Invasive fungal infections (IFIs) are primarily caused by Candida spp. and Aspergillus spp. However, there are some emerging fungi such as Geotrichum capitatum (now Saprochaete capitata) that are characterised by causing IFIs in immunosuppressed patients, primarily those with prolonged neutropenia and oncohaematological disease.1 Other risk factors, as in other fungal infections, are the presence of a central venous catheter (CVC), receiving parenteral nutrition, use of broad spectrum antibiotics, corticosteroid therapy, chemotherapy and disruption of the skin/mucosal barrier, with nosocomial outbreaks having been described and higher incidence in certain geographic areas such as Italy, France, Turkey and Spain.
There are published cases of IFI caused by Geotrichum spp. in oncohaematological paediatric patients,2–4 but there are few described cases of infection of immunocompetent patients,5 and none in the paediatric age group.
We present a case of catheter-related fungaemia due to Geotrichum capitum in a 4-month-old female infant, who presented a clinical picture compatible with bowel obstruction, and so underwent emergency surgery. In the postoperative period, she was admitted to ICU, a CVC was placed and treatment continued with ceftriaxone and metronidazole. She required parenteral nutrition for 13 days. On the 7th postoperative day, she presented fever, with Enterococcus faecalis being isolated in the surgical wound, so the antibiotic treatment was switched to piperacillin-tazobactam. The patient was operated on again for an omental hernia and presented irritability and fever at 48 h. Analytical and new microbiological samples (blood and peritoneal fluid cultures) were taken and linezolid added to her treatment. With the fever persisting, it was decided to withdraw the CVC and it was sent for culture.
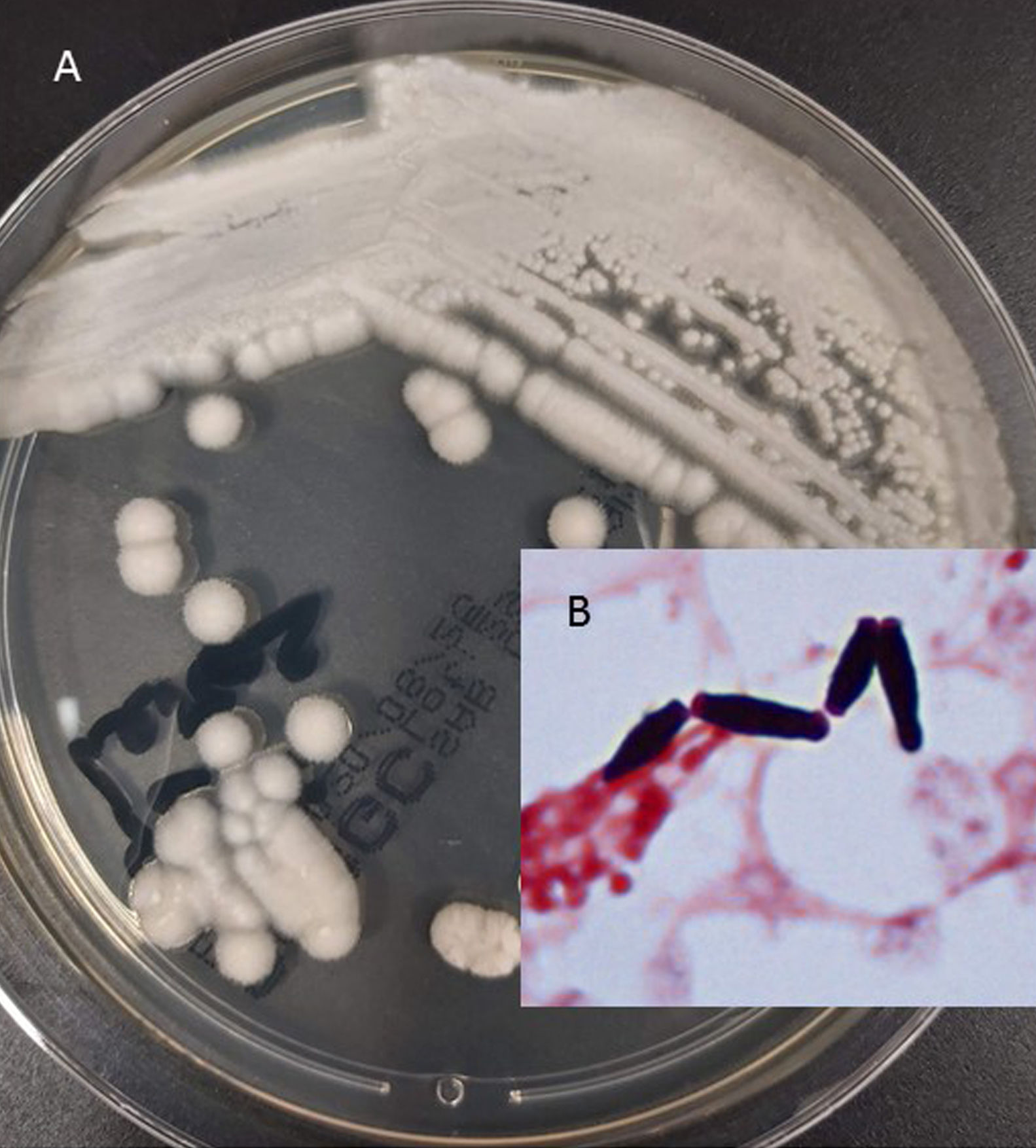
A levaduriform fungus was isolated in the culture from the tip of the catheter and in the blood cultures, so empirical treatment with fluconazole was initiated, then replaced with liposomal amphotericin B when the isolation of Geotrichum capitum was confirmed (Fig. 1 A, B). The extension study was negative, as was the galactomannan detection. The patient responded favourably with no microbiological isolation in follow-up blood cultures, and treatment was completed in 14 days. A cellular immunodeficiency study was carried out, with normal results, and the absence of neutropenia was confirmed. As a complication, after one week of treatment with amphotericin B, she presented hypokalaemia.
