Respiratory syncytial virus (RSV) causes an acute respiratory illness similar to influenza, although there are few data comparing both of them in adults. The existence of clinical differences between these two infections could have implications for their management.
Materials and methodsRetrospective observational cohort study including 63 adults with positive PCR for RSV and 221 for influenza during winter 2018–2019. Epidemiological, clinical characteristics and outcomes were contrasted between both groups.
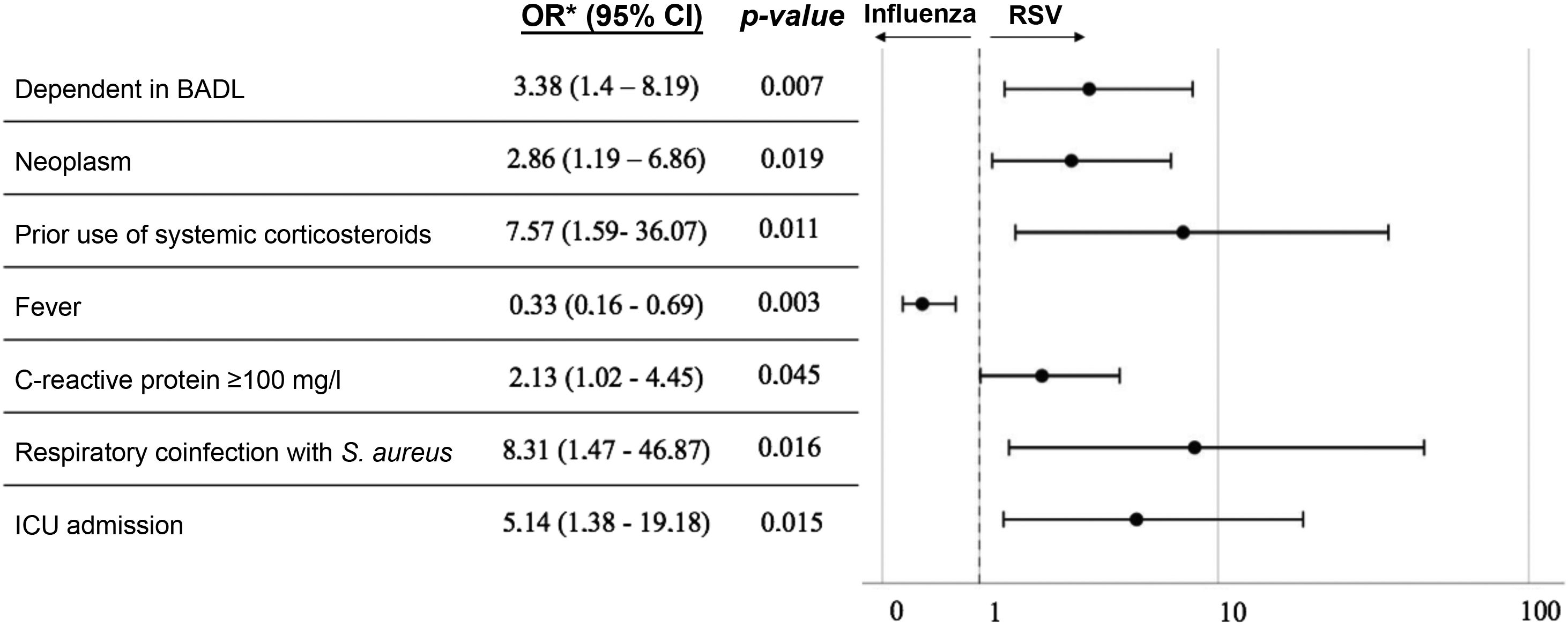
ResultsCompared to influenza, RSV-positive patients presented a higher association with active neoplasia (OR=2.9; 95% CI: 1.2–6.9), dependence for basic activities of daily living (OR=3.4; 95% CI: 1.4–8.2) and immunosuppression due to chronic glucocorticoid administration (OR=7.6; 95% CI: 1.6–36.1). At diagnosis, fever was less common (OR=0.3; 95% CI: 0.2–0.7), and C-reactive protein level ≥100mg/l was more frequent (OR=2.1; 95% CI: 1.0–4.5). They developed bacterial co-infection by Staphylococcus aureus in a higher proportion (OR=8.3; 95% CI: 1.5–46.9) and presented a greater need for admission to the intensive care unit (OR=5.4; 95% CI: 1.4–19.2).
ConclusionRSV is an important cause of respiratory illness in adults during the influenza season. It especially affects vulnerable patients with chronic underlying diseases, and has a higher morbidity than influenza. For all these reasons, specific detection, prevention and treatment of RSV is necessary in order to reduce the consumption of health care resources due to RSV disease in adults.
El virus respiratorio sincitial (VRS) produce una enfermedad respiratoria aguda parecida a la gripe, aunque en adultos existen pocos datos que las comparen. La existencia de diferencias clínicas entre ambas infecciones podría conllevar implicaciones en su manejo.
Materiales y métodosEstudio observacional de cohortes retrospectivo incluyendo 63 adultos con PCR positiva para VRS y 221 para gripe durante el invierno 2018–2019. Se contrastaron las características epidemiológicas, clínicas y desenlaces entre ambos grupos.
