Sexual intercourse is currently the main route of HIV infection in Spain. Despite decreases in new infections among women and drug users, the rate remains stable in men. The aim of this study was to assess risk behaviour and HIV awareness in a sample of young adults in Spain.
MethodsA cross-sectional, observational, descriptive study was performed on a non-HIV infected sample, using a questionnaire on sexual health and HIV awareness adapted from the Spanish National Institute of Statistics. A sexual risk variable was included (high and low), which was classified as high if subjects had had three or more sexual partners and did not always use a condom in all their sexual encounters.
Results243 subjects were included (65.6% women) aged between 16 and 36 years (mean=25.7; SD=4.1) (16–24 years: 134 subjects; 25–29 years: 60 subjects; over 30years: 47 subjects). Approximately 40.9% said that they used a condom in all sexual relations and 61% did not perceive any risk of infection. There were no significant differences in awareness of infection routes between the high and low risk profiles. Washing after sex, having few partners, spermicide use and having undetectable viral load were protective measures significantly associated with differences in sexual risk (p<0.05).
ConclusionsThe main finding of the study was the underestimation of risk of infection, analysed after differences found between self-assessment and sexual risk. Both positive and negative results were found concerning HIV awareness.
El contacto sexual es actualmente en España la primera vía de contagio de VIH. Pese a los descensos en el número de nuevas infecciones en mujeres y consumo de drogas, en hombres se mantiene estable. El presente estudio pretende evaluar conductas de riesgo y conocimientos sobre VIH en una muestra de jóvenes en España.
MétodosSe realizó un estudio observacional descriptivo transversal utilizando un cuestionario sobre salud sexual y conocimiento sobre el VIH adaptado del Instituto Nacional de Estadística. El grupo estuvo compuesto por jóvenes no infectados por VIH. Se incluyó la variable riesgo sexual (alto y bajo), siendo de riesgo alto los sujetos que habían tenido tres o más parejas y no utilizaban preservativo en todas las relaciones.
ResultadosSe encuestaron 243 jóvenes (65,6% mujeres) de entre 16 y 36años (media=25,7; DE=4,1) (16-24años: 134 sujetos; 25-29años, 60 sujetos; más de 30años, 47 sujetos). El 40,9% contestaron que utilizaban el preservativo en todas sus relaciones y el 61% que no perciben ningún riesgo de infección. De forma mayoritaria no se encuentran diferencias significativas en conocimiento sobre vías de transmisión entre los grupos de alto y de bajo riesgo. Los métodos de protección que se asociaron significativamente con las diferencias en riesgo sexual fueron lavarse tras las relaciones sexuales, tener pocas parejas, uso de espermicidas y carga viral indetectable (p<0,05).
ConclusionesEl principal resultado del estudio es la infravaloración personal de riesgo indicado según las diferencias encontradas entre la valoración personal y el índice de riesgo sexual. Se encuentran resultados tanto positivos como negativos en cuanto al conocimiento sobre el VIH.
In 2015, according to the annual report on the epidemiology of HIV issued by the Ministry of Health,1 approximately 150,000 people over the age of 15 in Spain were living with HIV. In the same period, the percentage of men who have sex with men (MSM) in the HIV-infected population increased, while the prevalence in the heterosexual population and among injecting drug users decreased.2 According to data from 2016,1 the trend in new infections among women shows a tendency to decrease while in men it remains stable, with sexual contact currently the main route of transmission.2
High-risk sexual behaviour usually begins in adolescence3 and more than half of new infections worldwide occur in people aged 15–24.4 Unprotected sex is the main cause of new infections among adolescents and young adults.5,6 Although new strategies have emerged such as pre-exposure prophylaxis (PrEP),7 prevention through condom use continues to be the main method recommended based on their accessibility and degree of effectiveness. However, the biggest issue in terms of prevention continues to be lack of condom use, an aspect which is mediated by each young person's range of knowledge and trends in practices.8–11
Having up-to-date data on knowledge about HIV and sexual practices is essential to our understanding of how risk is evolving, in order to develop effective prevention programmes. The aim of this study was to: (a) determine how much the population sample of young people living in Spain knew about HIV; (b) identify the proportion of risky sexual practices among the subjects, and (c) analyse the behaviours reported in different areas according to the risk profile subjects were classified as having, and observe any differences between the groups.
