Over a number of years now, the introduction of point-of-care ultrasound has become widespread in different medical and surgical specialities. This term refers to an ultrasound performed and interpreted by the doctor responsible for the patient.1 It is easy to apply with short learning curves, and allows immediate, concrete clinical information to be obtained.2 There is a wide range of recognised applications in the Accident and Emergency Department which offer great benefits in advanced capability for both diagnosis and monitoring of response to therapy.3
We present here the case of a 32-year-old female patient, 13 weeks pregnant, with no relevant previous medical history is presented. She described a one-week history of pain in the right maxillary region, nasal congestion, foul-smelling rhinorrhoea and documented pyrexia of up to 37.9°C which did not improve despite symptomatic treatment with paracetamol 650mg/8h.
On physical examination, she was found to have pain on palpation of the right maxillary region which increased with postural changes. There were no significant abnormalities in the rest of the examination.
With the physical examination findings and the symptoms reported by the patient, the initial suspicion was acute sinusitis. As the patient did not wish to start antibiotic treatment without diagnostic confirmation and as she was pregnant and did not wish to have a maxillary sinus X-ray, she was offered the possibility of a point-of-care ultrasound.
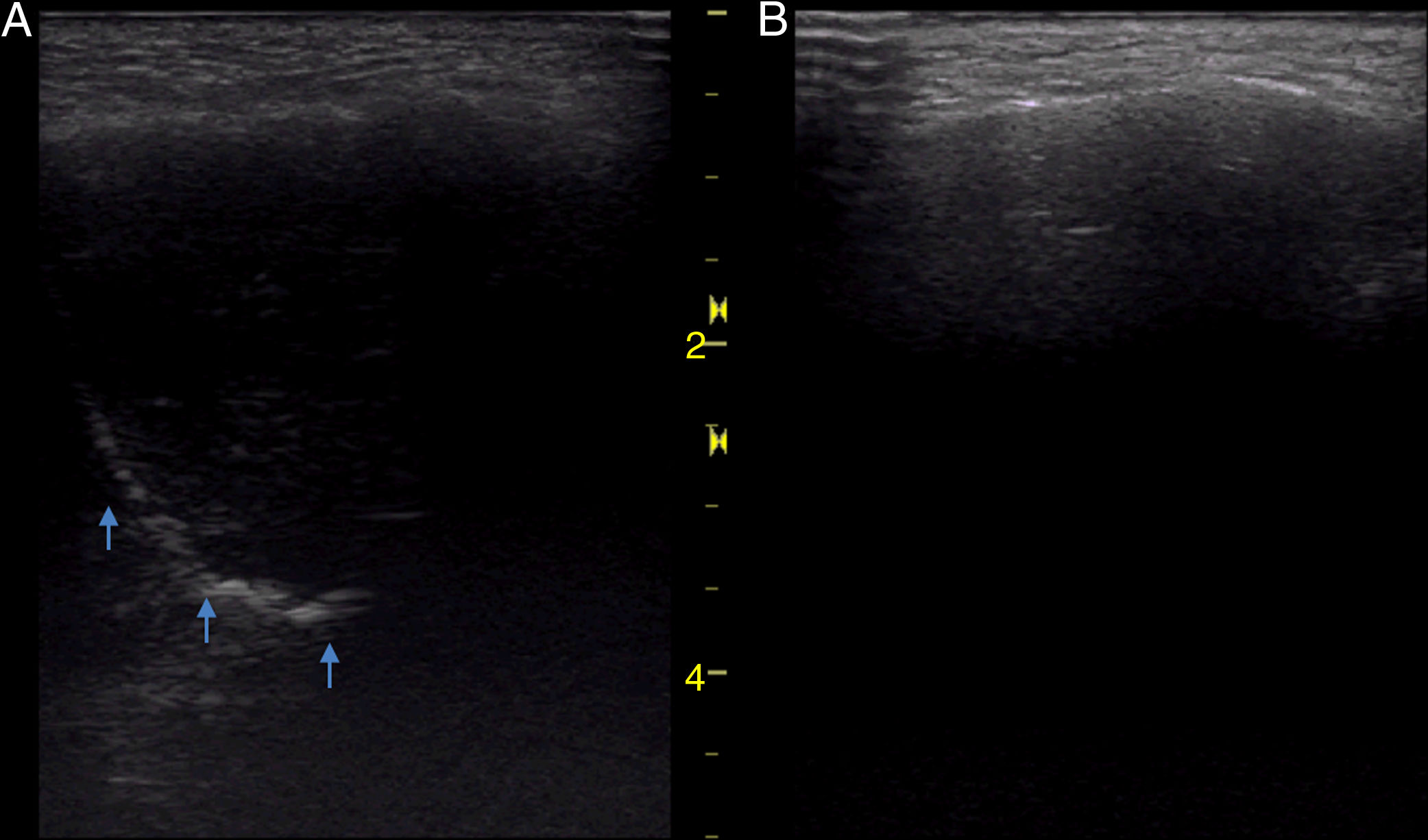
The ultrasound in the area of the right maxillary sinus (Fig. 1A) revealed the presence of a “sinusogram”, confirming the suspicion of acute sinusitis. The patient was prescribed antibiotic treatment with amoxicillin 750mg/8h for 10 days. From day two of treatment, she reported significant clinical improvement.