Geotrichum capitatum is an emerging fungus with a mortality rate over 70% in immunosuppressed patients. In this group of patients, the clinical presentation is similar to that of candidaemia, but with a higher frequency of disseminated disease.
An awareness of the fungus's pathogenicity and the host's immune response are essential tools for the management of these infections. Our patient had several predisposing factors, such as use of parenteral nutrition, broad spectrum antibiotics, a history of surgery and being fitted with a CVC. Because this fungus forms a part of the normal microbiota of the skin, digestive tract and respiratory tract, disruption of the mucosal or skin barrier could be considered a route of entry, with colonisation of the CVC and subsequent fungaemia. In spite of the high virulence and poor prognosis described, the good progress of our patient could be explained by her immunocompetent status, as well as the prompt removal of the CVC.
Diagnosis is generally performed through isolation in blood cultures. Fungi in the genus Geotrichum grow on Saboureaud agar with white colonies with a creamy appearance that can be confused with the genus Candida, but unlike the latter, on microscopic examination of the Gram stain, blastoconidia are observed to emerge from the arthroconidia in a "hockey stick" shape. The optimal growth temperature is 30°C. In general, Geotrichum spp. is a very asaccharolytic fungus, and Geotrichum capitatum in particular only ferments glucose and galactose, lacking even the ability to hydrolyse urea. Cases of cross-reactivity have been described in testing for the galactomannan antigen of Aspergillus spp.,4 something that did not occur with our patient.
There is no standardised treatment, but the administration of amphotericin B is recommended as high minimum inhibitory concentrations have been observed for echinocandins and fluconazole.6 In our case, Geotrichum capitatum presented minimum inhibitory concentrations similar to those described in the literature, with a favourable response after treatment with amphotericin B. Hypokalaemia, among others, is a side effect deriving from amphotericin B treatment, so it is important to monitor for this.
In conclusion, Geotrichum spp. is an emerging fungus that does not only affect immunosuppressed patients. For this reason, the risk must also be taken into account in immunocompetent patients with several predisposing factors for IFI.
Please cite this article as: Pastor-Tudela AI, Pérez-González D, Jiménez-Montero B, de Malet Pintos-Fonseca A. Fungemia relacionada con catéter por Geotrichum capitatum en una paciente pediátrica inmunocompetente. Enferm Infecc Microbiol Clin. 2021;39:363–364.