The high pharmacotherapeutic complexity, drug interactions and lack of adherence to concomitant medication are circumstances with negative consequences in the clinical evolution of patients with HIV infection. The 3-HIT phenomenon refers to the simultaneous occurrence of these situations. The objective of the study is to determine the prevalence of the phenomenon 3-HIT in the polymedicated HIV population as well as to determine factors related to its occurrence.
MethodsObservational, retrospective and single-center study that included all elderly patients on active antiretroviral treatment in pharmacotherapeutic follow-up between January and March 2020. A logistic regression model was carried out to evaluate the factors associated with the occurrence of the 3-HIT concept with the variables significantly associated with this phenomenon and those considered clinically relevant.
Results428 patients were included, registering a prevalence of polypharmacy in 25.9% of the study sample. The 3-HIT phenomenon was detected in 6.3% of the patients. For each concomitant drug prescribed the risk of developing the phenomenon 3-HIT increases 1.5 times.
ConclusionPrevalence of the phenomenon 3-HIT is high in HIV patients with polymedication. A change in the pharmaceutical care model to a multidimensional setting is essential, together with pharmacotherapeutic optimization strategies to improve patient health outcomes.
La alta complejidad farmacoterapéutica, las interacciones farmacológicas y la falta de adherencia a la medicación concomitante son circunstancias con consecuencias negativas en la evolución clínica de los pacientes con infección por VIH. El fenómeno 3-HIT se refiere a la ocurrencia simultánea de estas situaciones. El objetivo del estudio es determinar la prevalencia del fenómeno 3-HIT en la población VIH polimedicada así como determinar los factores relacionados con su ocurrencia.
MétodosEstudio observacional, retrospectivo y unicéntrico que incluyó a todos los pacientes ancianos en tratamiento antirretroviral activo en seguimiento farmacoterapéutico entre enero y marzo de 2020. Se realizó un modelo de regresión logística para evaluar los factores asociados a la ocurrencia del 3-HIT concepto con las variables significativamente asociadas a este fenómeno y aquellas consideradas clínicamente relevantes.
ResultadosSe incluyeron 428 pacientes, registrándose una prevalencia de polifarmacia en el 25,9% de la muestra de estudio. El fenómeno 3-HIT se detectó en el 6,3% de los pacientes. Por cada fármaco concomitante prescrito, el riesgo de desarrollar el fenómeno 3-HIT aumenta 1,5 veces.
ConclusiónLa prevalencia del fenómeno 3-HIT es alta en pacientes VIH con polimedicación. Un cambio en el modelo de atención farmacéutica a un entorno multidimensional es esencial, junto con estrategias de optimización farmacoterapéutica para mejorar los resultados de salud de los pacientes.
The prevalence of elderly people living with HIV infection (PLHIV) is growing at an exponential rate thanks to the development and improvement of antiretroviral therapy (ART), which has made it possible to transform the infection into a chronic pathology1. In fact, it is expected that by 2030, 73% of PLHIV will be 50 years of age or older and almost 40% will be over 65 years of age2,3. In addition, this population may be more vulnerable to the development of events associated with ageing4. This has resulted in a higher prevalence of chronic pathologies and comorbidities at younger ages than in the general population, with the consequent prescription of drugs to control them5,6.
Polypharmacy, defined as the simultaneous administration of six or more medications, is growing in PLHIV, it being estimated that 15%–39% of these patients are polymedicated, a percentage that rises to 82% in patients older than 50 years7. The presence of polypharmacy is a condition associated with a series of growing problems such as the prescription of potentially inappropriate medication (PIM), drug interactions, medication-related adverse events, non-adherence to concomitant medication and the appearance of high pharmacotherapeutic complexity8,9. The study by Morillo-Verdugo et al. determined a prevalence of 32.4% of polypharmacy in PLHIV, which rises to 71.6% in over-65s. They also reported the development of cardiometabolic and anxiety-depression comorbidities at earlier ages, according to the most common polypharmacy patterns in Spain10. In this same study, the risk factors for polypharmacy, such as ART, the presence of potential interactions, the use of different types of drugs and the number of comorbidities, were determined5.
Traditionally, a quantitative approach has been taken to measuring polypharmacy, i.e. based on the number of medications prescribed. However, in recent years a more qualitative approach has been embraced, since the same number of drugs may differ, among other aspects, in the instructions for use, preparation or administration, pharmaceutical form or dosage regimen. George et al.11 published the so-called “medication regimen complexity index” (MRCI), which allows all these aspects to be grouped together and weighted. In this regard, a value of 11.25 on this index has been established as a threshold for classifying a polymedicated patient as highly complex in PLHIV12.