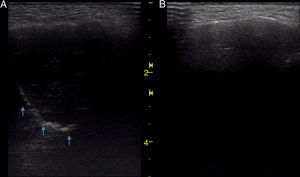
Right maxillary sinus, longitudinal section with linear probe in the area of greatest sensitivity. (A) A “sinusogram” sign (arrows) can be seen delimiting the posterior wall of the maxillary sinus, which has echogenic content inside. (B) Two weeks later, in the same location, disappearance of the sinusogram.
After completing the treatment, a repeat ultrasound scan was performed in the same position as the first (Fig. 1B) and showed the disappearance of the sinusogram.
Acute sinusitis consists of infection of the paranasal sinuses, either of viral or bacterial origin. The pathophysiological mechanism involves three fundamental factors: obstruction of the sinus opening, reduced mucociliary clearance and an increase in the viscosity of the secretions. It is most common for the infection to be located in the maxillary sinus and aetiology is predominantly viral, but in 0.5–2% of the cases, it can be complicated by a bacterial superinfection.4,5
Diagnosis is essentially clinical and should be supported by physical examination, consisting of palpation of the sinus areas. However, it does require a high degree of clinical suspicion. Imaging tests are not usually required for diagnosis, with their use reserved for searching for complications.4,5
When a patient presents with a clinical respiratory infection lasting seven days and two or more of the following: purulent nasal exudate, poor response to decongestants, facial pain or pain in sinus areas which is aggravated by postural changes or the Valsalva manoeuvre, headache and fever, we should suspect acute sinusitis.
The main aim of treatment is to drain the contents of the sinuses by measures such as humidifying the environment, nasal corticosteroids or heat over the sinus and symptomatic treatment. The use of antibiotics should be reserved for patients who do not improve after seven days of symptomatic treatment or when they have serious symptoms or complications.
The sinus X-ray (mainly the specific Waters projection for the maxillary sinus) would show a thickening of the mucosa, with opacification of the sinus or air-fluid levels, but it has a low sensitivity and specificity.4,5 Although it is more sensitive than physical examination, the use of plain X-ray in the diagnosis of acute sinusitis is not cost-effective in the initial management.
Ultrasound of the paranasal sinuses is a quick, simple and non-invasive examination. The procedure is painless, can be repeated without limits, is easy to interpret and does not emit radiation. This technique has shown a high sensitivity (>86%) and specificity (>96%) much higher than X-ray for determining the presence of exudate from the maxillary sinuses. Among its limitations is that it is not possible to examine the ethmoid and sphenoid sinuses.
We consider ultrasound to be an aid in the diagnosis and follow-up of acute sinusitis, as well as a guide in the differential diagnosis of other common disorders, such as headache, rhinitis or conditions of odontogenic origin.
Conflicts of interestThe authors declare that they have no conflicts of interest.
Please cite this article as: Arenas-Berenguer I, Tung-Chen Y, Alonso González B. Utilidad de la ecografía clínica en el diagnóstico y seguimiento de la sinusitis aguda. Enferm Infecc Microbiol Clin. 2020;38:508–509.