Thirty-eight-year-old male from Guinea who lived in Brazil for four (4) years and has been living in Spain since the year 2004. He had a prior history of Chagas disease accompanied by mild sensory polyneuropathy that was treated with benznidazole. Back in May 2010 he underwent one orthotopic liver transplant at our center due to hepatitis B virus-related cirrhosis and hepatocarcinoma. The post-transplant period occurred without any complications.
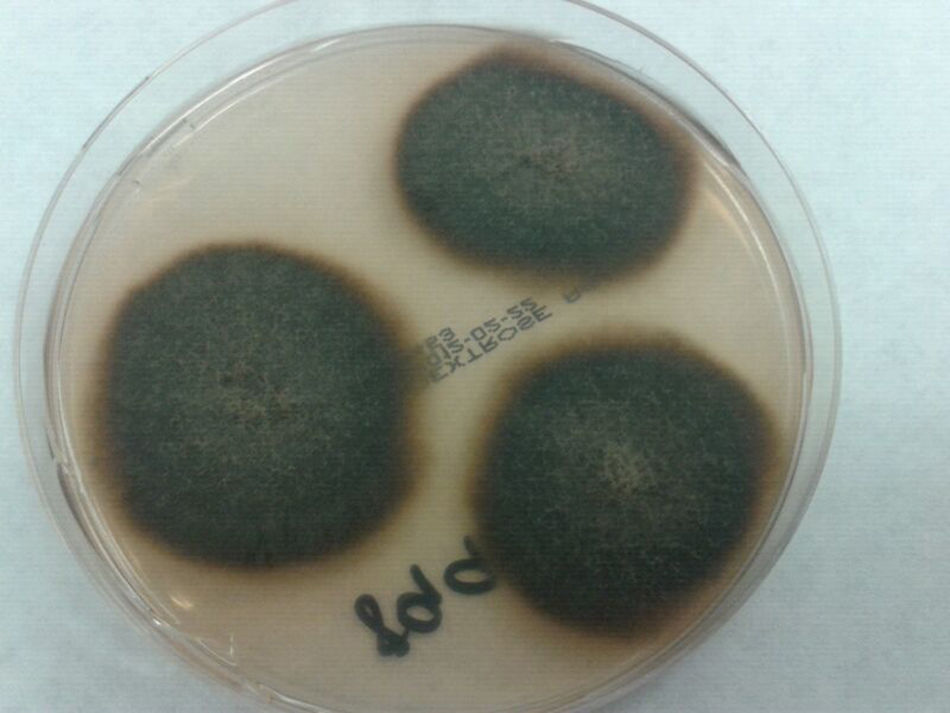
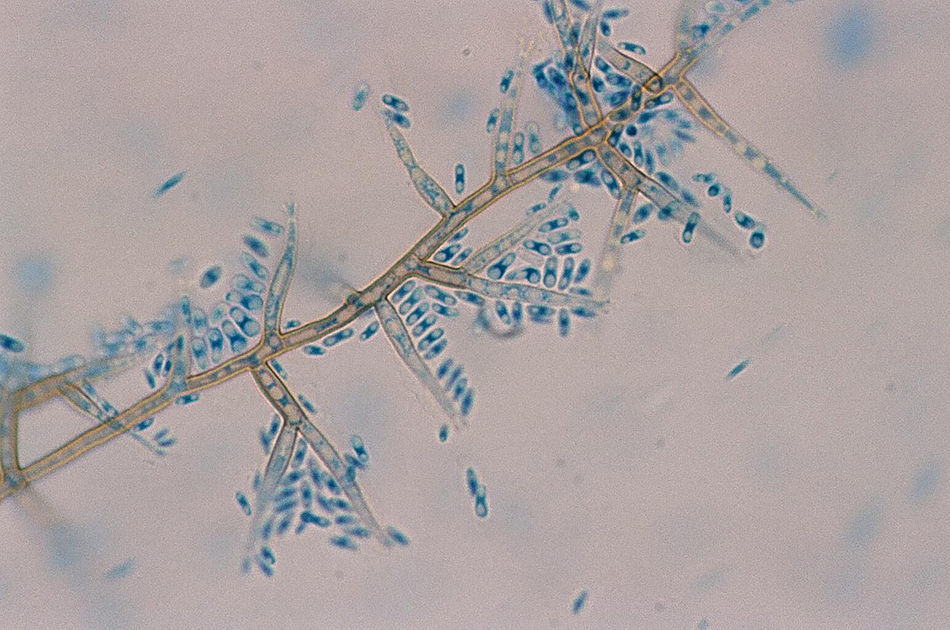
On the +60th day, the patient had an asymptomatic infection due to cytomegalovirus that was treated with valganciclovir for two (2) weeks. Ten (10) days later, the presence of two (2) painless, violet, nonsuppurative skin nodes (one in each thigh) of approximately 2cm×2cm was confirmed. The patient had no recollection of prior trauma. He was on immunosuppressive treatment with tacrolimus and steroids. He had not received any antifungal drugs at that time or previously. The skin biopsy was suggestive of panniculitis with presence of hyphae on the anatomopathological study. Both nodes were removed, and after (5) days of incubation at 86°F the culture on Sabouraud-dextrose agar medium showed dark cotton-like colonies that were black on the back (Fig. 1). The microscopic study showed dark septate hyphae, conidiogenous cells with collarets, and slightly curved cylindrical conidia (Fig. 2).
