This was a 28-year-old male with no hospital medical history or use of antibiotics in the last six months who came to the Accident and Emergency Department (A&E) with a three-day history of fever, chills, asthenia, reduced appetite and myalgia. He was treated with diclofenac im, injected into his left gluteal muscle. During the following days, his symptoms persisted, associated with oedema, erythema, heat and redness at the application site. Concomitantly, he developed periocular oedema and erythema, eye pain and decreased visual acuity, for which he returned to A&E.
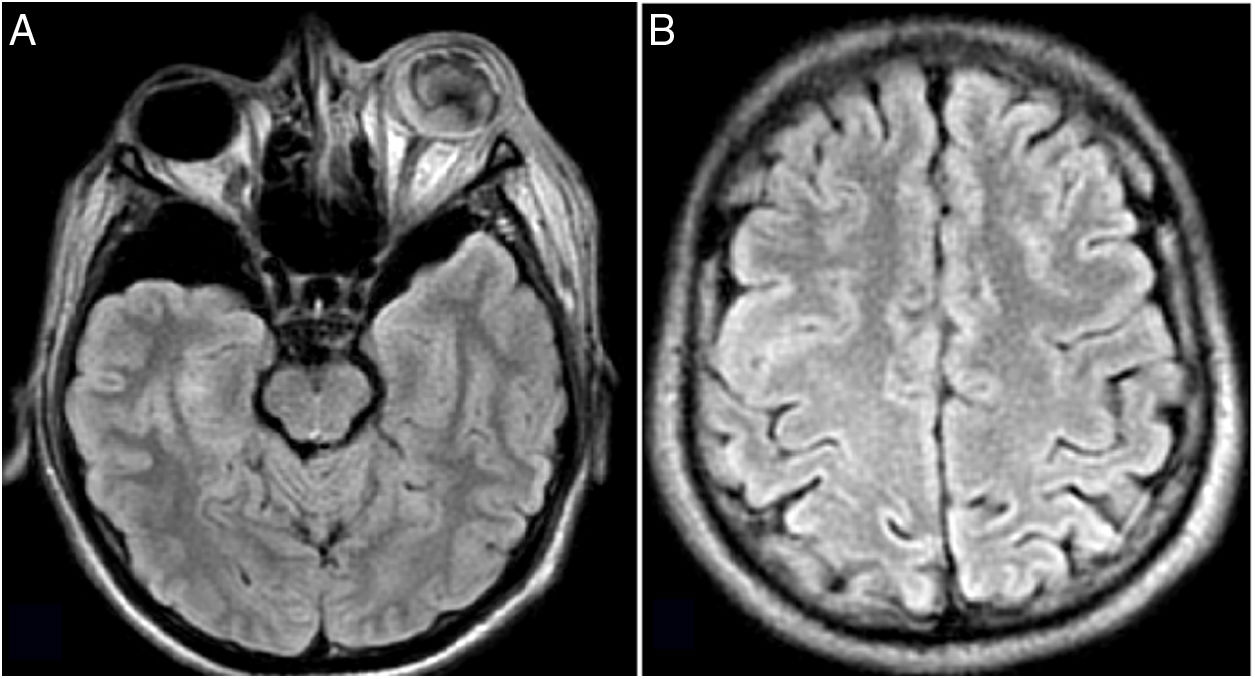
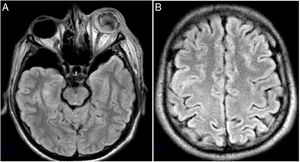
On arrival he was feverish and tachycardic, with local inflammatory signs in his left gluteal region. Ophthalmology examination revealed palpebral oedema, eyelid erythema, ophthalmoplegia, proptosis, 360° chemosis, purulent discharge in the cul-de-sac, 2-mm, hyporeactive pupil, with pain triggered by eye movements. It was not possible to see the fundus of the eye (Fig. 1). Contrast magnetic resonance imaging of the skull with emphasis on orbits revealed rupture of the eyeball towards the superior aspect, purulent material in the anterior and posterior chambers, myositis of the extrinsic muscles of the eye, and preseptal and palpebral inflammation (Fig. 2A). Contrast tomography of the abdomen showed hepatomegaly, multiple bilateral cystic images predominantly in the right interpolar region 42mm in size, compatible with liver abscess in the right lobe (Fig. 3A). Chest tomography revealed lung nodules in the right upper, middle and lower lobes, some of them cavitary (Fig. 3B).