MethodThis was a cross-sectional descriptive study carried out through a survey online and in physical format in a hospital context. The subjects were recruited by incidental sampling (without HIV infection, resident in Spain and 15–36 years of age) using the snowball method.
All participants were guaranteed anonymity and the voluntary nature of participation. The study was approved by the ethics committees of all participating hospitals. This study formed part of the Spanish cohort of paediatric patients infected with HIV, CoRISpe (Cohorte Pediátrica de la Red de Investigación en SIDA [Paediatric cohort of the AIDS Research Network]), NeuroCoRispe and FARO projects. We interviewed 241 young people not infected with HIV living in Spain aged 16–36 (mean [M]=25.79, standard deviation [SD]=4.14).
For the measurement of the variables, we used an adapted version of the Questionnaire on Health and Sexual Habits in Relation to HIV used by the Instituto Nacional de Estadística (INE) [Spanish Institute of Statistics].12 Questions were included about sociodemographic characteristics, drug use, knowledge about HIV and sexual behaviour. Two risk profiles for HIV transmission were created and the 230 subjects who provided information for this area were defined as high (48.1%, 116 subjects) if they did not always use condoms and had had three or more sexual partners, or low (47.3%, 114 subjects) if they always used condoms or had had fewer than three sexual partners. The subjects were also divided into three age groups according to the criterion in the publication by Arnett13: 16–25 (134 subjects); 25–29 (60 subjects) and over 30 (47 subjects).
The collected data were analysed by the statistical package SPSS Statistics for Windows. v.17. We used descriptive statistics (M, SD and percentages) to compare variables within the sample, Student's t-test for age differences between risk groups, and the chi-square test as a measure of association. When the percentage of expected values exceeded the chi-square validity criterion, the association was analysed by Fisher's exact test. Univariate analyses were performed to search for association between variables in the areas of sociodemographic characteristics, sexual behaviour, drug use and knowledge about transmission routes and protection methods.