The nucleotide sequence with ITS-1 and ITS-4 primers revealed a 98 per cent sequence similarity with Phaeoacremonium fuscum using the GenBank BLAST database. Then, the Mycology Unit of the National Microbiology Center of Madrid, Spain confirmed the identification of Phaeoacremonium fuscum with the following sensitivity using the EUCAST methodology1: minimum inhibitory concentration (MIC): amphrotericin B 0.12mg/l; itraconazole >8mg/l; voriconazole 2mg/l, posaconazole >8mg/l; terbinafine 1mg/l; and caspofungin >16mg/l.
The thoracoabdominal CT scan conducted revealed normal findings. The patient has remained asymptomatic ever since and no new lesions have appeared.
Final commentThe Phaeoacremonium species that was described by Crous et al.2 includes over 20 different species of filamentous fungi. It can be found in the environment and it has been isolated in human beings and woody plants such as endophytes or disease causal agents. Few species have proven to be human pathogens only.3 On the morphological level, the Phaeacremonium species is categorized between the Acremonium and the Phialophora species.4 Phaeacremonium spp are opportunistic pathogens that can cause subcutaneous infections; eumycetomas; osteoarthritis; osteomyelitis; or disseminated infection such as fungemia and endocarditis. They are usually preceded by traumatic inoculation. Subcutaneous infections are common in rural workers who are in contact with contaminated soils, thorns, splinters, or other objects causing the trauma.5 Because of the presence of splinters in the lesions, it is believed that retaining the contaminated material is needed to cause the lesion; however, other cases have been reported where no foreign body was ever found. Infections due to these fungi have been reported worldwide, although they are more common in tropical and subtropical climates. They are more prevalent in immunosuppressed patients, but they can also be seen in individuals without any predisposing factors.6
The identification of the species is based on its morphological and culture characteristics, though, at times, this identification is not easy. The management of most patients with localized infections is deep surgical resection and it is usually enough.7,8 In some cases, antifungal therapy has been administered too. Phaeacremonium fuscum is one of those species that can cause cutaneous and subcutaneous affectation in humans. Its maximum growth occurs at temperatures of 98.6°F compared to the 86°F of other species. Its capacity of growth at 98.6°F suggests it can survive at body temperature.9 Mc Grogan et al. described the first case of mycetoma due to Phaeoacremonium fuscum in a kidney transplant recipient.10
In sum, Phaeoacremonium fuscum is a rare cause of cutaneous or subcutaneous fungal infection mainly affecting immunosuppressed patients, being the complete resection of the lesion with curative purposes important in cases in which the infection is localized as it was the case with our patient. As we mentioned above, these cases are usually preceded by traumatic inoculation and even though in our case, the patient had no recollection of any prior traumas, we cannot rule it out, or the fact that the patient experienced local reactivation in the context of his immunosuppressive therapy.
Please cite this article as: Blanco-Vidal MJ, López-Soria L, Monzón-de la Torre A, Montejo-Baranda JM. Nódulos cutáneos en trasplantado hepático. Enferm Infecc Microbiol Clin. 2018;36:140–141.