Whooping cough in patients aged under 3 months has higher rates of morbimortality. Hospitalisation and treatment with azithromycin is generally recommended. Many patients with cough without other signs of alarm, are admitted and started antibiotic therapy until a result of Bordetella-PCR is available. This technique, when performed urgently, can provide the diagnosis in a few hours. The objective of this study is to determine if its generalisation in the Emergency Department allows to improve patient management.
MethodsRetrospective cohort study of patients aged under 3 months who underwent Bordetella-PCR testing from upper respiratory tract secretions since March 2011 to December 2017. From December 2015 the test was performed urgently.
ResultsOne hundred and fifty-eight PCR were performed, 16 (10%) were positive for B. pertussis. Negative results (142; 90%) were divided in 2 cohorts: conventional-PCR, with 74 cases, and urgent-PCR, with 68 cases. The 2 groups were homogeneous in terms of clinical and analytical characteristics. In the urgent-PCR group there was 18% reduction in chest X-rays performed (p=0.008). There were 33 (48.5%) patients admitted in the urgent-PCR group, compared to 49 (66.2%) in the conventional-PCR (p=0.042). Antibiotic treatment was initiated in 32% of the patients in the urgent-PCR group compared to 67% in the conventional-PCR group (p=0.000047), without observing any significant increase in the number of visits to the Emergency Department or worse clinical performance.
ConclusionsThe introduction of urgent PCR in the Emergency Department is a useful tool in the management of infants under 3 months of age with suspected pertussis, since it can avoid unnecessary admissions, diagnostic tests and antibiotic treatments.
En pacientes menores de 3 meses con sospecha de tosferina se recomienda ingreso y tratamiento con azitromicina debido a su mayor morbimortalidad, por lo que muchos pacientes con tos sin otros signos de alarma ingresan con antibioterapia hasta obtener el resultado de la PCR de Bordetella. La realización de esta técnica de forma urgente proporciona el diagnóstico en pocas horas. Nuestro objetivo fue determinar si su introducción en los servicios de Urgencias mejoraba el manejo de estos pacientes.
MétodosEstudio de cohortes histórico de pacientes menores de 3 meses a los que se realizó en Urgencias la PCR de Bordetella de secreciones respiratorias desde marzo de 2011 hasta diciembre de 2017. A partir de diciembre de 2015 era procesada de forma urgente.
ResultadosSe realizaron 158 PCR, 16 (10%) de las cuales resultaron positivas para B. pertussis. Los resultados negativos (142; 90%) se dividen en 2 grupos de estudio: PCR-convencional, con 74 casos, y PCR-urgente, con 68 casos. Los 2 grupos son homogéneos en cuanto a características clínicas y analíticas. En el grupo PCR-urgente se realizaron un 18% menos de radiografías de tórax (p=0,008) e ingresaron 33 pacientes (48,5%), frente a 49 (66,2%) en el grupo PCR-convencional (p=0,042). Recibió tratamiento antibiótico el 32% en el grupo PCR-urgente frente al 67% en el PCR-convencional (p=0,000047), sin aumento significativo de las reconsultas en Urgencias ni peor evolución.
ConclusionesLa PCR urgente de Bordetella es una herramienta útil en los servicios de Urgencias para el manejo de los lactantes menores de 3 meses con sospecha de tosferina, ya que puede evitar ingresos, pruebas y tratamientos antibióticos innecesarios.