The consequences of non-adherence to ART, such as the development of mutations that lead to virological failure and loss of viral undetectability, are known. On the other hand, non-adherence to concomitant medication has been related to the decompensation of chronic cardiometabolic pathologies and even to the risk of readmission13.
As mentioned above, the phenomena of polypharmacy, potentially inappropriate medication and drug interactions have been the subject of different studies, albeit always separately. However, for these phenomena to be more representative of reality, the medication adherence component must be included. For this reason, we have defined the 3-HIT concept, referring to a combined variable that includes the three elements that we regard as key to the management of polypharmacy in PLHIV, namely high pharmacotherapeutic complexity, the presence of drug interactions and non-adherence to concomitant medication.
The main objective of our study is therefore to assess the prevalence of this phenomenon and to study the possible risk factors associated with its development in PLHIV with polypharmacy.
MethodsDesignAn observational, retrospective, single-centre study was carried out, which included all PLHIV over 18 years of age on active ART and treated at hospital pharmacy outpatient departments between 1 January and 31 March 2021 using the Pharmaceutical Care Capability, Opportunity, Motivation (COM) methodology14. Patients participating in clinical trials and those who did not sign the informed consent were excluded.
Sociodemographic and clinical variables were collected, as were immunological, virological, ART and concomitant medication data. A complete list of non-HIV-related comorbidities was obtained by a retrospective clinical history review, while the drugs were taken from the clinical histories of the patients treated at our pharmacy outpatient departments. To describe the multimorbidity patterns, the classification proposed by De Francesco et al.15 was used, and which includes: cardiovascular disease, chronic obstructive pulmonary disease (COPD)-liver disease, HIV/AIDS-related events, neurological-psychiatric diseases, sexually transmitted diseases and general health.
Polypharmacy was defined as the concomitant administration of six or more different drugs, including ART. The term major polypharmacy was restricted to the simultaneous use of 11 different active ingredients. To describe polypharmacy patterns, we used the classification proposed by Prados-Torres et al.16: cardiovascular, anxiety-depression, COPD and mixed. The classification of a patient within the patterns of polypharmacy required at least three drugs included in this group.
The harmacotherapyeutic complexity index was measured using the MRCI tool, a validated 65-item tool that assesses the complexity of the treatment regimen based on the number of medications, dosage form, dosage frequency and additional or special instructions17.
The University of Liverpool database was used to identify drug–drug interactions (DDIs) between the ART and concomitant medication. The Lexicomp© tool was used to identify the DDIs between different non-antiretroviral drugs, taking into account those rated as D (potential) or X (contraindications). To assess non-adherence to concomitant medication, we used the multiple-interval dispensing coefficient in the prescription of medication collected at the pharmacy by means of the Receta XXI-Diraya (concomitant medication) and at hospital pharmacy (ART) outpatient departments by means of the Dominion-Farmatools© outpatient dispensing programme for the last six months. Non-adherence to concomitant medication was considered to be the collection of less than 90% of the prescribed medication by the scheduled date.
The main variable was the prevalence of the 3-HIT phenomenon, defined as the simultaneous presence of high pharmacotherapeutic complexity, DDIs and non-adherence to concomitant medication.
The study complied with all the ethical requirements and was approved by the Clinical Research Ethics Committee of the Hospital Virgen de Valme (C.I. 0987-N-21).
Statistical analysisThe discrete variables were expressed as frequency (percentage) and continuous variables as medians and interquartile ranges (IQR). The hypothesis of independence was studied using the Chi-square test or Fisher’s exact test in the case of categorical variables and the Mann–Whitney T or U test for qualitative variables, depending on whether or not they fit normality.
A logistic regression model was carried out to evaluate the factors independently related to the occurrence of the 3-HIT phenomenon. The variables significantly associated with this phenomenon, those that address relevant pharmacotherapeutic or clinical aspects for the follow-up of PLHIV, were considered in the bivariate analysis. The threshold for statistical significant was set at p<0.05. The data analysis was performed with the Windows SPSS statistical package, version 25.0.0.