ResultadosEn comparación con la gripe los pacientes VRS positivos asociaron mayor relación con neoplasia activa (OR=2,9; IC 95%: 1,2–6,9), dependencia para las actividades básicas de la vida diaria (OR=3,4; IC 95%: 1,4–8,2) e inmunosupresión por administración crónica de glucocorticoides (OR=7,6; IC 95%: 1,6–36,1). Al diagnóstico era menos común la presencia de fiebre (OR=0,3; IC 95%: 0,2–0,7) y más frecuente un nivel de proteína C reactiva ≥ 100mg/l (OR=2,1; IC 95%: 1,0–4,5). Desarrollaron coinfección bacteriana por Staphylococcus aureus en mayor proporción (OR=8,3; IC 95%: 1,5–46,9) y presentaron una mayor necesidad de ingreso en la unidad de cuidados intensivos (OR=5,4; IC 95%: 1,4–19,2).
ConclusiónEl VRS es una causa importante de enfermedad respiratoria en adultos durante la época de gripe. Afecta especialmente a pacientes vulnerables con enfermedades crónicas de base, y presenta una morbilidad superior a la gripe. Por todo ello es necesaria la detección, prevención y tratamiento específicos del VRS con el objetivo de reducir el consumo de recursos sanitarios que supone la enfermedad por VRS en adultos.
Respiratory syncytial virus (RSV) is known for causing severe respiratory disease in children and immunocompromised patients. The RSV genome is made up of a negative-sense, single-stranded RNA and the virus belongs to the Pneumoviridae family, genus Orthopneumovirus1. It tends to circulate in winter and, globally, is the most common cause of lower respiratory tract infection in childhood, as well as a major cause of hospital admission in this age group2. Its pathogenic potential in adults, however, is less well understood.
Until a few years ago, a large proportion of adult hospital admissions for RSV during the winter were wrongly attributed to the influenza virus. That situation may largely be explained by the difficulty in making the clinical distinction between the two viral conditions3,4, the low degree of suspicion among physicians, and the lack of accessible techniques for RSV detection. However, the recent and progressive incorporation of molecular techniques into the range of available diagnostic tests has made it possible to significantly increase the number of RSV cases diagnosed during the annual influenza epidemics5. The need therefore arises to determine the true role of RSV as an aetiology to be ruled out in cases of severe lower respiratory tract infection at this time of year.
The aim of this study was to analyse and compare the clinical and epidemiological characteristics and the outcomes among patients infected with RSV and influenza over the 2018–2019 winter season at Hospital Universitario Fundación Alcorcón (HUFA) in Madrid, Spain.
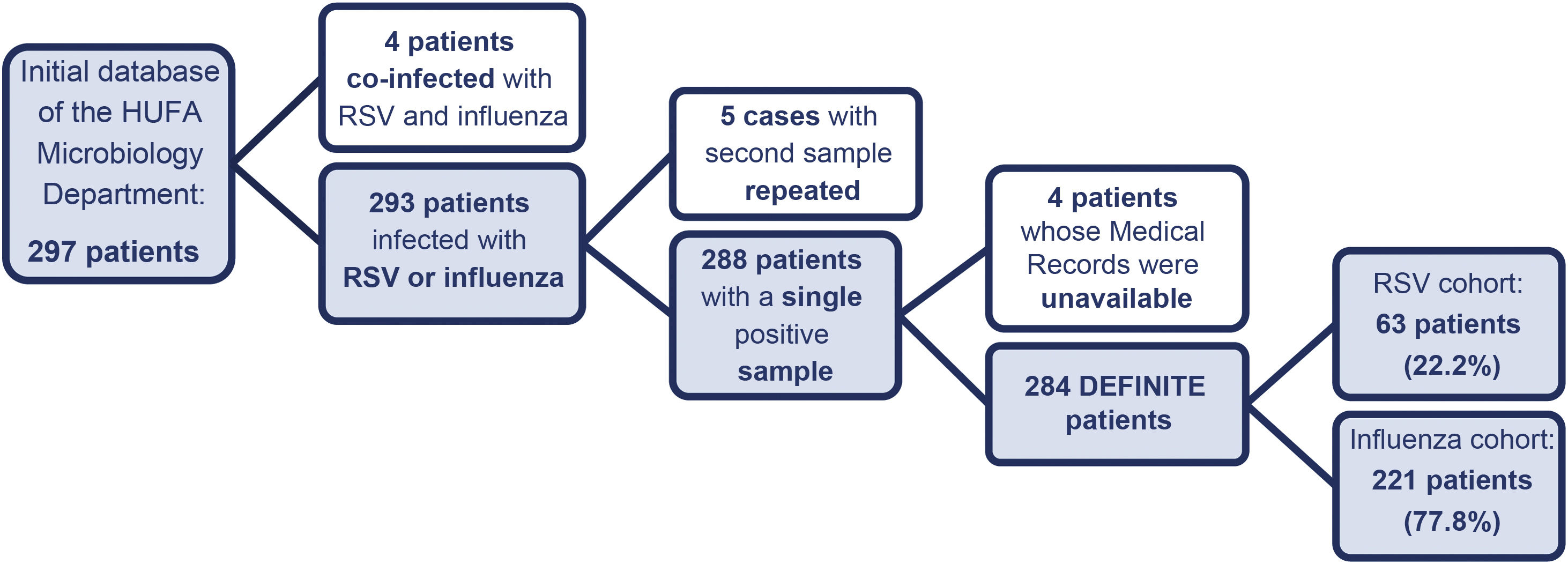
Materials and methodsWe conducted a retrospective observational cohort study at HUFA, analysing samples from adult patients (aged ≥18) positive for RSV and/or influenza processed in the HUFA Microbiology Laboratory from 28 November 2018 to 24 March 2019. In cases where there were two positive samples over the course of the period, only the first one was counted, whether for RSV or influenza, in the corresponding cohort. Also excluded from the study were cases co-infected simultaneously with the two viruses, as well as patients with insufficient information in their medical records (MR). Lastly, the resulting sample of patients was grouped into two independent RSV and influenza cohorts, in order make subsequent statistical comparisons. The study was assessed and approved by the HUFA Research Ethics Committee.