Whooping cough is an endemic disease worldwide, caused by acute infection of the upper respiratory tract caused by Bordetella pertussis (85–95%) and Bordetella parapertussis (5–15%).1 The World Health Organisation declaration describing whooping cough as a “re-emerging” disease2 and the public alarm after the last epidemic peaks3 have increased the number of patients attending or being referred to Accident and Emergency departments to confirm or rule out the diagnosis of this disease. The clinical criteria are insufficient to differentiate it from the generally milder “pertussis-like syndromes” caused by a group of bacterial and viral agents such as Mycoplasma pneumoniae, adenovirus and respiratory syncytial virus,4,5 and microbiological study is necessary for a definitive diagnosis. The technique of choice is currently polymerase chain reaction (PCR) for Bordetella species in nasopharyngeal aspirate (NPA). This test provides a rapid diagnosis within a few hours (2–24h depending on the technique used), in addition to being highly sensitive (90.7–97%) and specific (93–100%) compared to cell culture (sensitivity 58–64%, specificity 100%).6–8 However, PCR has the disadvantage that it needs both infrastructure and human and technical resources in order to be carried out urgently. In most hospitals in our region it is not possible for the sample to be processed at the time of collection. This results in a delay in obtaining results and thus a definitive diagnosis takes up to 48–72h.4
Although whooping cough can affect all age groups, patients under 3–4 months old are the main risk group, as they tend to have more nonspecific symptoms and higher morbidity and mortality rates. When whooping cough is suspected in this age range, hospital admission and starting antibiotic therapy with macrolides are recommended, due to the risk of rapid progression and potentially lethal complications.4,5,9 This recommendation has led many patients under the age of three months with pertussis-like cough but no other concerning factors to be admitted and started on antibiotics until the result of the Bordetella PCR arrived.
In 2015, our centre introduced the ability to process the NPA sample and performing the Bordetella PCR immediately after collection for patients in this age range, obtaining the definitive diagnosis by PCR in approximately 4h.
The aim of this study was to determine whether or not the introduction of urgently processed PCR avoided unnecessary admissions, additional tests and antibiotic treatments in patients under the age of three months with clinically suspected whooping cough.
MethodsThis was a retrospective cohort study, which included patients under three months of age for whom a Bordetella PCR in NPA was requested by the Paediatric Accident and Emergency Department (A&E), from March 2011 to December 2017. Exclusion criteria were the existence of previous pathology (heart disease, chronic respiratory disease, multiple malformation syndrome or prematurity <37 weeks) and having started antibiotic treatment prior to the A&E consultation.
The technique used to process the NPA samples was real-time PCR. From 2011–2015 the test was carried out in a delayed manner in all cases, with the result obtained in 24–48h. Then, the potential for urgent PCR was introduced for patients under the age of three months, so from 2015–2017 most of the samples were analysed immediately after collection, with the definitive result obtained in 3–4h. We can therefore distinguish two study groups: the first, in which the patients’ samples were processed conventionally (C-PCR); and the second, in which they were processed urgently (U-PCR). The four patients in whom the result was indeterminate due to inhibition of the sample were first included in the C-PCR group, and then in the end the result was not obtained until the conventional 24h, after the test needed to be repeated with a new sample. Repeating the test urgently would involve very young infants being in A&E for at least 9–10h. As that would delay the start of antibiotic therapy if the patient actually had whooping cough, and would expose the patient to a greater risk of contagion by other microorganisms, it was agreed with the Microbiology Service that the new sample would be processed using the routine method in the cases. This also avoided overloading the on-call microbiologist. These patients are generally admitted and started on antibiotic treatment until the PCR result is obtained.
In both groups, the Diagenode PCR (Diagenode Diagnostics, Liège, Belgium) was performed in the BD Max system (Becton Dickinson, Franklin Lakes, NJ, USA), an automated multiplex real-time PCR targeting insertion sequence 481 for the diagnosis of B. pertussis and insertion sequence 1001 for the detection of B. parapertussis. The technique takes approximately 2.5h, with a first manual sample preparation stage and the master mix of 15–20min. Both the extraction and amplification processes are carried out automatically, which significantly reduces the risk of contamination.10
All the samples were cultured immediately in Charcoal agar and incubated at 35–37°C in a humid environment for 7–10 days. The colonies likely to be Bordetella spp. were identified by MALDI-TOF MS (Bruker Daltonik GmbH, Bremen, Germany).
