The genus Aerococcus spp. was described for the first time in 1953. It comprises eight different species, among which Aerococcus urinae and Aerococcus sanguinicola are the primary human pathogens, being associated with underlying disease in adults.1 However, they have been reported as rare causes of infection in the paediatric population. We report clinical and microbiological characteristics corresponding to three cases.
Case 1A 10-year-old boy visited the emergency department owing to a fever of 40 °C lasting 24 h associated with abdominal pain. Notably, he was found to have pain on palpation of his right flank, with painful fist percussion.
He had a history of admission when he was 25 days old due to a suspected febrile urinary tract infection (UTI), not confirmed microbiologically. A renal ultrasound revealed bilateral pyelocaliceal dilation. At 7 years of age, he was diagnosed with acute appendicitis. In the postoperative period, he was readmitted owing to fever and elevated acute-phase reactants, with normal urinalysis results. He was treated with piperacillin/tazobactam and responded favourably.
A urinalysis showed leukocyturia. A urine culture and blood testing revealed 14,259 leukocytes/mm3 and C-reactive protein (CRP) 22.6 mg/l. The boy was diagnosed with pyelonephritis and a decision was made to treat him with cefixime for 7 days. A renal ultrasound showed pyelocaliceal dilatation, distally tortuous right ureter and urinary retention.
Case 2A 5-year-old boy had erythema of the urinary meatus and whitish urethral discharge, with the rest of the examination being normal. A sample of the discharge was taken for culture and treatment was started with a topical corticosteroid. He was seen by his paediatrician 21 days later due to persistent urethral discharge, with no fever. He was prescribed topical mupirocin for a week, and his symptoms remitted.
Case 3An 8-year-old boy had colicky abdominal pain for 2 days and diarrhoeic stools. A urinalysis revealed microhaematuria, and a mid-stream urine culture was performed. He was prescribed fosfomycin tromethamine for 2 days, and his signs and symptoms disappeared. A subsequent renal ultrasound was normal.
