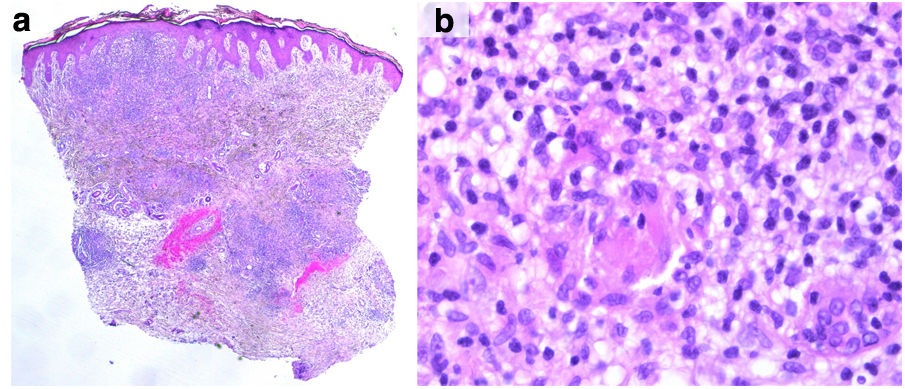
A 68-year-old Caucasian man with a history of Crohn's disease, taking azathioprine and adalimumab for 4 years, presented to our outpatient dermatology clinic with a two-month history of pain, edema, and erythema of the left-hand middle finger. The patient used to take care of his aquarium and a bonsai without wearing gloves, therefore having suffered a small traumatic wound on this finger caused by a dead fish. He had no response to previous treatment with amoxicillin-clavulanic acid, cotrimoxazole, and valacyclovir. Physical examination revealed an inflamed crusted lesion on the third left finger and multiple cutaneous papules, distributed in a sporotrichoid pattern on the back of his left hand, and on his third, fourth, and fifth finger (Fig. 1a). There was no enlargement of lymph nodes or involvement of other internal organs. Left-hand x-ray excluded osteomyelitis. Skin biopsy revealed a dermal infiltrate of lymphocytes and plasma cells surrounding epithelioid granulomas with giant multinucleated cells (Fig. 2). Gram, periodic acid-Schiff, Grocott, and Ziehl-Neelsen stains were negative. Mycobacterium (M.) marinum was isolated from a skin biopsy in solid cultures and confirmed by polymerase chain reaction and DNA sequencing (Fig. 1b).
The patient started treatment with ethambutol 2g and rifampicin 600mg once daily. Beyond that, adalimumab was discontinued and replaced by ustekinumab due to a persistent lack of control of Crohn's disease. After 6 months of therapy, there is complete resolution. The patient completed 9 months of therapy due to immunosuppressive therapy performed for Crohn's disease.
Closing remarksM. marinum is a non-tuberculosis mycobacterium that can cause granulomatous skin infections. It is an endemic fish pathogen found in fish tanks, swimming pools, and natural bodies of water.1–3 It clinically presents as a solitary papulo-nodule at the inoculation site, which may ulcerate and spread in 20% of the cases in a sporotrichoid pattern (lymphangitic spread) following minor trauma and exposure to contaminated water or from direct contact with fish or shellfish.1,4 Because its optimal temperature for growth is around 30°C, cutaneous lesions most frequently occur in the upper or lower extremities and sometimes on the tip of the nose.3–5 Tumour necrosis factor (TNF) alpha plays an essential role in granuloma formation and mycobacterial growth restriction within macrophages. Thus, patients taking anti-TNF agents are at increased risk for granulomatous infections such as M. marinum. Most of these patients had infections confined to the skin and subcutaneous tissue, often in a sporotrichoid distribution, as in our case. However, immunocompromised patients may show severe and disseminated disease with deep infections such as tenosynovitis, osteomyelitis, and septic arthritis.2,3,5 Cutaneous lesions are often misdiagnosed as furunculosis, sporotrichosis, pyoderma, cutaneous leishmaniasis, tuberculosis primary complex, and sarcoidosis.3,5 Despite the availability of diagnostic tools, such as tissue cultures, PCR, and histology, the diagnosis of M. marinum is challenging. Culture provides a definitive diagnosis of M. marinum, but it is positive in only 70–80% of cases.2,5 By standard susceptibility testing, M. marinum isolates are susceptible to rifampicin, rifabutin, ethambutol, clarithromycin, sulfonamides, trimethoprim-sulfamethoxazole, doxycycline, and minocycline. American Thoracic Society and Infectious Diseases Society of America (ATS/IDSA) statement and recommendations advocate the treatment with two active agents until 1–2 months after resolution of symptoms.1,3,4 Patients taking anti-TNF agents often require a more extended multidrug regimen or even surgical intervention, with an average course of treatment over 6 months to 1 year.2,3 Attention must be paid to the interruption of TNF-alpha inhibitor treatment so as to hasten resolution and should be determined on a case-by-case basis.2,3 In this case, biological therapy with an anti-IL-12/IL-23 was successfully maintained during antibiotic therapy. Due to the increasing use of biologics, M. marinum infections should always be included in the differential diagnosis of cutaneous infections in immunocompromised patients.
Funding sourceThis article has no funding source.
Conflict of interestThe authors have no conflict of interest to declare.
We thank the Professor José Cristino, Director of the Clinical Pathology Laboratory of Centro Hospitalar Universitário Lisboa Norte, to the Microbiology Laboratory, under the direction of Dr. Luís Marques Lito, and to doctors Carlos Ribeiro and Leonardo Carneiro, for identifying and photographing the culture of mycobacterium marinum, which was crutial to make this diagnosis.