The results were analysed using the data processing programme IBM SPSS Statistics version 20. In the descriptive analysis the results are presented with measures of centralisation and dispersion (mean and standard deviation, median and interquartile range [IQR]) in the case of quantitative variables and using absolute (n) and relative (%) frequencies for qualitative variables. The Chi-squared test or Fisher's exact test were used to study the association of qualitative variables, and Student's t test and the Mann–Whitney U test were used for independent quantitative samples.
ResultsA total of 175 Bordetella spp. PCR were performed on 175 patients under three months of age with suspected whooping cough, of which we analysed 158. The remaining 17 cases were excluded because the information in the medical records was incomplete, did not meet the inclusion criteria, or met one or more of the exclusion criteria.
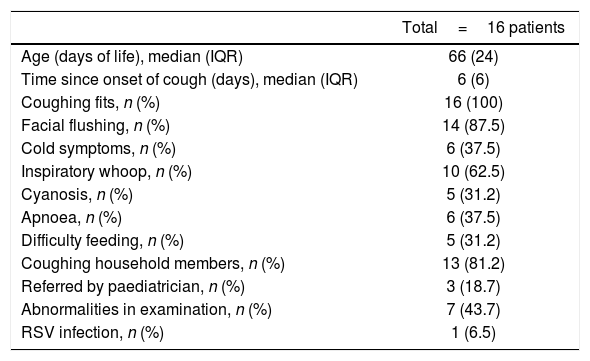
Of the 158 PCR analysed, 16 (10%) were positive for B. pertussis and 142 (90%) were negative. All (100%) of the positive results corresponded to the C-PCR group. The clinical characteristics of these patients are shown in Table 1.
Clinical characteristics of the patients with positive Bordetella spp. PCR.
| Total=16 patients | |
|---|---|
| Age (days of life), median (IQR) | 66 (24) |
| Time since onset of cough (days), median (IQR) | 6 (6) |
| Coughing fits, n (%) | 16 (100) |
| Facial flushing, n (%) | 14 (87.5) |
| Cold symptoms, n (%) | 6 (37.5) |
| Inspiratory whoop, n (%) | 10 (62.5) |
| Cyanosis, n (%) | 5 (31.2) |
| Apnoea, n (%) | 6 (37.5) |
| Difficulty feeding, n (%) | 5 (31.2) |
| Coughing household members, n (%) | 13 (81.2) |
| Referred by paediatrician, n (%) | 3 (18.7) |
| Abnormalities in examination, n (%) | 7 (43.7) |
| RSV infection, n (%) | 1 (6.5) |
PCR: polymerase chain reaction; IQR: interquartile range; RSV: respiratory syncytial virus.
As regards the results of the cultures, nine were positive (56.2% of the cases with positive PCR), and all (100%) of the cases with negative PCR were negative. Of all the PCR analysed, 11 (6.9%) were initially indeterminate due to inhibition of the sample, four in the U-PCR group and seven in the C-PCR group, all with negative results after analysis of a new sample. Indeterminate tests are included for statistical analysis in the C-PCR group, as explained in the materials and methods section.
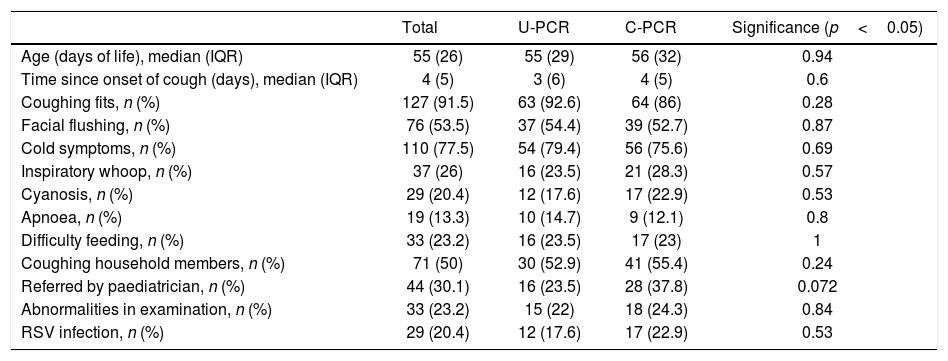
In the analysis of all the negative results, 74 cases belonged to the C-PCR cohort and 68 to the U-PCR, and corresponded to 72 males and 70 females with a median age of 55 days of life (IQR 26), with no significant differences between study groups (p=0.94).