The choice of analysis contemplated was to obtain significant univariate associations for specific analysis and comparison with previous related studies. Multivariate analyses were ruled out because of the large number of categories of variables in a restricted sample size, as this leads to a large number of association groups and makes it difficult to obtain accurate results.
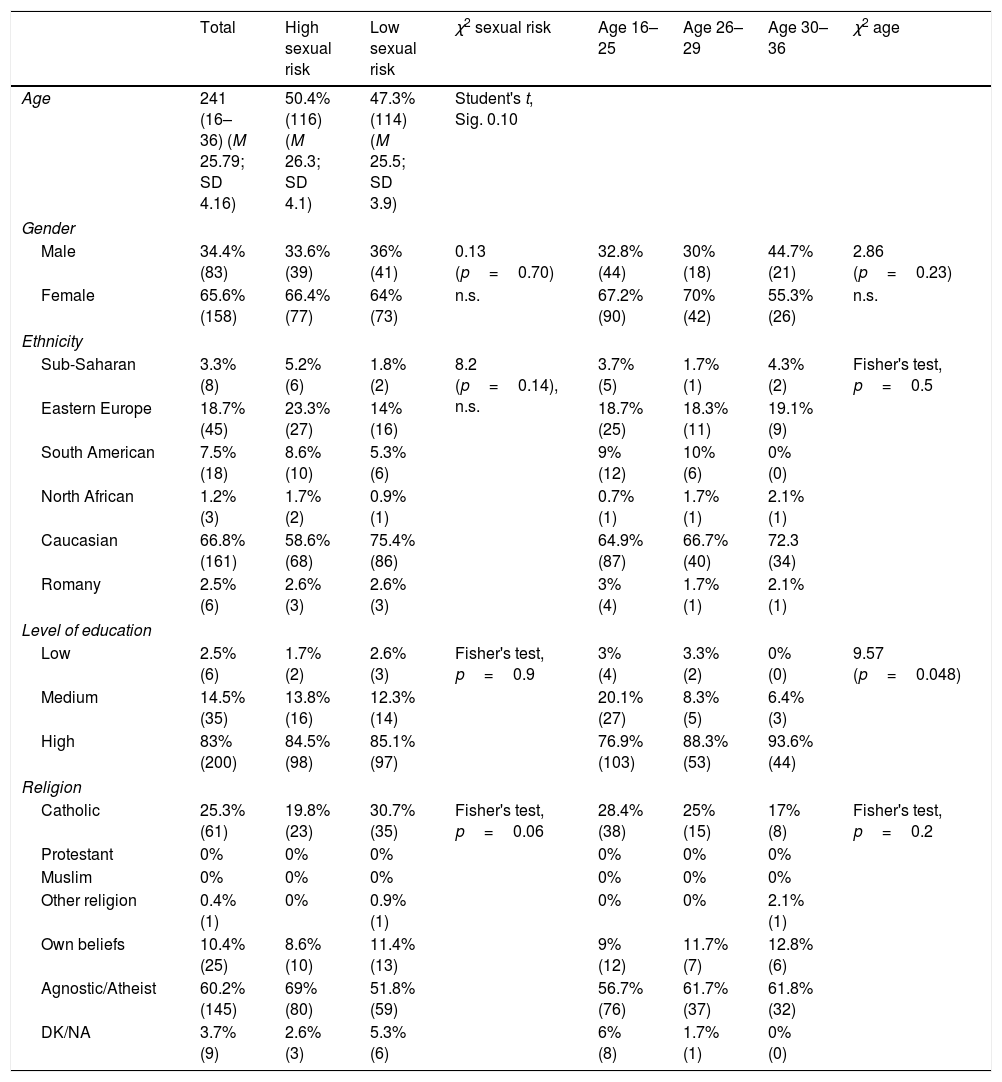
ResultsWe included 243 young people. Their sociodemographic characteristics are shown in Table 1. The mean age was 25.79 (SD 4.14 years) and 34.4% were male, 83% had a high level of education and 2.5% only primary or compulsory secondary education.
Sociodemographic characteristics of the young people.
| Total | High sexual risk | Low sexual risk | χ2 sexual risk | Age 16–25 | Age 26–29 | Age 30–36 | χ2 age | |
|---|---|---|---|---|---|---|---|---|
| Age | 241 (16–36) (M 25.79; SD 4.16) | 50.4% (116) (M 26.3; SD 4.1) | 47.3% (114) (M 25.5; SD 3.9) | Student's t, Sig. 0.10 | ||||
| Gender | ||||||||
| Male | 34.4% (83) | 33.6% (39) | 36% (41) | 0.13 (p=0.70) | 32.8% (44) | 30% (18) | 44.7% (21) | 2.86 (p=0.23) |
| Female | 65.6% (158) | 66.4% (77) | 64% (73) | n.s. | 67.2% (90) | 70% (42) | 55.3% (26) | n.s. |
| Ethnicity | ||||||||
| Sub-Saharan | 3.3% (8) | 5.2% (6) | 1.8% (2) | 8.2 (p=0.14), n.s. | 3.7% (5) | 1.7% (1) | 4.3% (2) | Fisher's test, p=0.5 |
| Eastern Europe | 18.7% (45) | 23.3% (27) | 14% (16) | 18.7% (25) | 18.3% (11) | 19.1% (9) | ||
| South American | 7.5% (18) | 8.6% (10) | 5.3% (6) | 9% (12) | 10% (6) | 0% (0) | ||
| North African | 1.2% (3) | 1.7% (2) | 0.9% (1) | 0.7% (1) | 1.7% (1) | 2.1% (1) | ||
| Caucasian | 66.8% (161) | 58.6% (68) | 75.4% (86) | 64.9% (87) | 66.7% (40) | 72.3 (34) | ||