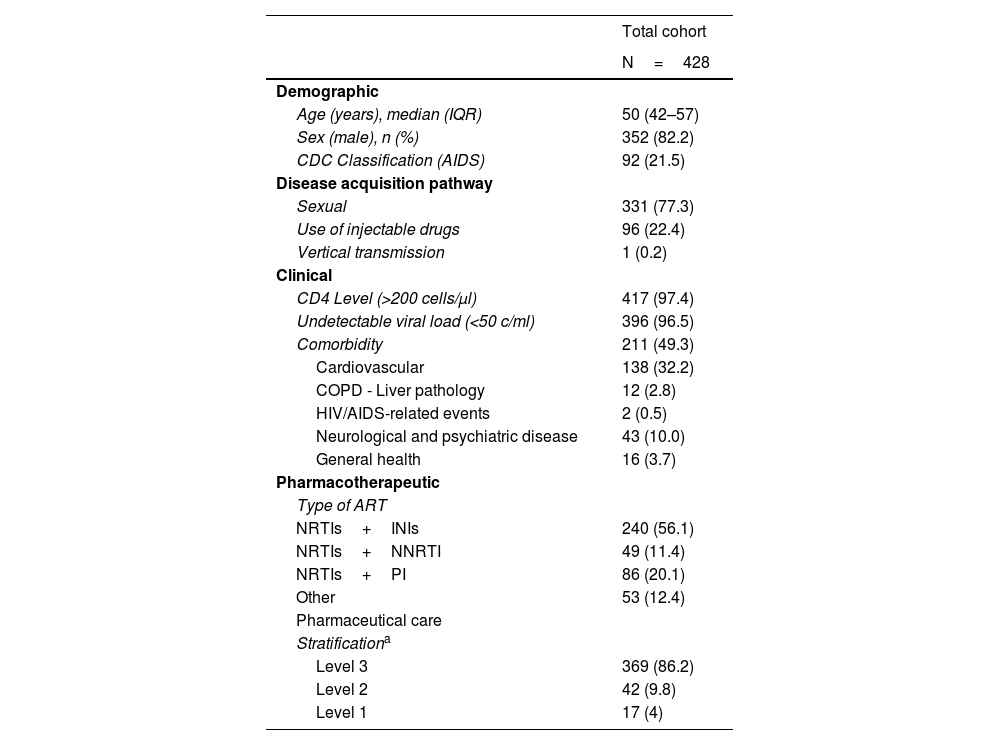
ResultsA total of 428 patients with HIV infection were included. 82.2% were men and 58.4% were older than 50 years. 96.5% had an undetectable viral load and 97.6% CD4 T lymphocyte levels >200 cells/μl. The first ART in the PLHIV included in the study had started with a mean of 12.2 (±3.2) years, while the current regimen evaluated in the study had a mean period of 3.9 (±1.7) years. The main baseline characteristics of the study population are shown in Table 1.
Baseline characteristics of the patients included in the analysis.
| Total cohort | |
|---|---|
| N=428 | |
| Demographic | |
| Age (years), median (IQR) | 50 (42–57) |
| Sex (male), n (%) | 352 (82.2) |
| CDC Classification (AIDS) | 92 (21.5) |
| Disease acquisition pathway | |
| Sexual | 331 (77.3) |
| Use of injectable drugs | 96 (22.4) |
| Vertical transmission | 1 (0.2) |
| Clinical | |
| CD4 Level (>200 cells/μl) | 417 (97.4) |
| Undetectable viral load (<50 c/ml) | 396 (96.5) |
| Comorbidity | 211 (49.3) |
| Cardiovascular | 138 (32.2) |
| COPD - Liver pathology | 12 (2.8) |
| HIV/AIDS-related events | 2 (0.5) |
| Neurological and psychiatric disease | 43 (10.0) |
| General health | 16 (3.7) |
| Pharmacotherapeutic | |
| Type of ART | |
| NRTIs+INIs | 240 (56.1) |
| NRTIs+NNRTI | 49 (11.4) |
| NRTIs+PI | 86 (20.1) |
| Other | 53 (12.4) |
| Pharmaceutical care | |
| Stratificationa | |
| Level 3 | 369 (86.2) |
| Level 2 | 42 (9.8) |
| Level 1 | 17 (4) |
ART: antiretroviral therapy; INIs: integrase inhibitors; MRCI: Medication Regimen Complexity Index; NRTIs: nucleoside reverse transcriptase inhibitors; NNRTI: non-nucleoside reverse transcriptase inhibitors; PI: protease inhibitors.
Stratification according to the Pharmaceutical Care model for HIV patients from the Sociedad Española de Farmacia Hospitalaria [Spanish Society of Hospital Pharmacy]18.