Table 2 shows the clinical characteristics of the patients with negative PCR, including variables which could represent a bias when analysing differences in rates of hospitalisation and initiation of antibiotic therapy. The two groups were homogeneous with respect to all the variables analysed.
Clinical characteristics of the patients with negative Bordetella spp. PCR.
| Total | U-PCR | C-PCR | Significance (p<0.05) | |
|---|---|---|---|---|
| Age (days of life), median (IQR) | 55 (26) | 55 (29) | 56 (32) | 0.94 |
| Time since onset of cough (days), median (IQR) | 4 (5) | 3 (6) | 4 (5) | 0.6 |
| Coughing fits, n (%) | 127 (91.5) | 63 (92.6) | 64 (86) | 0.28 |
| Facial flushing, n (%) | 76 (53.5) | 37 (54.4) | 39 (52.7) | 0.87 |
| Cold symptoms, n (%) | 110 (77.5) | 54 (79.4) | 56 (75.6) | 0.69 |
| Inspiratory whoop, n (%) | 37 (26) | 16 (23.5) | 21 (28.3) | 0.57 |
| Cyanosis, n (%) | 29 (20.4) | 12 (17.6) | 17 (22.9) | 0.53 |
| Apnoea, n (%) | 19 (13.3) | 10 (14.7) | 9 (12.1) | 0.8 |
| Difficulty feeding, n (%) | 33 (23.2) | 16 (23.5) | 17 (23) | 1 |
| Coughing household members, n (%) | 71 (50) | 30 (52.9) | 41 (55.4) | 0.24 |
| Referred by paediatrician, n (%) | 44 (30.1) | 16 (23.5) | 28 (37.8) | 0.072 |
| Abnormalities in examination, n (%) | 33 (23.2) | 15 (22) | 18 (24.3) | 0.84 |
| RSV infection, n (%) | 29 (20.4) | 12 (17.6) | 17 (22.9) | 0.53 |
PCR: polymerase chain reaction; C-PCR: conventional polymerase chain reaction; U-PCR: urgent polymerase chain reaction; IQR: interquartile range; RSV: respiratory syncytial virus.
In most of the patients, the time since onset of the symptoms was short, with a median of four days (IQR 5); 77% had cold symptoms and 91.5% coughing fits; 20% had cyanosis during the coughing episodes and 13%, apnoea. Only half of the patients had an epidemic environment, with coughing household members, and 30% had been referred by their paediatrician to rule out whooping cough.
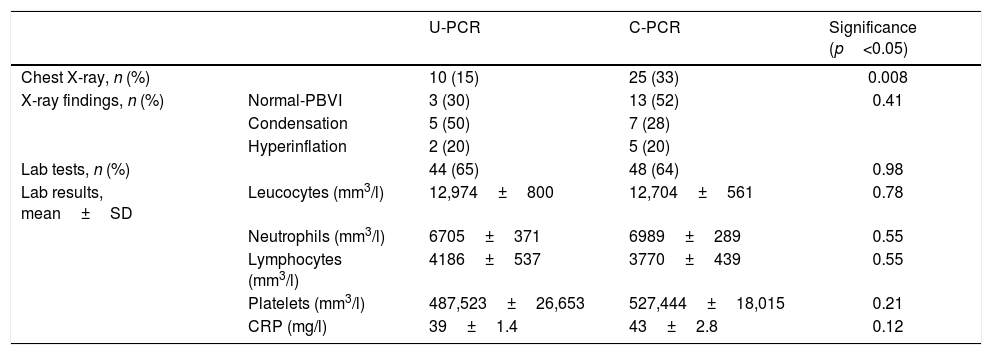
Table 3 shows the diagnostic tests performed on patients with negative PCR. Blood tests were performed on 48 patients (64%) in the C-PCR group and 44 (65%) in the U-PCR group, with no significant differences between the two groups in terms of the test rate or the results. However, significantly fewer chest X-rays were performed in the U-PCR group, with 10 X-rays (15%), versus 25 (33%) in the C-PCR group (p=0.008), with no significant differences in the radiological findings.