| Romany | 2.5% (6) | 2.6% (3) | 2.6% (3) | 3% (4) | 1.7% (1) | 2.1% (1) | ||
| Level of education | ||||||||
| Low | 2.5% (6) | 1.7% (2) | 2.6% (3) | Fisher's test, p=0.9 | 3% (4) | 3.3% (2) | 0% (0) | 9.57 (p=0.048) |
| Medium | 14.5% (35) | 13.8% (16) | 12.3% (14) | 20.1% (27) | 8.3% (5) | 6.4% (3) | ||
| High | 83% (200) | 84.5% (98) | 85.1% (97) | 76.9% (103) | 88.3% (53) | 93.6% (44) | ||
| Religion | ||||||||
| Catholic | 25.3% (61) | 19.8% (23) | 30.7% (35) | Fisher's test, p=0.06 | 28.4% (38) | 25% (15) | 17% (8) | Fisher's test, p=0.2 |
| Protestant | 0% | 0% | 0% | 0% | 0% | 0% | ||
| Muslim | 0% | 0% | 0% | 0% | 0% | 0% | ||
| Other religion | 0.4% (1) | 0% | 0.9% (1) | 0% | 0% | 2.1% (1) | ||
| Own beliefs | 10.4% (25) | 8.6% (10) | 11.4% (13) | 9% (12) | 11.7% (7) | 12.8% (6) | ||
| Agnostic/Atheist | 60.2% (145) | 69% (80) | 51.8% (59) | 56.7% (76) | 61.7% (37) | 61.8% (32) | ||
| DK/NA | 3.7% (9) | 2.6% (3) | 5.3% (6) | 6% (8) | 1.7% (1) | 0% (0) | ||
High sexual risk: 3 or more partners and does not always use a condom. Low sexual risk: less than 3 partners and/or always uses a condom.
Level of education. Low: compulsory primary or secondary education; middle: high school or middle grade vocational training; high: higher grade vocational training or university studies.
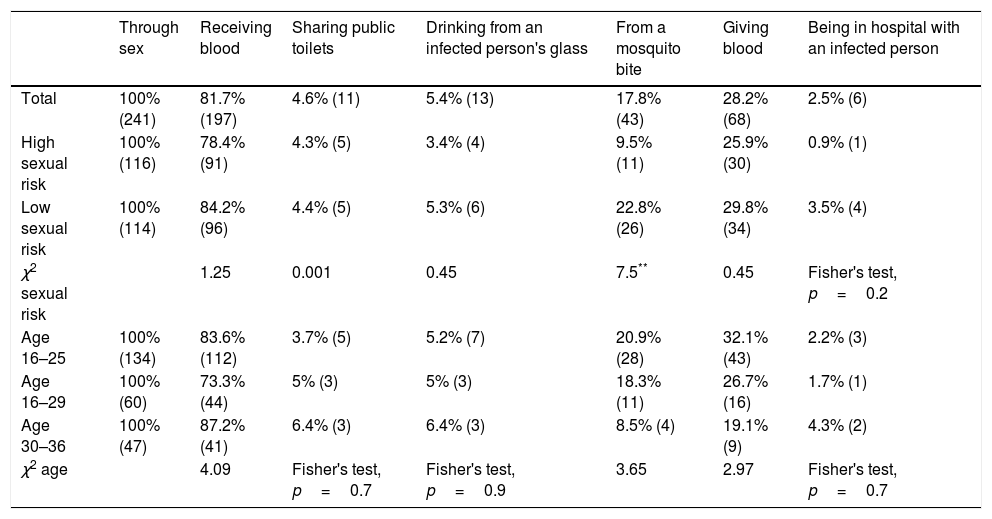
In terms of knowledge about HIV transmission routes, from Table 2 we can see that 4.6% of the respondents said HIV transmission occurs when sharing toilets or drinking from an infected person's glass, and 17.8% that one way may be from a mosquito bite. The subjects had high correct response rates on sexual relations (100%) and receiving blood (81.7%). Comparing according to sexual risk, no significant differences were found between the high-risk and low-risk groups, except in infection by mosquito bite, which 22.8% of the low-risk subjects said was a transmission route (p<0.01). The comparisons according to age group showed similar response patterns between groups, with no significant differences.
