Necrotising fasciitis (NF) is a serious infectious disease that results from the progressive involvement of muscle fascia and subcutaneous fat. Initially, the skin and subcutaneous cell tissue are not altered, which makes diagnosis difficult, so clinical suspicion is vitally important.1 The diagnosis confirmation of this entity is established with surgical exploration, visualising fascia and muscle planes.1,2
Radiological examinations are of diagnostic help, but they shouldn't delay surgery in cases of high clinical suspicion.3 Computed tomography (CT) is currently considered the initial radiological test of choice. Clinical ultrasound performed by the physician responsible him/herself is submitted as a valid alternative to confirm or rule out multiple diseases and thus guide us in the differential diagnosis. It is a fast, inexpensive, safe and reproducible test.4 The availability of ultrasound scanners in hospital emergency departments (A&E) makes it possible to speed up waiting times in the diagnostic process and make integrated decisions with the clinical picture.4
We present the case of a 68-year-old woman who was brought to our A&E due to a low level of consciousness for 12 h prior. As relevant history, she had chronic lower back pain and had undergone surgery 4 years earlier, for which she was taking 1 g/every 8 h, tramadol 50 mg/every 8 h and clonazepam 0.5 mg/every 12 h. She attended A&E due to low consciousness, which according to relatives occurred after increasing the intake of dexketoprofen 25 mg, tramadol 75 mg/every 8 h and clonazepam 1 mg/every 12 h prescribed for poor pain control after suffering a fall with trauma to the left hip 7 days earlier.
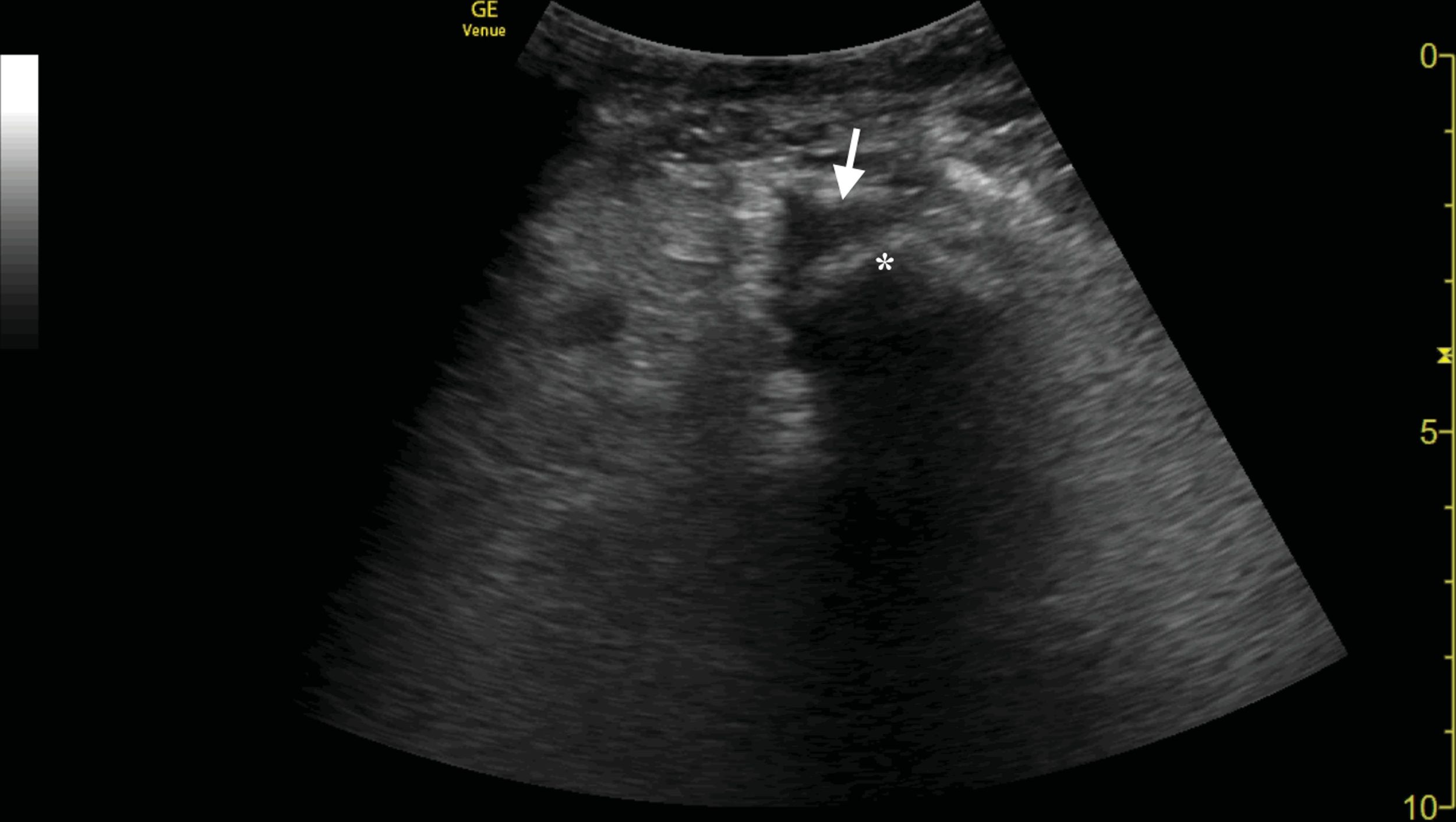
Physical examination showed poor general condition, disorientation, with a Glasgow score of 10 (E2V3M5), blood pressure of 123/55 mmHg and 109 bpm, slight abdominal bloating, and a volume increase in the lower left limb was striking. The rest of the exploration did not reveal significant findings. Lab tests revealed leukocytosis of 16.1 × 103/µl (normal: 4.5–11), acute hyponatraemia of 120 mEq/l (normal: 135–145), raised direct bilirubin of 3.23 mg/dl (normal: < 0.3), slightly elevated CPK of 216 UI/l (normal: < 175), elevated C reactive protein 374.6 mg/dl (normal: 0–3) and procalcitonin (5.34 ng/dl; normal: < 0.5). Previously, a lower limb angio-CT was requested. While waiting for this additional test, a clinical