The Cobas Liat® System test for nucleic acids (Influenza A/B & RSV) was used for the microbiological diagnosis of the respiratory tract samples. This is an automated multiplex assay for reverse transcriptase polymerase chain reaction, which enables in vitro and real-time (20min) differentiation between the virus RNA for influenza A, influenza B and RSV in samples from patients with signs and symptoms of acute respiratory infection6.
All data were obtained through the electronic MR at HUFA (Selene platform) and the Madrid Region medical records computer system (Horus platform). We prospectively collected the information on the clinical process from the onset of the patient’s respiratory symptoms to the date of hospital discharge or the death of the patient, based on the medical record number of each patient included in the initial list provided by the HUFA Microbiology Department.
We collected the following variables: demographic characteristics; obesity (recorded as such in the MR); smoking; vaccination status (against influenza in the campaign at the time of the study and against pneumococcus on any occasion); dependence in basic activities of daily living (BADL); origin of the infection (community or hospital-acquired); baseline comorbidity according to the Charlson Index7; coronary and non-coronary heart disease (valve disease, arrhythmias, cardiomyopathy and others); cancer; immunosuppression (including long-term treatment with systemic glucocorticoids [≥5mg/day for ≥15 days]); symptoms and signs at diagnosis; treatment used (bronchodilators, inhaled and systemic corticosteroids, and antibiotic therapy); and investigations (chest X-ray, blood leucocyte count, and C-reactive protein [CRP] level in blood). According to the HUFA protocol, isolation precautions for droplets during the infectious period and treatment with oseltamivir were indicated for all patients admitted with confirmed influenza, while in cases with RSV, isolation precautions for droplets were indicated for immunosuppressed patients only.
In order to assess a patient's hospital outcome, the following were taken into account: complications (respiratory failure [oxygen blood pressure <60mmHg], respiratory co-infection, pneumonia, bacteraemia and sepsis); exacerbation of chronic diseases (chronic obstructive pulmonary disease [COPD], asthma, heart failure, arrhythmias, acute myocardial damage, cerebral ischaemia, decompensated diabetes, renal and liver failure); use of respiratory support (invasive mechanical ventilation [IMV] or non-invasive mechanical ventilation [NIMV]); admission to intensive care unit (ICU); mean length of hospital stay; and mortality.
Statistical analysis was performed with the software program SPSS® Statistics, version 25.0. Descriptive statistics included means and standard deviations for continuous variables and frequencies and percentages for categorical variables. To assess the association between categorical variables, we used Pearson’s χ2 test and Fisher’s exact test if appropriate, while Student’s t-test was used for continuous data. At the same time, multivariate logistic regression analyses were performed to establish which factors were independently associated with RSV infection. A p-value of <0.05 was considered statistically significant.
ResultsThe vast majority of the samples for analysis were collected from the upper respiratory tract (99.3%), while only a minority came from the lower respiratory tract (0.7%). The patient selection process according to the study inclusion criteria is shown in Fig. 1.
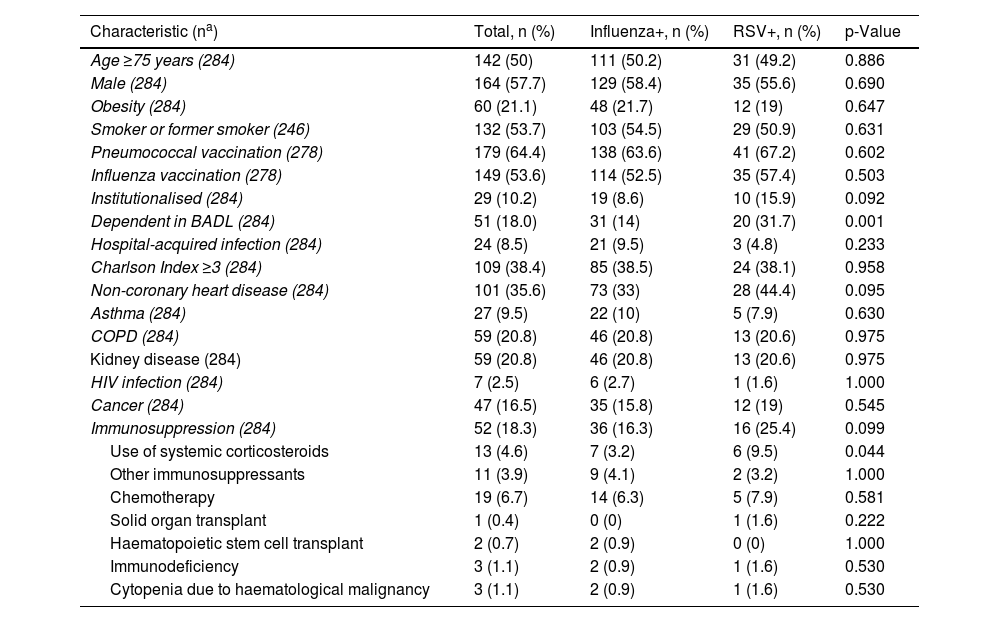
Of the 284 patients studied, 164 were male (57.7%), and the mean age was 71.57 years (±15.9 years). More than half were or had been smokers, and 21.1% were obese. With regard to underlying diseases, 52 (18.3%) suffered from some type of immunosuppression, while the mean comorbidity calculated according to the Charlson Index was 2.46 points (±2.26 points). In total, 29 of the patients (10.2%) lived in some type of institution, and pneumococcal and influenza vaccination rates were 64.4% and 53.6%, respectively (Table 1).