Affirmative responses about HIV transmission according to sexual risk and age, and association rates.
| Through sex | Receiving blood | Sharing public toilets | Drinking from an infected person's glass | From a mosquito bite | Giving blood | Being in hospital with an infected person | |
|---|---|---|---|---|---|---|---|
| Total | 100% (241) | 81.7% (197) | 4.6% (11) | 5.4% (13) | 17.8% (43) | 28.2% (68) | 2.5% (6) |
| High sexual risk | 100% (116) | 78.4% (91) | 4.3% (5) | 3.4% (4) | 9.5% (11) | 25.9% (30) | 0.9% (1) |
| Low sexual risk | 100% (114) | 84.2% (96) | 4.4% (5) | 5.3% (6) | 22.8% (26) | 29.8% (34) | 3.5% (4) |
| χ2 sexual risk | 1.25 | 0.001 | 0.45 | 7.5** | 0.45 | Fisher's test, p=0.2 | |
| Age 16–25 | 100% (134) | 83.6% (112) | 3.7% (5) | 5.2% (7) | 20.9% (28) | 32.1% (43) | 2.2% (3) |
| Age 16–29 | 100% (60) | 73.3% (44) | 5% (3) | 5% (3) | 18.3% (11) | 26.7% (16) | 1.7% (1) |
| Age 30–36 | 100% (47) | 87.2% (41) | 6.4% (3) | 6.4% (3) | 8.5% (4) | 19.1% (9) | 4.3% (2) |
| χ2 age | 4.09 | Fisher's test, p=0.7 | Fisher's test, p=0.9 | 3.65 | 2.97 | Fisher's test, p=0.7 |
Chi squared.
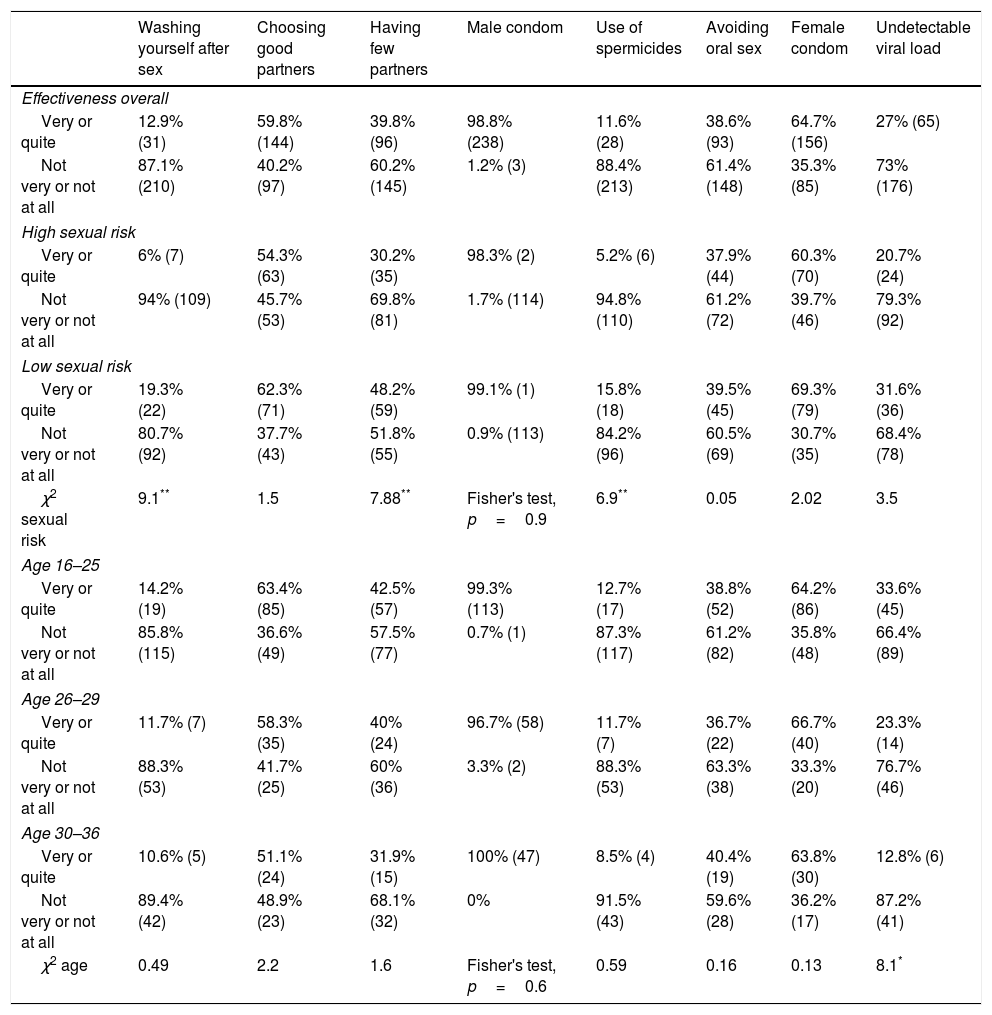
Table 3 shows the subjects’ responses about measures of protection against infection, with 19.3% of low-risk subjects saying that washing after sex is an effective form of protection and 15.8% saying the use of spermicides was very or quite effective.
Knowledge about the effectiveness of forms of protection against HIV overall and according to sexual risk and association rates, grouped by high or low effectiveness.