Of the study cohort, 111 patients (25.9%) fulfilled the definition of polypharmacy and 23 patients (5.4%) that of major polypharmacy. Of the 220 patients who presented multimorbidity, the most common comorbidity patterns were cardiometabolic (34.6%) and anxiety-depression (10.3%). The mean number of concomitant drugs was four (±3) and 303 patients (70.8%) received two or more drugs concomitantly with ART.
Focusing on the elements that comprise the 3-HIT phenomenon, the mean value of the total complexity index was 6.9 (±5.5). More than half (69.4%) of PLHIV regarded themselves as adherent to both the ART and the concomitant medication. Drug interactions were present in 120 patients, the most frequent being potential interactions between the ART and concomitant medication (23.6%). The presence of absolutely contraindicated interactions was found in five patients (1.2%).
The interrelationship analysis between the criteria suggestive of the 3-HIT concept in PLHIV showed that 27 (6.3%) of the patients presented the three criteria included in this concept.
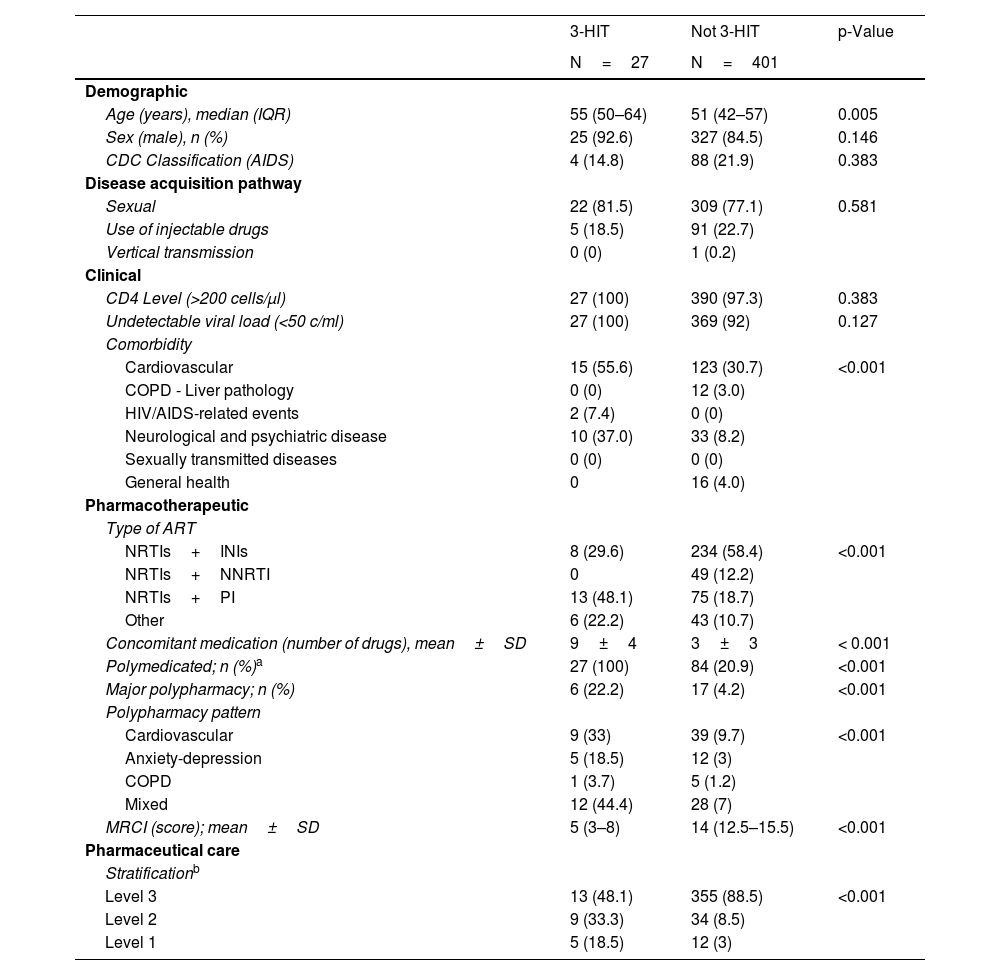
In the bivariate analysis, significant differences were observed between patients with and without 3-HIT in variables such as age, comorbidity pattern, type of ART, polypharmacy, polypharmacy pattern, complexity index and stratification level. Table 2 shows the complete results.