Epidemiological characteristics and baseline situation of the study patients and comparison between cases with influenza and with RSV.
| Characteristic (na) | Total, n (%) | Influenza+, n (%) | RSV+, n (%) | p-Value |
|---|---|---|---|---|
| Age ≥75 years (284) | 142 (50) | 111 (50.2) | 31 (49.2) | 0.886 |
| Male (284) | 164 (57.7) | 129 (58.4) | 35 (55.6) | 0.690 |
| Obesity (284) | 60 (21.1) | 48 (21.7) | 12 (19) | 0.647 |
| Smoker or former smoker (246) | 132 (53.7) | 103 (54.5) | 29 (50.9) | 0.631 |
| Pneumococcal vaccination (278) | 179 (64.4) | 138 (63.6) | 41 (67.2) | 0.602 |
| Influenza vaccination (278) | 149 (53.6) | 114 (52.5) | 35 (57.4) | 0.503 |
| Institutionalised (284) | 29 (10.2) | 19 (8.6) | 10 (15.9) | 0.092 |
| Dependent in BADL (284) | 51 (18.0) | 31 (14) | 20 (31.7) | 0.001 |
| Hospital-acquired infection (284) | 24 (8.5) | 21 (9.5) | 3 (4.8) | 0.233 |
| Charlson Index ≥3 (284) | 109 (38.4) | 85 (38.5) | 24 (38.1) | 0.958 |
| Non-coronary heart disease (284) | 101 (35.6) | 73 (33) | 28 (44.4) | 0.095 |
| Asthma (284) | 27 (9.5) | 22 (10) | 5 (7.9) | 0.630 |
| COPD (284) | 59 (20.8) | 46 (20.8) | 13 (20.6) | 0.975 |
| Kidney disease (284) | 59 (20.8) | 46 (20.8) | 13 (20.6) | 0.975 |
| HIV infection (284) | 7 (2.5) | 6 (2.7) | 1 (1.6) | 1.000 |
| Cancer (284) | 47 (16.5) | 35 (15.8) | 12 (19) | 0.545 |
| Immunosuppression (284) | 52 (18.3) | 36 (16.3) | 16 (25.4) | 0.099 |
| Use of systemic corticosteroids | 13 (4.6) | 7 (3.2) | 6 (9.5) | 0.044 |
| Other immunosuppressants | 11 (3.9) | 9 (4.1) | 2 (3.2) | 1.000 |
| Chemotherapy | 19 (6.7) | 14 (6.3) | 5 (7.9) | 0.581 |
| Solid organ transplant | 1 (0.4) | 0 (0) | 1 (1.6) | 0.222 |
| Haematopoietic stem cell transplant | 2 (0.7) | 2 (0.9) | 0 (0) | 1.000 |
| Immunodeficiency | 3 (1.1) | 2 (0.9) | 1 (1.6) | 0.530 |
| Cytopenia due to haematological malignancy | 3 (1.1) | 2 (0.9) | 1 (1.6) | 0.530 |
BADL: basic activities of daily living; COPD: chronic obstructive pulmonary disease; HIV: human immunodeficiency virus.
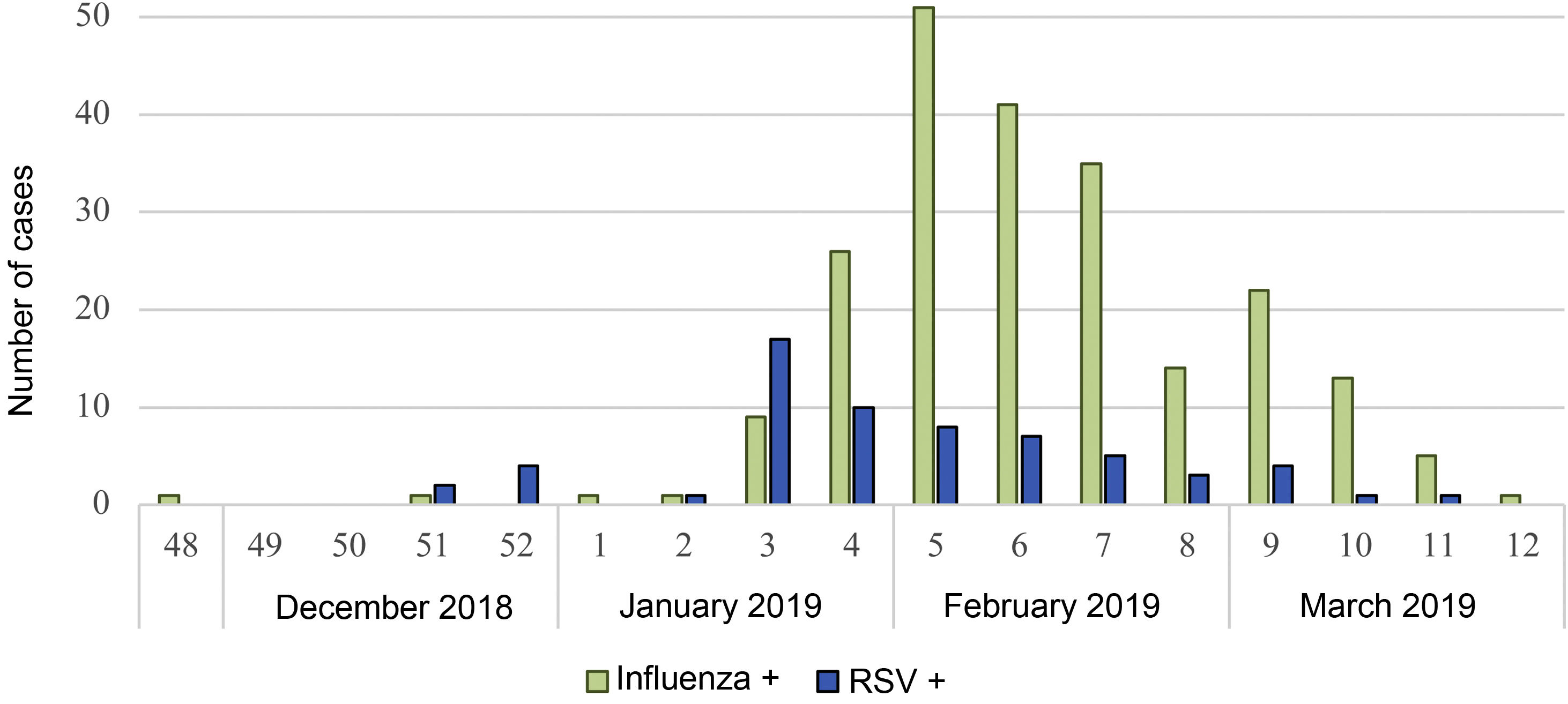
The time distribution of both viruses throughout the period in which the study took place is shown in Fig. 2. The maximum peak in RSV cases was reached in the third week of January 2019, while the peak in samples positive for influenza occurred during the first few days of February, when the number of RSV cases had already begun to decline.
