A 30-year-old male patient with sexually acquired human immunodeficiency virus (HIV) infection (sex with men), stage B2, was receiving treatment with emtricitabine/rilpivirine/tenofovir disoproxil fumarate with good virological and immunological control (CD4 count 845 cells/mm3 and undetectable viral load). Notable elements of his personal medical history included prior gonococcal and syphilis infection. He had received appropriate treatment for both sexually transmitted infections (STIs).
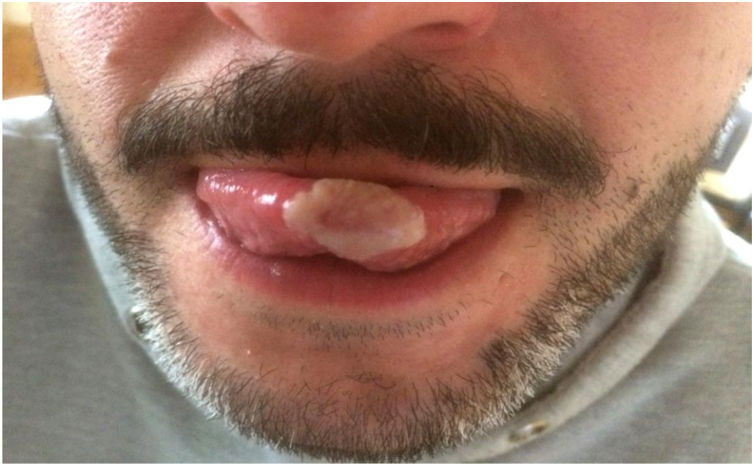
He came to the infectious diseases unit due to the appearance of a painful whitish lesion on the tip of the tongue (Image 1) three days earlier, with no accompanying lesions in the genital region or elsewhere. He denied having fever, chills, dysphagia or urethral discharge. Physical examination revealed a rough, oval-shaped lesion on the apex of the tongue, extending towards the left half of the tongue and both tongue surfaces, that did not come off when scraped. No locoregional lymphadenopathy or other lesions of the oral mucosa or genitals were detected, and the patient’s physical examination was otherwise normal. In the appointment, blood tests were performed, a sample of the tongue lesion was taken for microbiological analysis and a urine sample was taken for STI screening.
A broad differential diagnosis should be made in HIV patients with high-risk sexual practices. It should include oral hairy leukoplakia, pseudomembranous candidiasis, human papillomavirus condyloma, post-traumatic ulcer, lichen planus, syphilis, coated tongue and neoplastic diseases (unlikely given the rapid onset of the lesion).
Clinical courseMicrobiological testing of the sample of the tongue lesion yielded a positive polymerase chain reaction (PCR) result for Chlamydia trachomatis (CT). Treatment was started with oral doxycycline 100 mg every 12 h for one week initially; this was prolonged to 21 days due the persistence of part of the lesion, resulting in complete subsequent resolution. All other microbiological results for STI screening in blood and urine were negative, and the blood tests performed revealed no significant abnormalities.
Closing remarksGenital infection with C. trachomatis is currently believed to be one of the most common STIs worldwide. It predominantly affects young people under 25 years of age. Various studies conducted in men who have sex with men (MSM) have identified significant rates of extragenital (oropharyngeal or rectal) infection with CT, with or without concomitant urogenital infection.1,2 For this reason, the Centers for Disease Control and Prevention (CDC) recommend routine urethral and anorectal examination for CT in MSM, while oropharyngeal screening is not recommended due to the low rate of oropharyngeal infection and because the clinical significance of the involvement of this site is unknown.3 In men, the primary clinical sign is urethritis, while in women, it is cervicitis. Proctitis, pharyngeal infections and conjunctivitis have also been reported. However, 1%–25% of infections in men are asymptomatic4–6; this figure has been found to be as high as 100% in the case of oropharyngeal infections.2,7,8 This wide variability could be due to the different diagnostic techniques employed (culture, direct immunofluorescence or nucleic acid amplification tests) or the sample site. Symptomatic pharyngeal infections tend to manifest as pharyngitis, localised lymphadenopathy or inflammation of the oral cavity5; other forms of presentation are rare. We conducted a review of atypical forms of presentation in the PubMed database using English terminology and were unable to find reported cases in the literature of infection with CT presenting with a whitish lesion of the oral mucosa, as in our case.
In conclusion, although oropharyngeal infection with CT is asymptomatic in most patients, it should be taken into consideration in patients with high-risk sexual practices and included in the differential diagnosis of white lesions of the oral mucosa.
Please cite this article as: Vázquez-Temprano N, Casal Lorenzo J, Rodríguez García JC, Diz Arén J. Lesión blanquecina en vértice lingual en paciente con virus de inmunodeficiencia humana. Enferm Infecc Microbiol Clin. 2021;39:413–414.