Constipation and hyporexia are the most common gastrointestinal clinical manifestations in hypothyroid patients. They result from a generalized decrease in gastrointestinal tract motility, and on rare occasions may trigger a pseudo-obstructive picture that usually responds to the administration of thyroid hormone.1 Thus, the occurrence of gastrointestinal complications requiring surgery is anecdotal.2 Thyroid remnant ablation after surgery in patients with differentiated thyroid cancer (DTC) requires stimulation with TSH, which may be performed by administering recombinant human TSH α or after discontinuation of levothyroxine treatment with the resultant elevation in endogenous TSH. This iatrogenic hypothyroid state is symptomatic in a significant number of cases, impairing patient quality of life,3 but clinical symptoms are transient and usually well tolerated in most cases. However, constipation secondary to bowel hypomotility is one of the most commonly reported secondary manifestations.3 The case of a female patient who experienced acute abdomen as an exceptional complication following preparation in a hypothyroid state for ablation with 131I after surgery for DTC is reported below.
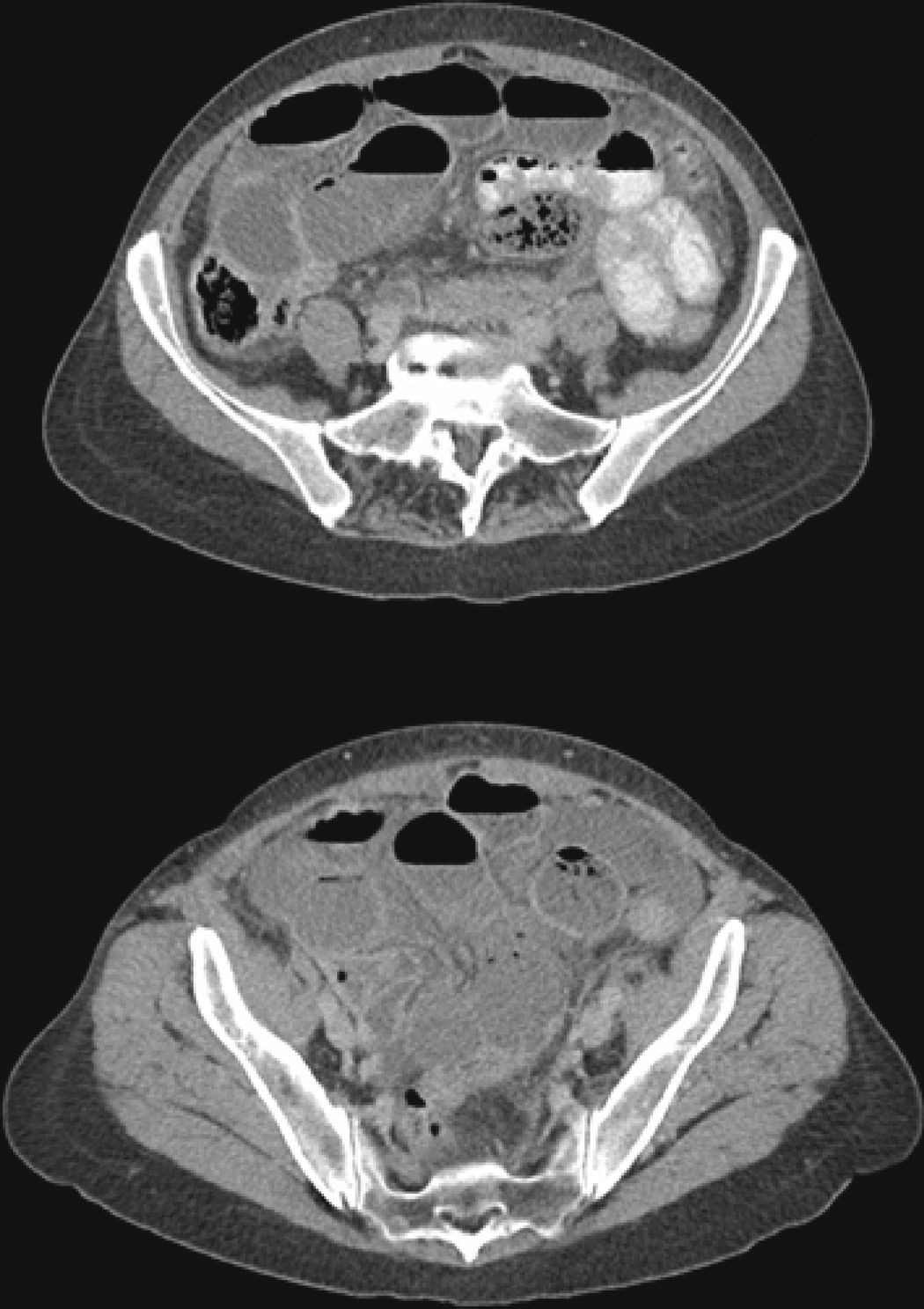
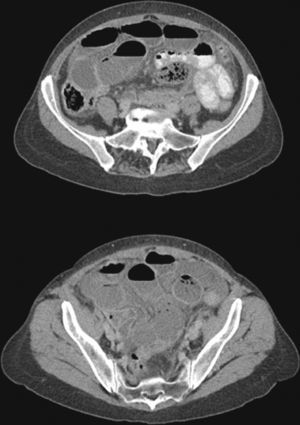
A 59-year-old female patient attended the emergency room of our hospital reporting continuous pain in the right side of the abdomen with colic-like exacerbations lasting for 72h, dysthermic sensation and chills, nausea, bile-stained vomiting, and no defecation during the episode. Her personal history included no surgery or abdominal or pelvic trauma, nor prior chronic or intermittent abdominal symptoms. Five months earlier she had undergone total thyroidectomy for a 15-mm unifocal papillary thyroid carcinoma, and seven days before attending the emergency room she had received ablation therapy with 131I in a hypothyroid state (TSH 58mIU/L, undetectable FT4) after the discontinuation of suppressing levothyroxine treatment for four weeks. A whole body scan performed after ablation showed thyroid bed uptake only. On physical examination, the patient was afebrile and hemodynamically stable, but had a poor general status. An abdominal examination revealed decreased air-fluid sound and generalized bloating in a distended and diffusely tender abdomen with no masses or visceromegalies and with signs of peritoneal irritation. The only remarkable result of laboratory tests performed in the emergency room was leukocytosis (17,070cells/mm3) with 94% neutrophils. An abdominal CT scan (Fig. 1) showed a dilatation of the small bowel loops from the jejunum to the ileum except for the distal 20–30cm, where a change in size with no identifiable cause was seen, intraperitoneal free fluid, and a gastric cavity distended with oral contrast. Based on these findings, an exploratory laparotomy was performed, revealing dilated small bowel loops up to the distal ileum, which was rotated and obstructed by a congenital web that caused vascular compromise and signs of non-reversible intestinal ischemia. A resection of 15cm of the compromised ileum was performed, followed by side-to-side anastomosis and abdominal cavity washing, and normal retrograde emptying of loops was seen with no other findings. At the histopathological examination, a small bowel segment with ischemic necrosis and signs of severe peritonitis was found. The early postoperative course was uneventful, and food tolerance and oral levothyroxine treatment started at 72h. Since surgery, the patient has not had new abdominal symptoms or evidence of any persistence or recurrence of thyroid neoplasm.
