The solitary fibrous tumors (SFTs) are infrequent, distinct neoplasm of mesenquimal origin, usually of intrathoracic localization, originating in the pleura.1 Extrathoracic SFTs are rare, most of them reported in the upper respiratory tract, orbit and extremities. Intraabdominal and particularly retroperitoneal SFTs are very infrequent.
The usual clinical expression is due to the compressive effect. Nevertheless, in very few cases they produce active peptides/hormones. So far, SFTs producing insulin-like growth factor (IGF)-1 and IGF-2 have been described.2,3 Most of the cases encountered “big” IGF-2, a precursor of IGF-2, to be associated to recurrent hypoglycemia. We present the first case of non-islet cell tumor induced hypoglycemia caused by metastatic, multiple, recurrent, intraabdominal solitary fibrous tumors. The patient reported multicentric papillary thyroid carcinoma and thymus hyperplasia.
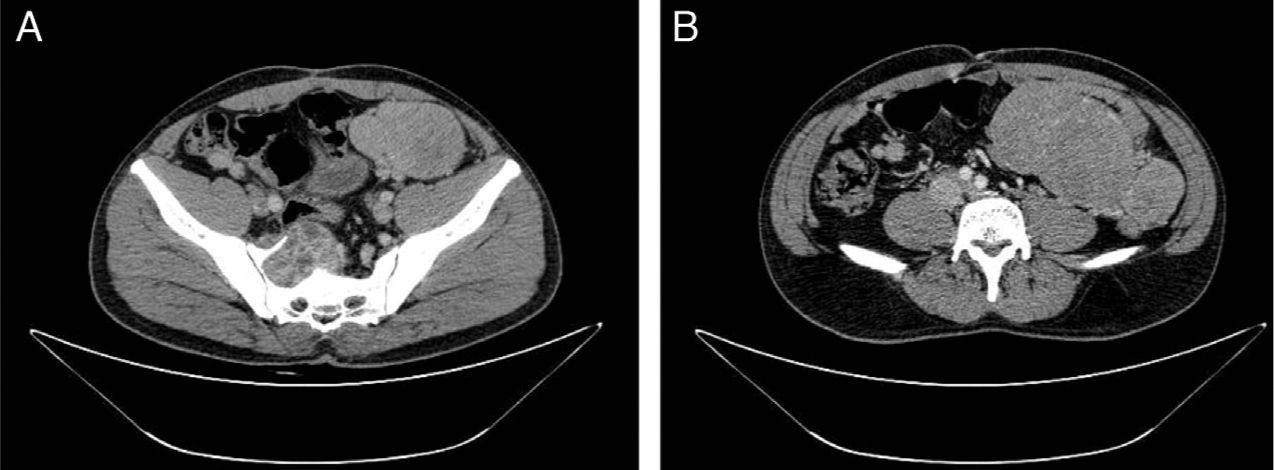
A 32-year-old man, with a history of a surgical excision of a 10-cm retrovesical SFT 9 years ago, was admitted to the emergency department in December 2009 with a Glasgow coma scale score 8 and capillary blood glucose of 25mg/dl. He presented a complete recovery after endovenous glucose administration. In the previous 8 months he referred nervousness, tremors and sweating during fasting conditions, and rhinophyma, hoarse voice, and a palpable cervical node of rapid growth. In the emergency room the following data were recorded: blood pressure 131/78mmHg, heart rate 77/min, height 1.71m, weight 80kg, and body mass index 27.35kg/m2; he was afebrile, with a normal physical examination, except for: (a) acromegalic facial appearance, (b) right cervical node, of approximate 3cm, (c) palpable superficial abdominal mass of approximately 10cm in the left lower quadrant. The electrocardiogram and chest X-ray were normal. Plain abdominal X-ray showed an image suggestive of left lower quadrant occupation. He had normal blood test (routine biochemistry and hemogram). He tested negative for anti-insulin antibodies and sulfonylureas. In the presence of hypoglycemia, levels of insulin, C-peptide, growth hormone and IGF-1 were undetectable. Oral glucose tolerance test showed very low insulin response. Controlled induced hypoglycemia showed a total deficit of growth hormone. The rest of the pituitary hormonal axis was unaltered. IGF-2 levels were 2974ng/dl, (144–3000ng/dl), with a ratio IGF-2/IGF-1 >118,96, suggestive of non-islet cell induced hypoglycemia by IGF-2. An abdominal and pelvic computerized tomography scan (Fig. 1) showed multiple intraabdominal tumors, the biggest of 9×11, with 5cm invading the sacrum. In addition, the extension study showed a thymus hyperplasia. The patient underwent incomplete debulking surgery on June 2010, with remnant intrasacral tumors. All of them were malignant solitary fibrous tumors. Quantitative real-time PCR (protein chain reaction) of tumor showed high amounts of IGF-2 mRNA and the immune electrophoresis evidenced high amounts of “big”-IGF-2 in both the serum and the tumor. After the surgical intervention and radiotherapy sessions, big-IGF-2 was no longer detected in the serum and he presented with a normal IGF-2/IGF-1 ratio (<10).
A total thyroidectomy was also performed, showing bilateral multiple papillary thyroid carcinoma, with capsular and vascular invasion. Radioiodine therapy was given. At 2 years follow-up he presented with a significant reduction of the remnant intraabdominal tumors and the radioactive iodine whole body scan was negative. He was normoglycemic and had normal facial appearance.
The incidence of hypoglycemia associated with the SFTs and its mechanisms are still to be elucidated. Classically, since it was first postulated in 1988 by Daughaday et al.,4 it is considered that non-islet cell induced hypoglycemia is due to large amounts of IGF-2. A high-molecular-weight IGF-2 (big IGF-2), most likely an incompletely processed IGF-2, is present at elevated levels in some SFTs. So far, the increased production of “big-IGF-2” was demonstrated in 3 patients with intraabdominal SFT. Our case is the first that associates hypoglycemia and other solid tumors (papillary thyroid carcinoma, thymus hyperplasia and a pituitary non-functional adenoma).
There is recent evidence of the involvement of the IGFs system in malignancies. In vitro studies have shown that in many tumors including SFTs the predominant receptor of the IGF system is the fetal isophorm of the insulin receptor (IR-A). There is evidence of the predominance of the IR-A in thyroid papillary cancer and a local autocrine loop IGF-2/IR-A,5 which could explain the multicentric, rapid growing papillary thyroid cancer of our patient. All the members of the insulin-gene family are present in the thymus, and only IGF-2 has an important role in thymopoiesis.6 This patient presented with thymus hyperplasia which we believe was due to prolonged exposure to high levels of IGF-2 and its precursors.
This is the first case-report of non-islet cell hypoglycemia due to a recurrent metastatic retroperitoneal SFT becoming clinically evident after 9 years from the first surgical intervention. The high levels of “big-IGF-2” were associated with acromegalic appearance, high risk papillary thyroid carcinoma of rapid growth and thymus hyperplasia, suggesting the relation between the IGF-system and tumor growth.
Conflict of interestThe authors have nothing to declare.
Special thanks to Dr. Marta García for the Western blot and quantitative real-time PCR analysis.