In general, there were no significant differences between RSV-infected and influenza-infected in the distribution of most of the demographic characteristics and personal history (age, gender, obesity, smoking, Charlson Index and vaccination), as shown in Table 1. The only exceptions, found to be more common in the RSV-positive group, were the prevalence of living in some type of institution (15.9% vs 8.6%; p=0.09), non-coronary heart disease (44.4% vs 33%; p=0.09) and immunosuppression (25.4% vs 16.3%; p=0.09). Dependence in BADL (31.7% vs 14%; p=0.001) and long-term systemic corticosteroid therapy (9.5% vs 3.2%; p=0.04) were also significantly more common in RSV infection. Although the difference was not significant, RSV cases were much less often hospital-acquired (4.8% vs 9.5%; p=0.23).
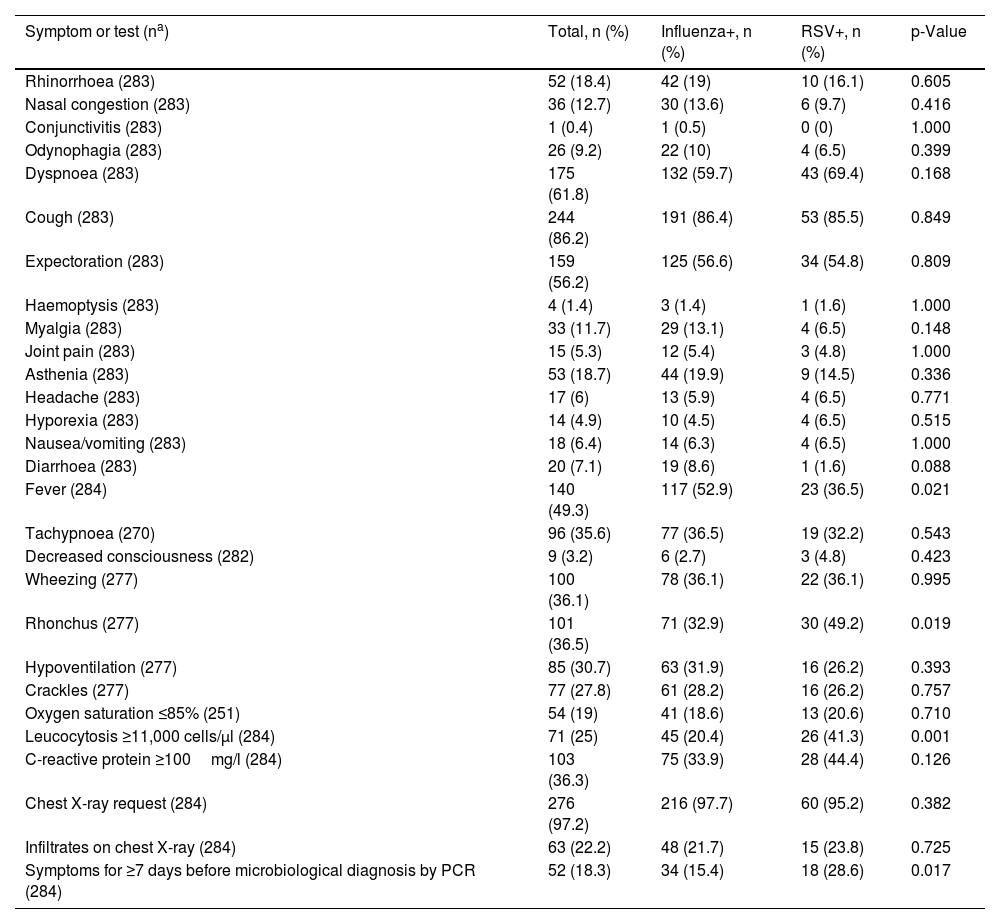
The differences between the signs and symptoms detected in the patients on arrival at the hospital are shown in Table 2. Comparing the two groups, fever was significantly less common in patients with RSV (36.5% vs 52.9%; p=0.02), as were diarrhoea (1.6% vs 8.6%; p=0.09) and myalgia (6.5% vs 13.1%; p=0.15), both of which showed the same trend. In contrast, patients diagnosed with RSV disease were more likely to report dyspnoea (69.4% vs 59.7%; p=0.16) and had a significantly higher prevalence of rhonchi on lung auscultation (49.2% vs 32.9%, p=0.02). The higher leucocyte count in the first blood test (10.2 vs 8.43×103 cell/μl; p=0.005) and the number of days with symptoms until microbiological diagnosis (5.63 vs 4.18 days, p=0.04) were statistically representative in favour of the RSV+ group.