Bivariate analysis between patients for whom 3-HIT was recorded and those for whom it was not.
| 3-HIT | Not 3-HIT | p-Value | |
|---|---|---|---|
| N=27 | N=401 | ||
| Demographic | |||
| Age (years), median (IQR) | 55 (50–64) | 51 (42–57) | 0.005 |
| Sex (male), n (%) | 25 (92.6) | 327 (84.5) | 0.146 |
| CDC Classification (AIDS) | 4 (14.8) | 88 (21.9) | 0.383 |
| Disease acquisition pathway | |||
| Sexual | 22 (81.5) | 309 (77.1) | 0.581 |
| Use of injectable drugs | 5 (18.5) | 91 (22.7) | |
| Vertical transmission | 0 (0) | 1 (0.2) | |
| Clinical | |||
| CD4 Level (>200 cells/μl) | 27 (100) | 390 (97.3) | 0.383 |
| Undetectable viral load (<50 c/ml) | 27 (100) | 369 (92) | 0.127 |
| Comorbidity | |||
| Cardiovascular | 15 (55.6) | 123 (30.7) | <0.001 |
| COPD - Liver pathology | 0 (0) | 12 (3.0) | |
| HIV/AIDS-related events | 2 (7.4) | 0 (0) | |
| Neurological and psychiatric disease | 10 (37.0) | 33 (8.2) | |
| Sexually transmitted diseases | 0 (0) | 0 (0) | |
| General health | 0 | 16 (4.0) | |
| Pharmacotherapeutic | |||
| Type of ART | |||
| NRTIs+INIs | 8 (29.6) | 234 (58.4) | <0.001 |
| NRTIs+NNRTI | 0 | 49 (12.2) | |
| NRTIs+PI | 13 (48.1) | 75 (18.7) | |
| Other | 6 (22.2) | 43 (10.7) | |
| Concomitant medication (number of drugs), mean±SD | 9±4 | 3±3 | < 0.001 |
| Polymedicated; n (%)a | 27 (100) | 84 (20.9) | <0.001 |
| Major polypharmacy; n (%) | 6 (22.2) | 17 (4.2) | <0.001 |
| Polypharmacy pattern | |||
| Cardiovascular | 9 (33) | 39 (9.7) | <0.001 |
| Anxiety-depression | 5 (18.5) | 12 (3) | |
| COPD | 1 (3.7) | 5 (1.2) | |
| Mixed | 12 (44.4) | 28 (7) | |
| MRCI (score); mean±SD | 5 (3–8) | 14 (12.5–15.5) | <0.001 |
| Pharmaceutical care | |||
| Stratificationb | |||
| Level 3 | 13 (48.1) | 355 (88.5) | <0.001 |
| Level 2 | 9 (33.3) | 34 (8.5) | |
| Level 1 | 5 (18.5) | 12 (3) | |
ART: antiretroviral therapy; INIs: integrase inhibitors; MRCI: Medication Regimen Complexity Index; NRTIs: nucleoside reverse transcriptase inhibitors; NNRTI: non-nucleoside reverse transcriptase inhibitors; PI: protease inhibitors.
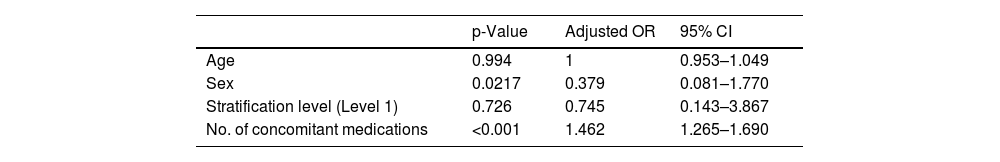
Using a binary logistic regression model, possible factors independently related to the presence of 3-HIT were studied, it transpiring that this included the number of drugs prescribed (OR 1.5; 95% CI=1.3–1.7) (Table 3).
DiscussionOur study shows that the simultaneous appearance of high pharmacotherapeutic complexity, drug interactions and non-adherence to concomitant medication, called the 3-HIT phenomenon, is common in elderly PLHIV. In addition, according to our results, for each new drug prescribed in the patient’s pharmacotherapeutic strategy, the risk of developing the 3-HIT phenomenon increases 1.5-fold.
The simultaneous presence of polypharmacy, drug interactions and potentially inappropriate medication has led to this situation to be defined as the “iatrogenic triad” in recent years19. Previously, the factors involved were analysed by authors such as Greene et al.20. A previous study in elderly PLHIV evaluated the factors involved in this concept separately. The results showed a high prevalence of polypharmacy, a 52% presence of potentially inappropriate medication and 70% drug interactions, 11% of which were interactions that should have been avoided21.