Microbiology studyUsing previously described procedures,1,2 the urine cultures performed showed >100,000 colony-forming units (CFUs)/mL and >10,000 CFUs/mL of A. urinae for case 1 and A. sanguinicola for case 3. Abundant colonies of A. urinae alone grew in the urethral discharge culture. For the urine cultures, sensitivity to cefotaxime, ciprofloxacin, nitrofurantoin, penicillin and vancomycin was studied. For the urethral discharge culture, sensitivity to ampicillin, levofloxacin, linezolid, meropenem, rifampicin, tetracycline and vancomycin was studied. The micro-organisms were sensitive to all the antibiotics assessed.
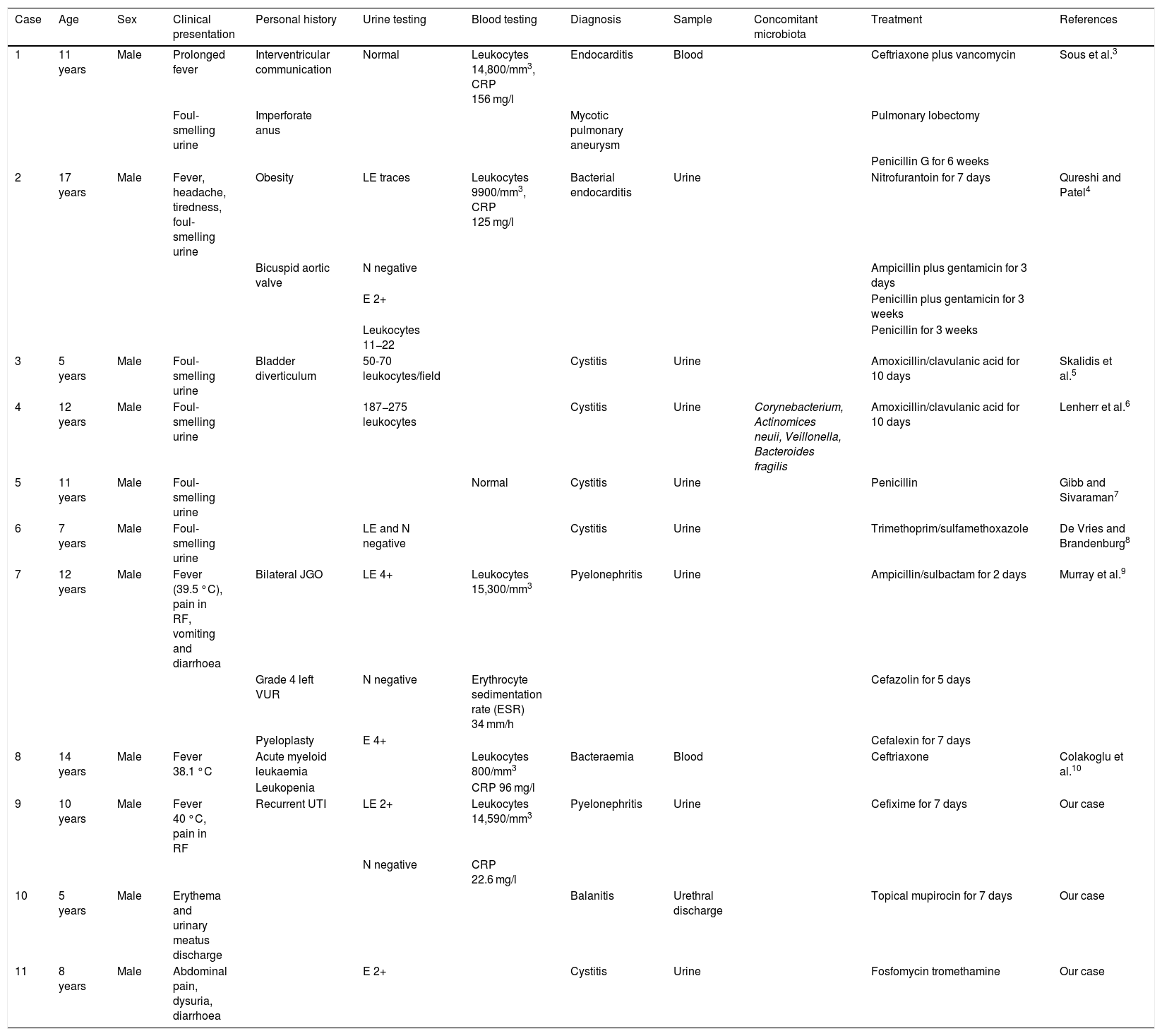
ConclusionsGenitourinary tract sample culture enables identification of unusual micro-organisms that may present in patients with risk factors. Two of these micro-organisms, which were recently described, are A. urinae and A. sanguinicola. Infection with these micro-organisms has been widely reported as a cause of potentially serious diseases (pyelonephritis, bacteraemia, endocarditis, peritonitis, etc.) in elderly patients with urinary tract infections, immune disease or systemic disease.1 In a review conducted in PubMed (7/2/2020), we found just 8 cases in patients 0–18 years of age (Table 1).3–10 Among them, 6 cases featured the notable finding of extremely foul-smelling urine and two presented endocarditis. Another corresponded to a case of pyelonephritis in a patient with vesicoureteral reflux who presented abdominal pain and fever.8 A case of bacteraemia in a 14-year-old patient with leukaemia was also reported.9 Patients were mostly adolescent or pre-adolescent males and generally received a late diagnosis. Case 2 in our series is notable for being the first reported case of balanitis caused by A. urinae.
Infections caused by non-viridans Aerococcus in paediatric patients published in PubMed up to 7/2/2020 and 3 cases reported in our article.