Clinical manifestations and investigations performed in the study patients and comparison between cases with influenza and with RSV.
| Symptom or test (na) | Total, n (%) | Influenza+, n (%) | RSV+, n (%) | p-Value |
|---|---|---|---|---|
| Rhinorrhoea (283) | 52 (18.4) | 42 (19) | 10 (16.1) | 0.605 |
| Nasal congestion (283) | 36 (12.7) | 30 (13.6) | 6 (9.7) | 0.416 |
| Conjunctivitis (283) | 1 (0.4) | 1 (0.5) | 0 (0) | 1.000 |
| Odynophagia (283) | 26 (9.2) | 22 (10) | 4 (6.5) | 0.399 |
| Dyspnoea (283) | 175 (61.8) | 132 (59.7) | 43 (69.4) | 0.168 |
| Cough (283) | 244 (86.2) | 191 (86.4) | 53 (85.5) | 0.849 |
| Expectoration (283) | 159 (56.2) | 125 (56.6) | 34 (54.8) | 0.809 |
| Haemoptysis (283) | 4 (1.4) | 3 (1.4) | 1 (1.6) | 1.000 |
| Myalgia (283) | 33 (11.7) | 29 (13.1) | 4 (6.5) | 0.148 |
| Joint pain (283) | 15 (5.3) | 12 (5.4) | 3 (4.8) | 1.000 |
| Asthenia (283) | 53 (18.7) | 44 (19.9) | 9 (14.5) | 0.336 |
| Headache (283) | 17 (6) | 13 (5.9) | 4 (6.5) | 0.771 |
| Hyporexia (283) | 14 (4.9) | 10 (4.5) | 4 (6.5) | 0.515 |
| Nausea/vomiting (283) | 18 (6.4) | 14 (6.3) | 4 (6.5) | 1.000 |
| Diarrhoea (283) | 20 (7.1) | 19 (8.6) | 1 (1.6) | 0.088 |
| Fever (284) | 140 (49.3) | 117 (52.9) | 23 (36.5) | 0.021 |
| Tachypnoea (270) | 96 (35.6) | 77 (36.5) | 19 (32.2) | 0.543 |
| Decreased consciousness (282) | 9 (3.2) | 6 (2.7) | 3 (4.8) | 0.423 |
| Wheezing (277) | 100 (36.1) | 78 (36.1) | 22 (36.1) | 0.995 |
| Rhonchus (277) | 101 (36.5) | 71 (32.9) | 30 (49.2) | 0.019 |
| Hypoventilation (277) | 85 (30.7) | 63 (31.9) | 16 (26.2) | 0.393 |
| Crackles (277) | 77 (27.8) | 61 (28.2) | 16 (26.2) | 0.757 |
| Oxygen saturation ≤85% (251) | 54 (19) | 41 (18.6) | 13 (20.6) | 0.710 |
| Leucocytosis ≥11,000 cells/μl (284) | 71 (25) | 45 (20.4) | 26 (41.3) | 0.001 |
| C-reactive protein ≥100mg/l (284) | 103 (36.3) | 75 (33.9) | 28 (44.4) | 0.126 |
| Chest X-ray request (284) | 276 (97.2) | 216 (97.7) | 60 (95.2) | 0.382 |
| Infiltrates on chest X-ray (284) | 63 (22.2) | 48 (21.7) | 15 (23.8) | 0.725 |
| Symptoms for ≥7 days before microbiological diagnosis by PCR (284) | 52 (18.3) | 34 (15.4) | 18 (28.6) | 0.017 |
PCR: polymerase chain reaction.
The need for hospital admission was similar between RSV and influenza (approximately 87%), with admission to internal medicine being the most common. Therapeutic coverage with oseltamivir was 84.2% in patients with influenza, and 4.8% of RSV+ cases and 81.9% of cases with influenza were kept in isolation with droplet precautions in place. Both the mean duration of antibiotic therapy (7.15 vs 6.47 days; p=0.17) and the use of bronchodilators (87.3% vs 79.6%; p=0.16) showed a tendency to be higher in patients with RSV.
