aware of this disease and be able to identify it in newborn infants early enough to avoid any undesirable consequences. If values of maternal TRAbs are not available, monitoring and treatment should be carried out as if they were elevated.3,5
Please cite this article as: García García E, Porras Cantarero JA, Fernández López P, Domínguez Gutiérrez de Ceballos R, Domínguez Pascual I. Hipertiroidismo neonatal en hijos de madres con enfermedad de Graves tratadas con radioyodo. Endocrinol Nutr. 2013;60:31–e32.