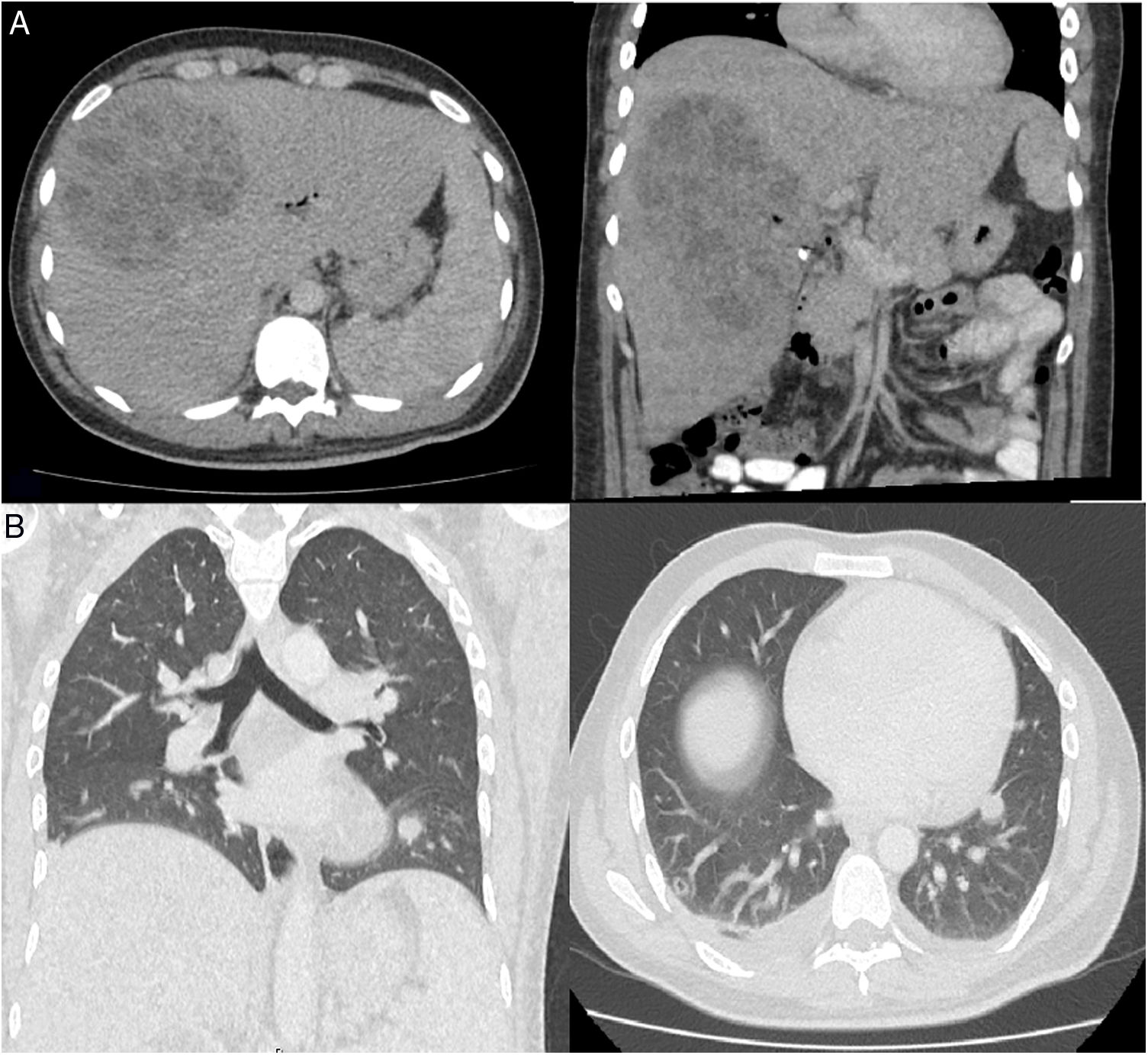
A) FLAIR images showing purulent material in the anterior and posterior chambers accompanied by supraorbital laminar collection oedema, intra- and extraconal soft tissue oedema, and myositis of the extrinsic muscles of the eye. B) Rounded hyperintense lesions in FLAIR, with peripheral ring enhancement and central diffusion restriction of less than a centimetre, with a tendency to confluence in the left medial frontal gyrus, compatible with small abscesses.