As far as we know, this is the first study that simultaneously takes into account three factors with a significant impact on polymedicated PLHIV, which suggests a change in the healthcare approach. In addition, the relationship between polypharmacy and the appearance of drug interactions is known, and 51% of HIV patients over 50 years of age present interactions between ART and concomitant medication22. The POPPY multicentre study23 showed that drug interactions in polypharmacy patients occur with a higher prevalence in patients over 50 years of age, as was the case in our study, where 36.8% of patients over 50 years of age present polypharmacy compared to 10.7% of patients under that age. In this sense, the importance of interactions in these elderly patients has already been studied by Tseng et al.8, who found a higher frequency of drug interactions in patients treated with protease inhibitors. This data coincides with the data obtained in our study, in which patients treated with protease inhibitors present a higher percentage of interactions, reaching 39.2% of cases.
Adherence to both ART and concomitant medication in patients with HIV infection is a focal point of attention for all professionals involved in caring for these patients. The main consequence of inadequate adherence is therapeutic failure and failure to achieve the established objectives, related to both HIV infection and to underlying diseases24. Focusing on the HIV patient, adherence to medication is fundamental to the suppression of viral load, which allows the disease to be controlled, thus avoiding transmission and delaying the associated maturation25. Given the importance of adherence, the latter has been the subject of different studies that have permitted the development of predictive models of short-term non-adherence26.
The study by Guaraldi et al.27 demonstrated an increased risk of hospital admission of 47% in HIV patients above 65 years with polypharmacy, showing that the risk increases by 8% for each drug prescribed. The relevance of this data is evident given the high prevalence of polypharmacy in this population, 25.9%, and the possible risk involved.
Elderly HIV patients are known to have a high prevalence of prescription problems, where adverse health outcomes associated with polypharmacy and inappropriate prescriptions, causing drug interactions or non-adherence due to not finding any benefit, render it necessary to develop interventions for the prevention of possible harm to the patient, including a review of the prescribed pharmacotherapeutic strategy for the purpose of optimisation26. The level of stratification used in the care of PLHIV has been shown to be a good indicator of negative consequences for the patient's pharmacotherapy and therefore for the development of the 3-HIT phenomenon. The data in the literature on the influence of gender on polypharmacy are contradictory. Although evidence on the relevance of menopause in the increase of polypharmacy does exist. It would be desirable for this relationship to be analysed in future studies to ascertain the extent to which gender can affect the characterisation of polypharmacy28.
This all provides a rationale for the conduct of larger and multicentre studies to explain the risk factors for the appearance of 3-HIT better. Another aspect that should be considered is that, given the novelty of the concept, we do not know whether the percentage of patients in whom 3-HIT appears is higher in non-PLHIV. In addition, studies are called for to evaluate the impact of the multidimensional approach to reduce the percentage of PLHIV in this situation.
The main limitations of the study are its retrospective design, although since its primary objective is not the evaluation of the clinical impact of the prescription of inappropriate medications, the bias caused may be mitigated to a certain extent. In general, the reason for non-adherence was not specified, although it could possibly be related to the patient's refusal or inability to take the medication, lack of response to a medication or adverse effects, rather than the non-prescription of a drug (primary non-adherence was not included in this study). In addition, the number of over-the-counter medications may not be reported and not be included in the Medication Regimen Complexity Index. Finally, in view of the healthcare setting, we did not include an uninfected control group.
Future lines of research that include larger numbers of patients would also allows us to relate the onset of these problems to patient health outcomes. This may be beneficial for the consideration of the practical utility of these criteria in healthcare practice.
In conclusion, the appearance of this new concept associated with negative medication-related consequences provides greater knowledge and the ability to approach pharmacotherapy more realistically and the achievement of objectives in this type of patient. Medication reconciliation and a regular review of prescriptions by experienced pharmacists, ideally as part of multidisciplinary consultations, could reduce the risk of the 3-HIT phenomenon and its deleterious health consequences in these patients. Therefore, the routine introduction of a multidimensional approach in a multidimensional environment for the optimisation of pharmacotherapy in these patients is essential. To confirm the findings of this study, new studies with a larger casuistry are necessary, of a prospective nature and with an uninfected comparator group.
Conflicts of interestThe authors declare that they have no conflicts of interest.