Tests performed on the patients with negative Bordetella spp. PCR.
| U-PCR | C-PCR | Significance (p<0.05) | ||
|---|---|---|---|---|
| Chest X-ray, n (%) | 10 (15) | 25 (33) | 0.008 | |
| X-ray findings, n (%) | Normal-PBVI | 3 (30) | 13 (52) | 0.41 |
| Condensation | 5 (50) | 7 (28) | ||
| Hyperinflation | 2 (20) | 5 (20) | ||
| Lab tests, n (%) | 44 (65) | 48 (64) | 0.98 | |
| Lab results, mean±SD | Leucocytes (mm3/l) | 12,974±800 | 12,704±561 | 0.78 |
| Neutrophils (mm3/l) | 6705±371 | 6989±289 | 0.55 | |
| Lymphocytes (mm3/l) | 4186±537 | 3770±439 | 0.55 | |
| Platelets (mm3/l) | 487,523±26,653 | 527,444±18,015 | 0.21 | |
| CRP (mg/l) | 39±1.4 | 43±2.8 | 0.12 |
PBVI: peribronchovascular infiltrates; PCR: polymerase chain reaction; C-PCR: conventional polymerase chain reaction; U-PCR: urgent polymerase chain reaction; CRP: C-reactive protein; IQR: interquartile range.
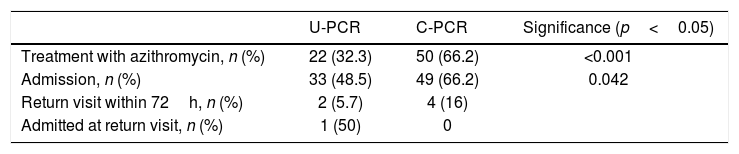
Of the patients with a negative result, 72 received antibiotic therapy with azithromycin, with large differences between one group and another: 22 treated cases (32%) in the U-PCR group and 50 (67%) in the C-PCR group, with a degree of significance of p=0.000047. There were also significant differences in terms of hospital admission, with 33 admissions (48.5%) in the U-PCR group versus 49 admissions (66.2%) in the C-PCR group (p=0.042). Of the 33 patients admitted with negative urgent PCR, the admissions could be explained by: apnoea in ten patients (30%); cyanosis in 12 (36%); difficulty feeding in nine (27%); altered physical examination in eight (24%); or a combination of various symptoms.
The length of hospital stay was the same in both groups, with a median of three days (IQR 3), p=0.79. Three patients had to be admitted to intensive care due to bronchiolitis, all belonging to the C-PCR group. Of the discharged patients, four from the C-PCR group and two from the U-PCR group returned to A&E; one patient was admitted for 24h with bronchiolitis (Table 4).
Admission and antibiotic therapy in patients with negative Bordetella spp. PCR.
| U-PCR | C-PCR | Significance (p<0.05) | |
|---|---|---|---|
| Treatment with azithromycin, n (%) | 22 (32.3) | 50 (66.2) | <0.001 |
| Admission, n (%) | 33 (48.5) | 49 (66.2) | 0.042 |
| Return visit within 72h, n (%) | 2 (5.7) | 4 (16) | |
| Admitted at return visit, n (%) | 1 (50) | 0 |
PCR: polymerase chain reaction; C-PCR: conventional polymerase chain reaction; U-PCR: urgent polymerase chain reaction.
According to our literature review, this is the first study to assess the utility of urgently processed PCR in patients under three months of age with suspected pertussis.