| Case | Age | Sex | Clinical presentation | Personal history | Urine testing | Blood testing | Diagnosis | Sample | Concomitant microbiota | Treatment | References |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 11 years | Male | Prolonged fever | Interventricular communication | Normal | Leukocytes 14,800/mm3, CRP 156 mg/l | Endocarditis | Blood | Ceftriaxone plus vancomycin | Sous et al.3 | |
| Foul-smelling urine | Imperforate anus | Mycotic pulmonary aneurysm | Pulmonary lobectomy | ||||||||
| Penicillin G for 6 weeks | |||||||||||
| 2 | 17 years | Male | Fever, headache, tiredness, foul-smelling urine | Obesity | LE traces | Leukocytes 9900/mm3, CRP 125 mg/l | Bacterial endocarditis | Urine | Nitrofurantoin for 7 days | Qureshi and Patel4 | |
| Bicuspid aortic valve | N negative | Ampicillin plus gentamicin for 3 days | |||||||||
| E 2+ | Penicillin plus gentamicin for 3 weeks | ||||||||||
| Leukocytes 11−22 | Penicillin for 3 weeks | ||||||||||
| 3 | 5 years | Male | Foul-smelling urine | Bladder diverticulum | 50-70 leukocytes/field | Cystitis | Urine | Amoxicillin/clavulanic acid for 10 days | Skalidis et al.5 | ||
| 4 | 12 years | Male | Foul-smelling urine | 187−275 leukocytes | Cystitis | Urine | Corynebacterium, Actinomices neuii, Veillonella, Bacteroides fragilis | Amoxicillin/clavulanic acid for 10 days | Lenherr et al.6 | ||
| 5 | 11 years | Male | Foul-smelling urine | Normal | Cystitis | Urine | Penicillin | Gibb and Sivaraman7 | |||
| 6 | 7 years | Male | Foul-smelling urine | LE and N negative | Cystitis | Urine | Trimethoprim/sulfamethoxazole | De Vries and Brandenburg8 | |||
| 7 | 12 years | Male | Fever (39.5 °C), pain in RF, vomiting and diarrhoea | Bilateral JGO | LE 4+ | Leukocytes 15,300/mm3 | Pyelonephritis | Urine | Ampicillin/sulbactam for 2 days | Murray et al.9 | |
| Grade 4 left VUR | N negative | Erythrocyte sedimentation rate (ESR) 34 mm/h | Cefazolin for 5 days | ||||||||
| Pyeloplasty | E 4+ | Cefalexin for 7 days | |||||||||
| 8 | 14 years | Male | Fever 38.1 °C | Acute myeloid leukaemia | Leukocytes 800/mm3 | Bacteraemia | Blood | Ceftriaxone | Colakoglu et al.10 | ||
| Leukopenia | CRP 96 mg/l | ||||||||||
| 9 | 10 years | Male | Fever 40 °C, pain in RF | Recurrent UTI | LE 2+ | Leukocytes 14,590/mm3 | Pyelonephritis | Urine | Cefixime for 7 days | Our case | |
| N negative | CRP 22.6 mg/l | ||||||||||
| 10 | 5 years | Male | Erythema and urinary meatus discharge | Balanitis | Urethral discharge | Topical mupirocin for 7 days | Our case | ||||
| 11 | 8 years | Male | Abdominal pain, dysuria, diarrhoea | E 2+ | Cystitis | Urine | Fosfomycin tromethamine | Our case |
CRP: C-reactive protein; E: erythrocytes; JGO: juxtaglomerular obstruction; LE: leukocyte esterase; N: nitrites; RF: right flank; VUR: vesicoureteral reflux.
These micro-organisms are difficult to identify by conventional methods since they are easily mistaken for Enterococcus or Streptococcus viridans, Abiotrophia defectiva, Lactococcus, Leuconostoc, or Pediococcus. Furthermore, urine cultures often yield false negatives since these are slow-growing, nutritionally demanding, facultative anaerobic bacteria that usually grow with CO2. Proper identification requires an experienced microbiologist.1,2 At present, MALDI-TOF mass spectrometry is being used to help identify these pathogens.
In conclusion, A. urinae and A. sanguinicola are uncommon, difficult-to-identify micro-organisms that cause genitourinary infections in paediatric patients and are probably underdiagnosed. Studying their epidemiology, signs and association with underlying disease in the paediatric population will enable the relationship to the prognosis to be established and suitable treatments to be selected.
Please cite this article as: Gutiérrez-Fernández J, Gámiz-Gámiz A, Navarro-Marí JM, Santos-Pérez JL. Infección del tracto genitourinario en el niño por Aerococcus no viridans. Revisión bibliográfica y descripción de 3 casos. Enferm Infecc Microbiol Clin. 2021;39:156–158.