ultrasound of the left lower limb was performed, showing an absence of signs of thrombosis in the femoral vein, as well as significant "cobblestone" oedema of the subcutaneous cellular tissue of the thigh, with fluid collection around the femur (Fig. 1). These findings were subsequently confirmed by angiogram, which revealed the presence of abscesses in the extensor compartment of the left thigh, consistent with a soft tissue infection, so urgent surgery was performed due to suspected NF. A microbiological sample of the surgical wound isolated Streptococcus intermedius, and antibiotic therapy with ceftriaxone 2 g/every 24 h was started during admission, later scaling down to levofloxacin 750 mg oral/every 24 h, with subsequent good evolution in follow-up in outpatient consultations.
Conducting clinical ultrasound in the presence of an exploratory finding such as an increase in limb volume can confirm or rule out the presence of urgent diseases safely and quickly. Although NF is a rare entity, it has a mortality of 70-80%, being a vital disease,5 whose main predictor is the delay in the diagnosis.
The characteristic ultrasound findings of FN include the presence of air, hyperechogenicity, and "cobblestone" oedema of subcutaneous cell tissue. The sensitivity of ultrasound for the diagnosis of NF is 88.2% and specificity is 93.3%.6 However, it has a series of limitations to keep in mind, such as lack of resolution at the level of deep structures or oedema and hyperechogenicity that can also be detected in situations of venous insufficiency and anasarca.7 Given the potential seriousness of this entity, in the face of clinical suspicion, a surgical exploration is necessary.
This clinical case is illustrative of the multiple advantages of clinical ultrasound performed by the emergency physician. It is fast, harmless, low cost and does not involve radiation, making it an ideal initial screening technique in complex cases. In our case, it was aimed at the early diagnosis of NF compared to other less plausible diagnoses (benzodiazepine poisoning, hip fracture, haematoma, or intra-abdominal disease). For all these reasons, it is essential to generalise this training, in order to improve the prognosis of this devastating disease.
Please cite this article as: Tung-Chen Y, Algora Martín A, Romero Gallego-Acho P. La utilidad de la ecografía clínica ante lasospecha de fascitis necrosante. Enferm Infecc Microbiol Clin. 2020;38:457–458.