Despite broad vaccine coverage in the paediatric population, pertussis is still a public health problem. This is particularly true for patients under three months of age, who not only have higher morbidity and mortality rates when they suffer from the disease, but are also at higher risk of iatrogenic complications when pertussis is suspected. There is no clinical criteria-based protocol with sufficient sensitivity and specificity for establishing the diagnosis of pertussis,4 although Bordetella spp. PCR is at present considered by many authors to be the gold standard for diagnosis.11 Use of this technique performed urgently in our study significantly reduced the number of admissions of patients in this age range falsely suspected of having pertussis from 66.2% to 48.5% (p<0.05). We believe that this difference could be greater, as in some medical records, paediatricians justified the admission of patients with negative urgent PCR while awaiting the culture results, probably unaware that culture has a lower sensitivity than PCR. Urgent PCR also reduced the number of patients who received antibiotic therapy with azithromycin, with 35% fewer children being treated after the urgent negative result (p<0.001), without increasing the rate of return visits to A&E or leading to a worse outcome.
As far as additional tests were concerned, urgent PCR reduced chest X-rays in our study by 18% (p=0.008), but not the performing of blood tests. This is probably because while waiting for the PCR result, many paediatricians prefer to carry out blood tests to rule out lymphocytosis or thrombocytosis as indicators of severity and initiate immediate treatment if detected.
Adult patients can also contract whooping cough and behave as transmitters. General A&E departments therefore need to have awareness of the disease in order to make a differential diagnosis in any patient with a long-lasting cough, start treatment early and adopt the necessary measures to prevent transmission.12 Although not analysed in our study, urgent Bordetella spp. PCR could also be a useful measure to help establish isolation measures.
In November 2015, vaccination was introduced for pregnant women in our Autonomous Region, and since 2016 it has been implemented throughout Spain,3 with the aim of protecting the most vulnerable infants, those under three months of age. Since 2010 in Spain, whooping cough has been identified as being in a situation of sustained outbreak.3,13 However, we found no studies which only included a population under three months of age. In our study, all the PCR positive for B. pertussis were before vaccination in pregnancy started. The last positive PCR in this age group was in December 2015, a month after the vaccinating began, suggesting, as demonstrated in other studies, that the vaccination programme has been a success.14,15
As a limitation, as ours was a retrospective study, we were not able to collect data on the vaccination of patients or their mothers during pregnancy as this information is not included in many of the medical records. Nevertheless, it is estimated that in 2016 the national coverage was 81.6%.3 Due to the cyclical epidemiology of pertussis, future incidence peaks would need to be analysed to assess the effectiveness of the vaccination programme.
Another limitation of our study is the fact that, being retrospective, it was not possible to reliably verify whether or not the urgent PCR result changed the decision to admit or start antibiotic therapy in each particular case.
From a conceptual point of view, the four urgent PCR results which were indeterminate were analysed in the C-PCR group, as the treating doctor's information was based around an unknown result until the test could be repeated as a conventional PCR, and the situation would therefore have played out as for a patient in the C-PCR group. However, this could be a limitation when analysing the benefits of the urgent test, as in 5.5% of cases (4/72), according to our series, decisions could not be made based on the result of that test.
In conclusion, Bordetella spp. PCR requested urgently by A&E departments is a useful tool in the management of patients under three months of age with suspected pertussis, as it can avoid unnecessary admissions, chest X-rays and antibiotics. Paediatricians need to be aware of the value of this test and its limitations, and make good use of it. The availability of an automated technique, a Microbiology Department with continuous 24h provision, and operational protocols for clinically suspected pertussis in infants under three months could all result in savings, both financially and in terms of the intangible losses associated with a hospital admission for the families. It would be interesting to carry out future prospective and cost-benefit studies to assess the efficiency of this measure.
Conflicts of interestThe authors declare that they have no conflicts of interest.
Please cite this article as: González-Bertolín I, Ochoa-Fernández BM, Bloise I, de Ceano-Vivas-La Calle M, Ruíz-Domínguez JA. PCR urgente de Bordetella en lactantes menores de 3 meses, una herramienta útil en el Servicio de Urgencias Pediátricas. Enferm Infecc Microbiol Clin. 2021;39:174–178.