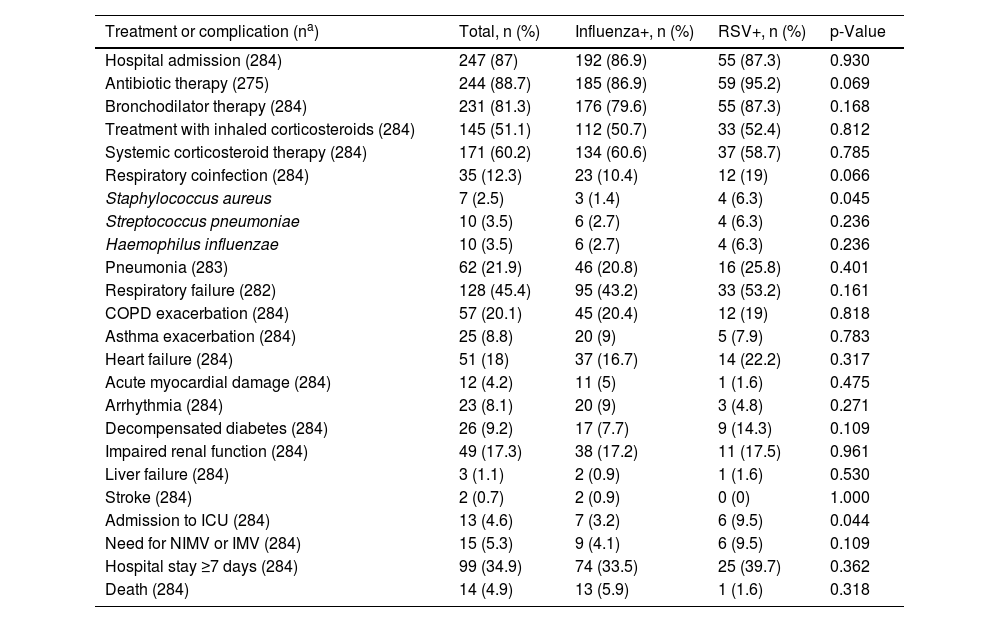
With regard to outcomes and complications (Table 3), the difference between the rates of respiratory co-infection found in the two viral diseases was striking, with 19% for RSV and 10.4% for influenza (p=0.06), the difference in the number of samples with Staphylococcus aureus being significant (6.3% vs 1.4%; p=0.04). There was a similar higher prevalence of respiratory failure and use of mechanical ventilation in RSV cases (53.2% vs 43.2%; p=0.16; 9.5% vs 4.1%; p=0.11, respectively). Admission to the HUFA ICU was higher among RSV+ patients (9.5% vs 3.2%; p=0.04), although no significant differences were found in mean hospital stay and mortality rates.
Treatment, complications and outcome for the study patients and comparison between cases with influenza and with RSV.
| Treatment or complication (na) | Total, n (%) | Influenza+, n (%) | RSV+, n (%) | p-Value |
|---|---|---|---|---|
| Hospital admission (284) | 247 (87) | 192 (86.9) | 55 (87.3) | 0.930 |
| Antibiotic therapy (275) | 244 (88.7) | 185 (86.9) | 59 (95.2) | 0.069 |
| Bronchodilator therapy (284) | 231 (81.3) | 176 (79.6) | 55 (87.3) | 0.168 |
| Treatment with inhaled corticosteroids (284) | 145 (51.1) | 112 (50.7) | 33 (52.4) | 0.812 |
| Systemic corticosteroid therapy (284) | 171 (60.2) | 134 (60.6) | 37 (58.7) | 0.785 |
| Respiratory coinfection (284) | 35 (12.3) | 23 (10.4) | 12 (19) | 0.066 |
| Staphylococcus aureus | 7 (2.5) | 3 (1.4) | 4 (6.3) | 0.045 |
| Streptococcus pneumoniae | 10 (3.5) | 6 (2.7) | 4 (6.3) | 0.236 |
| Haemophilus influenzae | 10 (3.5) | 6 (2.7) | 4 (6.3) | 0.236 |
| Pneumonia (283) | 62 (21.9) | 46 (20.8) | 16 (25.8) | 0.401 |
| Respiratory failure (282) | 128 (45.4) | 95 (43.2) | 33 (53.2) | 0.161 |
| COPD exacerbation (284) | 57 (20.1) | 45 (20.4) | 12 (19) | 0.818 |
| Asthma exacerbation (284) | 25 (8.8) | 20 (9) | 5 (7.9) | 0.783 |
| Heart failure (284) | 51 (18) | 37 (16.7) | 14 (22.2) | 0.317 |
| Acute myocardial damage (284) | 12 (4.2) | 11 (5) | 1 (1.6) | 0.475 |
| Arrhythmia (284) | 23 (8.1) | 20 (9) | 3 (4.8) | 0.271 |
| Decompensated diabetes (284) | 26 (9.2) | 17 (7.7) | 9 (14.3) | 0.109 |
| Impaired renal function (284) | 49 (17.3) | 38 (17.2) | 11 (17.5) | 0.961 |
| Liver failure (284) | 3 (1.1) | 2 (0.9) | 1 (1.6) | 0.530 |
| Stroke (284) | 2 (0.7) | 2 (0.9) | 0 (0) | 1.000 |
| Admission to ICU (284) | 13 (4.6) | 7 (3.2) | 6 (9.5) | 0.044 |
| Need for NIMV or IMV (284) | 15 (5.3) | 9 (4.1) | 6 (9.5) | 0.109 |
| Hospital stay ≥7 days (284) | 99 (34.9) | 74 (33.5) | 25 (39.7) | 0.362 |
| Death (284) | 14 (4.9) | 13 (5.9) | 1 (1.6) | 0.318 |
COPD: chronic obstructive pulmonary disease; ICU: intensive care unit; NIMV: non-invasive mechanical ventilation; IMV: invasive mechanical ventilation.
As can be seen in the multivariate analysis in Fig. 3, dependence in BADL, having cancer, previous use of corticosteroids, elevated blood CRP, co-infection by S. aureus and admission to ICU were at least twice as common in patients with RSV. In contrast, fever was more common in patients with influenza.
DiscussionAlthough there is much literature on RSV infection in the paediatric population2,8, there have been few studies on the behaviour of this virus in adults in Spain since Reina et al. published the first data9,10. Our aim with this study was therefore to help make the existing clinical knowledge on this acute respiratory infection more complete and highlight the significant role it plays in the over-18 age group, where we found that around one in five microbiological tests requested for patients with flu-like symptoms requiring hospital care are due to RSV rather than influenza. Although it is true that there are many similarities between these two diseases11,12, our results show that there are also some differences.
