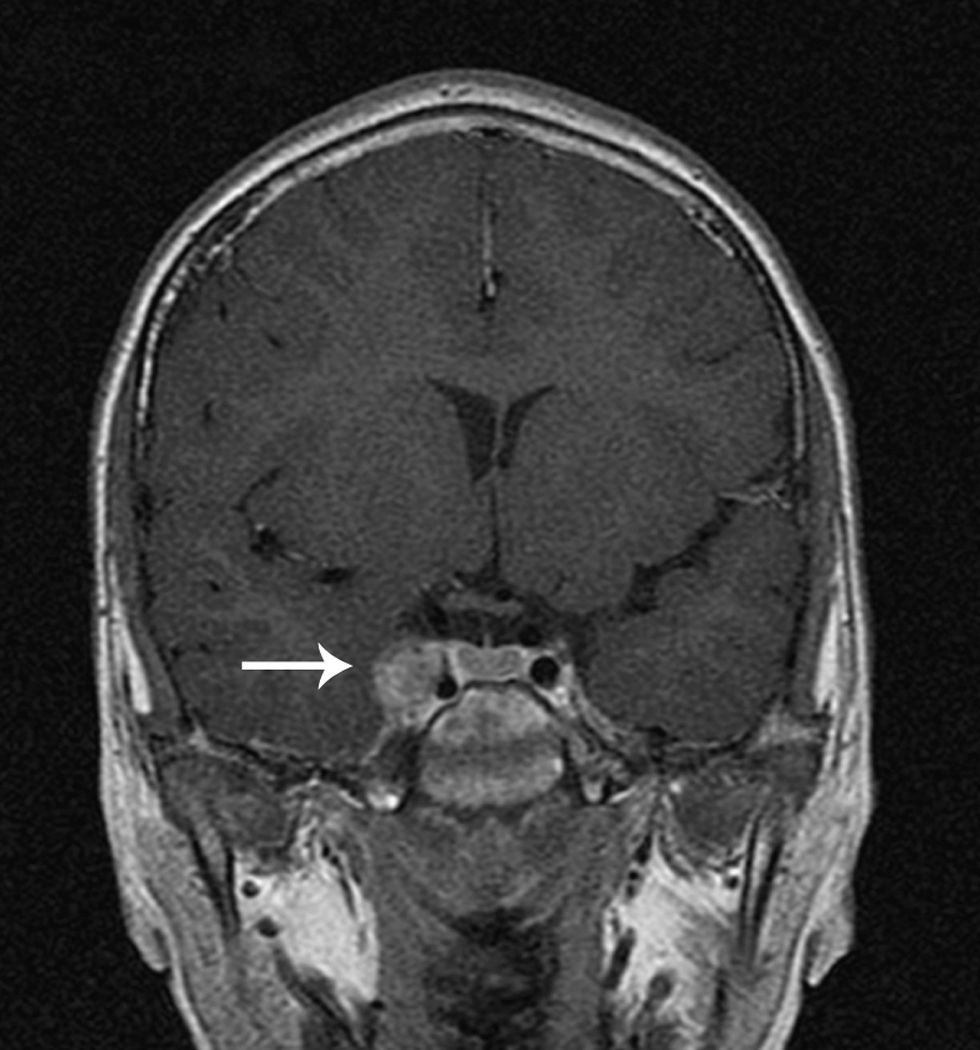
A previously healthy 9-year-old girl, born in Colombia and living in Spain for the last two years was admitted to our hospital with a 5-day history of fever and shivers. Physical examination at admission showed a sick-appearing girl, with nuchal rigidity, respiratory distress and a furuncle on her right shoulder. Bilateral peripheral nodular infiltrates were seen on chest X-ray. Laboratory results revealed neutrophilia, microcytic anemia, hyponatremia, C-reactive protein level of 20.6mg/dL and infectious consumption coagulopathy. Cerebrospinal fluid (CSF) examination was normal. A diagnosis of bacteriemia with pneumonia was suspected, and cefotaxime was started. Community-associated methicillin-resistant Staphylococcus aureus (CA-MRSA) grew in the blood culture. Genetic molecular analysis detected the Panton-Valentine leukocidin gene. Vancomycin was added to the initial treatment, but was changed to teicoplanin due to an allergic reaction. The patient was discharged on day 8, with clindamycin and cefuroxime treatment, but 20h later was readmitted with right ptosis, sixth cranial nerve palsy, and worsening headache. Cerebral magnetic resonance imaging (MRI) showed right cavernous sinus thrombosis and intracavernous internal carotid artery arteritis. Chest CT scan evidenced bilateral necrotized peripheral nodules, apparently corresponding to septic emboli. Retinal examination and echocardiography were normal. Cefotaxime and teicoplanin were reinitiated and enoxaparin and oral acenocoumarol were added. On day 14 teicoplanin was switched to linezolid because the patient showed no clinical improvement, and was completed at 8 weeks. Four months after discharge, MRI demonstrated an absence of thrombosis and a pseudoaneurysm-like image at the intracavernous right carotid artery (Fig. 1). The latest MRI, 8 months after discharge, showed a significant improvement, with a residual image of the pseudoaneurysm detected in the previous MRI. In the study of contacts, two members of her family proved to be MRSA carriers.
MRSA is an emergent pathogen and the most common cause of skin and soft tissue infections. In 2005, the estimated incidence rate of invasive infection by this pathogen in the United States was 31.8 per 100 000.1 Panton-Valentine leukocidin is a cytolytic toxin produced by CA-MRSA and is associated with furuncles and necrotizing pneumonia,2,3 as was seen in our case. In 2008, 4 cases of MRSA (21% of all S. aureus infections) were isolated in our pediatric department and two corresponded to bacteriemia.
Cerebral sinus thrombosis mainly affects immunocompromised patients or patients with acquired prothrombotic conditions, but can also affect children, as has been reviewed by DeVeber and Wasay.4,5 Our patient was a previously healthy child without prothrombotic conditions and no infection in the area responsible for venous drainage of the cavernous sinuses. MRI is the most sensitive and specific examination technique for this disease, since contrast-enhanced computed tomography (CT) will miss diagnostic features in about 40% of patients.4 Antibiotics have had the greatest impact on the prognosis of septic cavernous sinus thrombosis. When MRSA is isolated, high doses of vancomycin, teicoplanin or linezolid are recommended.6 Anticoagulant treatment in adults appears to be safe and is associated with a potentially substantial reduction in the risk of death, which does not reach statistical significance according to a Cochrane review.7 A trial conducted by deVeber in pediatric patients also concluded that low molecular weight heparin may play a role in the treatment of sinus venous thrombosis.8 We treated our patient with low molecular weight heparin because of progression of the local symptoms, despite effective antibiotic therapy (resolution of fever and respiratory symptoms).
To our knowledge, this is the first reported case of cavernous sinus thrombosis caused by CA-MRSA in a child as a complication of a distant infection, although previous reports of invasive MRSA affecting the cavernous sinus have been described in adults.9,10 The pediatric population may be affected when an adult, usually a family member, is a carrier of the microorganism. Considering the high morbidity and mortality related to this disease, the favorable recovery achieved in this patient is noteworthy.