The hand-foot-and mouth disease is an acute viral infection characterized by fever and vesicular exanthema affecting predominantly the palms of the hands, the palms of the feet, and the oral mucose.1 The isolated etiological agents most commonly associated with this disease are the coxackievirus A16 and the human enterovirus 71,2,3 although other enteroviruses, mainly class A, and echoviruses, have also been identified.4,5 The mechanism of transmission is fecal-oral through respiratory secretions or else, contact with the exudate of the lesions,6 since the virus replicates in the pharynx and the intestines. This disease predominantly affects kids under five (5) years of age.6
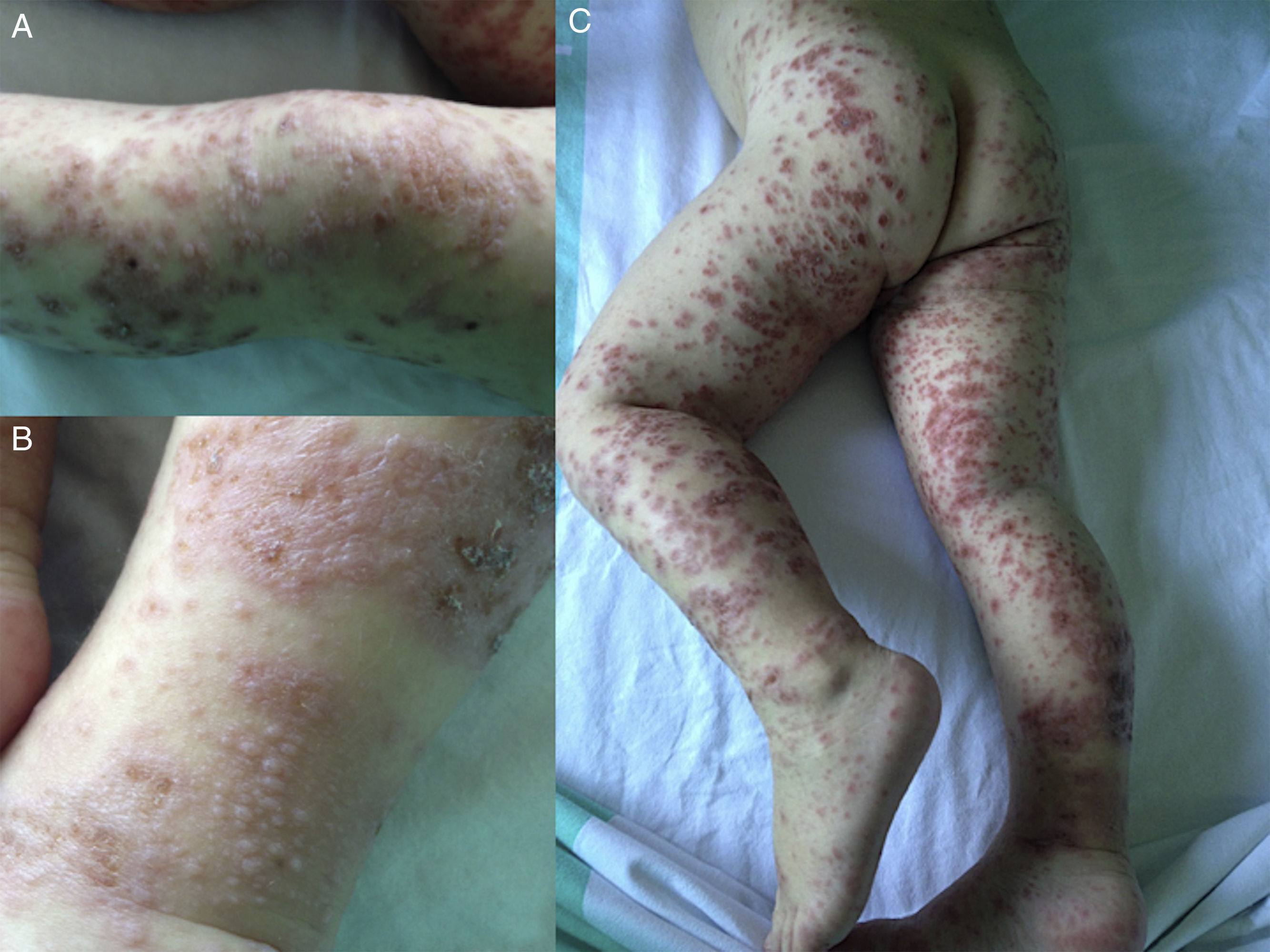
Clinical caseTwo-year-old kid who presented to the ER with an initially perioral pruringinous exanthema of palmoplantar affectation that in a matter of a few hours invaded the gluteal region, the upper and lower limbs with distal predominance, and the auricular pavilion, with some mild affectation at abdominal level. These are vesicular lesions on an erythematous base and, on some occasions, on a purpuric base, being some of them scabs that make up plaques with isolated petechial lesions in the abdominal region. In the perioral zone, we can see lesions in the impetiginized scabies phase. For the last 48h, the patient had a fever with maximum peaks of 101.3°F accompanied by rhinitis and cough. The device-based systematic examination was anodyne except for the aforementioned exanthema. The patient's personal history showed the presence of poorly controlled atopic dermatitis. In an attempt to structure the filiation of the etiology of the patient's clinical manifestations, one blood test was conducted with hemogram, hemostasis, and biochemistry including infection markers and one microbiological study taking samples for blood culture and serological purposes (HBV, HCV, CMV, mycoplasma, EBV, and parvovirus). Also, one vesicular exudate was collected in order to conduct PCR analyses of enteroviruses, and skin smear to rule out bacterial infection and nasopharyngeal aspirate. Both the hemogram, and the studies of biochemistry and hemostasis conducted were anodyne, while the infection markers were discreetly high showing one PCR score of 3.22mg/dl, and one PCT score of 0.33ng/ml. The microbiological study only showed the isolation of the saprophytic flora (Candida parasilopsis) and the PCR analysis