To our knowledge, no case has been reported where these two rare conditions concur: paralytic ileus secondary to hypothyroidism after discontinuation of levothyroxine treatment for administration of 131I in a patient with DTC, which leads to incarcerated intestinal hernia on a previously unknown and asymptomatic congenital web. Increased oral-cecal transit time,4 decreased esophageal persistalsis,5 slower gastric emptying,6 and bowel hypomotility mainly affecting the large bowel4 occur in hypothyroid patients. These symptoms are usually mild and improve with the administration of levothyroxine.7 However, severe, prolonged hypothyroidism may be associated with paralytic ileus or pseudo-obstructive conditions reversible with hormone treatment,8 and may very occasionally lead to intestinal ischemia that may, in turn, occasionally be fatal.9 The underlying cause of this hypomotility has yet to be elucidated. Colonic atony may be mediated by two mechanisms: submucosal myxedematous infiltration with separation of muscle fibers of the lymph nodes of Auerbach's plexus,8 and a severe autonomic neuropathy of extrinsic nerve fibers of the colon and myenteric plexus.9
Intestinal obstruction by a congenital web originating from embryonic structures such as the vitelline duct, artery and veins, and the urachus, or from an abnormal coupling of peritoneal layers during embryogenesis10 is uncommon in children and exceptional in adults.11 This represents a significant diagnostic dilemma before surgery due to its low frequency, but should be considered in differential diagnosis of any patient with an obstructive condition and an unremarkable abdominal history. The most common location is between the ascending colon and the terminal ileum, followed by the Treitz ligament and the terminal ileum,10 and may cause both small bowel strangulation and abdominal pain in patients with functional bowel disease. There are no specific imaging tests, but CT, MRI, and barium meal tests, if feasible, suggest diagnosis. Diagnostic-therapeutic surgical treatment using open laparotomy or laparoscopy consists of resection of the web and the necrotic bowel segment. In our patient, bowel dilatation and atony caused by hypothyroidism triggered torsion and incarceration of the proximal bowel segment over the congenital web axis, requiring surgical resection of the necrotic segment.
To sum up, an exceptional and potentially fatal complication of preparation in a hypothyroid state for 131I ablation therapy in patients with DTC is reported. Differential diagnosis of an abdominal condition in a myxedematous patient should include the uncommon presence of a congenital web unmasked by bowel hypomotility caused by hypothyroidism.
Please cite this article as: Luque-Ramírez M, Gómez Ramírez J, Azcárate Villalón A, Martín Pérez E, Larrañaga Barrera E. Efecto adverso excepcional de la suspensión del tratamiento con levotiroxina para la ablación con I-131 del remanente tiroideo en una paciente con cáncer diferenciado de tiroides. Endocrinol Nutr. 2013;60:412–414.