The patient was started on antibiotics with ceftriaxone 2g iv/12h and vancomycin 1g iv/12h. Blood cultures were positive for Klebsiella pneumoniae with the usual sensitivity pattern. Antibiotic therapy was continued with ceftriaxone alone. In the light of these findings, enucleation of the left eyeball was performed without complications. An extension study of the supratentorial brain parenchyma showed multiple hyperintense lesions in T2 and FLAIR, with peripheral ring enhancement and central diffusion restriction, less than a centimetre, compatible with small abscesses of probable embolic origin (Fig. 2B). Repeat blood cultures taken 48h after antibiotic therapy were negative. Transoesophageal echocardiogram showed no signs of vegetations. A collection of 154 cm3 was documented in soft tissues in the patient's left gluteal region, with disruption of the superficial fascia, myositis in the musculature of the gluteal compartment and oedema of the deep fascia. He was taken to theatre for surgical lavage on two separate occasions, with Gram staining and cultures of secretions negative. The final diagnosis was multiple abscesses due to hypervirulent K. pneumoniae.
CommentsKlebsiella pneumoniae is a member of the Enterobacteriaceae family of bacteria. It is highly important from a clinical point of view and is responsible for both hospital- and community-acquired infections. Most infections caused by this pathogen are associated with pneumonia or urinary tract or intra-abdominal infections. However, in the mid-1980s, a different clinical syndrome emerged, associated with hypervirulent subtypes of the bacteria and characterised by bacteraemia, liver abscesses and serious disseminated infections. Although initially described in Southeast Asia, since its recognition, cases have been reported worldwide.1,2 In the case we present here, the patient denies travel to Southeast Asia or frequenting restaurants associated with that region.
Capsular serotypes K1 and K2 are considered the most virulent strains of K. pneumoniae, with K1 the strain most commonly found in patients with invasive liver abscess syndrome. The hypermucosity phenotype has been cited as an important virulence factor of this pathogen.3,4 This is characterised by increased production of capsular polysaccharides, which aids bacterial evasion of phagocytosis by macrophages and mononuclear cells. At the molecular level, specific virulence genes have been described, such as rmpA (responsible for regulating the mucoid phenotype) and magA (responsible for the capsular serotype K1), both of which are determining factors of hypervirulence.5,6
Diabetes mellitus has been identified as the most common risk factor.7,8 The infection can compromise a number of different organs and can cause meningitis or brain abscesses, endogenous endophthalmitis, lung, prostate and soft tissue abscesses, necrotising fasciitis and osteomyelitis, as in the case presented here.7–9 Early percutaneous drainage of the liver abscess and targeted antibiotic treatment are the most important predictors in relation to decreasing mortality risk and a lower risk of complications.10
Please cite this article as: Díaz-Brochero C, Gerena LG, Cortés JA. Síndrome de abscesos múltiples invasivos en paciente inmunocompetente. Enferm Infecc Microbiol Clin. 2020;38:500–502.