tested positive, which is why the sample was sent to the reference lab for its genotyping, that confirmed the presence of coxackievirus A6. Oral hydroxyzine treatment was administered plus IV amoxicillin-clavulanic acid and topical mupirocin on the superinfected lesions. During the hospital admission and subsequent office follow-ups, an adequate progression of the patient's lesions was confirmed with disappearance of these lesions leaving no visible marks and followed by furfuraceous desquamation (Figs. 1–4).
This was a sporadic case managed at our center ER that happens to be part of the most serious and disseminated spectrum of the hand-foot-and mouth disease called “eczema coxsackium” classified from cases with similar characteristics and reported to the Centers for Disease Control and Prevention. From 2008, the coxackievirus A6, which was rare until now as the culprit in this disease, has been tagged as the etiological agent involved in these most severe episodes, initially in Western Asia and Europe and, more recently, in the United States.6
During childhood, the period that has the highest incidence rates is between 12 and 36 months of age – exactly the age of our patient, 24 months old. Clinically, and just as it has been published and reviewed in similar cases so far, the clinical manifestations are different from the classic disease in that there is greater skin damage that may include the back of hands and feet, calves, forearms, trunk, and neck, and a lower percentage of cases with intraoral affectation, as it was the case with our patient.4,7 The lesions usually coalesce making up large blistering lesions that progress into erosions and scabs. The development of perioral papulovesicular affectation has been associated with infections due to coxackievirus A6.6 Same as it happens with the eczema herpeticum, in kids affected by atopic dermatitis like our case, vesicular lesions usually spread in eczematous regions.7
If we take a look at the cases reported so far, the course of this new variant is acute, benign, and similar to the typical clinical manifestations. The systemic symptoms usually disappear in a few days and the skin lesions go away, leaving no visible marks, in a matter of days or weeks.
Please cite this article as: Barbed-Ferrández S, Arrudi-Moreno M, Álvarez-Salafranca M, Bustillo-Alonso M. Preescolar con exantema cutáneo y fiebre. Enferm Infecc Microbiol Clin. 2018;36:137–139.