In the first place, we found that RSV is a virus that mainly circulates in the winter months, but its epidemiological wave is two weeks earlier than that of influenza, a finding consistent with other studies13. While no significant differences were found between the baseline characteristics of the patients belonging to both cohorts, RSV predominantly affected those with non-coronary heart disease14 and immunosuppression. We should particularly mention the association we found between RSV infection and iatrogenic immunosuppression due to long-term administration of corticosteroids. Also interesting was the worse condition of vulnerability and frailty found in the cohort affected by RSV, with a greater number of cancer patients15 and people dependent in BADL, perhaps in relation to the origin of their infections, most often from closed institutions (residences, medium-to-long stay hospitals and prisons).
The proportions of oseltamivir therapy and isolation precautions for droplets achieved among patients with influenza were satisfactory. However, despite these isolation measures being carried out mainly in those affected by influenza, the percentage of hospital-acquired infections found in this group was almost double that of RSV+ cases. In spite of the lack of data in the literature in this regard, this finding could indicate a greater transmissibility of the influenza virus compared to RSV, or that the diagnosis of RSV occurred in a more developed and less contagious phase of the disease, as the mean delay in the microbiological detection of RSV from the onset of the symptoms was longer than that for influenza. This in turn could be related to the lack of symptoms and/or signs indicating severity, such as fever, at the onset of RSV respiratory disease.
In line with previous studies16, RSV patients were more likely to develop leucocytosis and elevated levels of acute phase reactants in blood such as CRP. These blood test results may be explained by bacterial co-infection, detected mostly in sputum samples from RSV+ patients, especially for S. aureus, which is a novel finding compared to other published articles16,17. Also of interest, and possibly related, is the high rate of pulmonary rhonchi detected on lung auscultation and the large proportion of people prescribed antibiotic therapy (95.2%) in RSV, which has already been reported in previous studies16,17. However, this does not correspond with the above-mentioned lack of fever among RSV+ cases, which is surprising given the greater inflammatory response they seem to develop. In any event, with regard to the prescribing of antibiotics, we believe this to be a clear scenario of inappropriate use of antibiotics18, as only a quarter of RSV+ patients ended up being diagnosed with pneumonia, and only 20% with a bacterial co-infection.
Compared to influenza, RSV infection had a higher prevalence of bronchospasm, and consequently greater use of bronchodilators, but unlike other authors, we did not find higher rates of COPD and asthma exacerbation12,14. Further interesting findings, highlighting the importance of RSV as a cause of morbidity, were the higher rate of respiratory failure and greater use of ICU among RSV+ patients, with the need for respiratory support being double that for influenza. As found in previous studies12,19, the mean length of hospital stay, although slightly higher for RSV, was shown to be statistically similar in influenza. However, the short-term mortality rate turned out to be higher in influenza, although once again it was not significant in the statistical analysis. That does contrast with the published reports that have demonstrated a higher long-term mortality rate in patients infected with RSV14,20.
Apart from the different prevalence of fever found at diagnosis, the data obtained for the patients’ clinical symptoms seem to confirm that any real chance of distinguishing between the conditions caused by the two viruses is limited3,4. It is therefore essential that we use the new molecular techniques to confirm the viral diagnosis5, as this will enable earlier detection and better specific therapeutic management of each infection. While for influenza we have antivirals such as oseltamivir, for RSV it is accepted that there is a need for further research on new therapeutic targets1,21 and vaccines, and studies have recently been conducted on the design of formulations providing cross-immunisation against both viruses22. In any event, simply being aware of RSV as the cause of a large proportion of the severe respiratory symptoms occurring in winter should have beneficial effects, including reducing the indiscriminate use of antibiotics for viral infections.
The limitations of our project include, firstly, those inherent to retrospective studies, where the collection of variables may not be complete and there is greater difficulty in controlling confounding factors. Secondly, the disparity in the epidemiological curve of influenza with respect to RSV probably led to an underestimation of the actual numbers of RSV over the course of the season. This is due to the ordering of tests for multiple viral diagnosis at HUFA essentially being based on the circulation pattern of influenza and the fact that it was clinically suspected by healthcare professionals. Thirdly, we have to acknowledge the small sample size, which limits the conclusions that can be extrapolated to the general population, as the study collected data from a single winter season, and from hospital patients in a specific location. In contrast, the main strength of our study is the large number of epidemiological, clinical and outcome variables we have analysed, making it one of the most exhaustive series of RSV infection in adults reported to date. Another strong point is the fact of having used a cohort of patients with confirmed infection, that is, selected solely for their positive result in the diagnostic test, which made it possible to record and compare a wide range of forms of clinical severity, both for RSV and for influenza. A final important factor is that this study was carried out prior to the start of the COVID-19 pandemic caused by SARS-CoV-2, so we do not know how these three viruses are going to behave in the post-pandemic period.
ConclusionsIn conclusion, in addition to corroborating the burden of morbidity and mortality caused by influenza each year, this study proves that RSV is indeed an important cause of respiratory disease during the winter months, with a major impact on the most vulnerable adults, oncology patients and people on long-term corticosteroid therapy. Compared to influenza, RSV infection was also associated with a greater inflammatory response and more bacterial co-infection with S. aureus. These findings, added to the potential this virus has for causing severe disease in patients, leading to life-threatening situations, such as requiring admission to ICU, highlight the importance of physicians being fully aware of RSV as a diagnostic entity, as they will have to continue to manage it while new preventive and therapeutic options are being developed.
FundingThe authors declare that this study did not receive any type of funding.
Conflicts of interestThere are no conflicts of interest.