| Washing yourself after sex | Choosing good partners | Having few partners | Male condom | Use of spermicides | Avoiding oral sex | Female condom | Undetectable viral load | |
|---|---|---|---|---|---|---|---|---|
| Effectiveness overall | ||||||||
| Very or quite | 12.9% (31) | 59.8% (144) | 39.8% (96) | 98.8% (238) | 11.6% (28) | 38.6% (93) | 64.7% (156) | 27% (65) |
| Not very or not at all | 87.1% (210) | 40.2% (97) | 60.2% (145) | 1.2% (3) | 88.4% (213) | 61.4% (148) | 35.3% (85) | 73% (176) |
| High sexual risk | ||||||||
| Very or quite | 6% (7) | 54.3% (63) | 30.2% (35) | 98.3% (2) | 5.2% (6) | 37.9% (44) | 60.3% (70) | 20.7% (24) |
| Not very or not at all | 94% (109) | 45.7% (53) | 69.8% (81) | 1.7% (114) | 94.8% (110) | 61.2% (72) | 39.7% (46) | 79.3% (92) |
| Low sexual risk | ||||||||
| Very or quite | 19.3% (22) | 62.3% (71) | 48.2% (59) | 99.1% (1) | 15.8% (18) | 39.5% (45) | 69.3% (79) | 31.6% (36) |
| Not very or not at all | 80.7% (92) | 37.7% (43) | 51.8% (55) | 0.9% (113) | 84.2% (96) | 60.5% (69) | 30.7% (35) | 68.4% (78) |
| χ2 sexual risk | 9.1** | 1.5 | 7.88** | Fisher's test, p=0.9 | 6.9** | 0.05 | 2.02 | 3.5 |
| Age 16–25 | ||||||||
| Very or quite | 14.2% (19) | 63.4% (85) | 42.5% (57) | 99.3% (113) | 12.7% (17) | 38.8% (52) | 64.2% (86) | 33.6% (45) |
| Not very or not at all | 85.8% (115) | 36.6% (49) | 57.5% (77) | 0.7% (1) | 87.3% (117) | 61.2% (82) | 35.8% (48) | 66.4% (89) |
| Age 26–29 | ||||||||
| Very or quite | 11.7% (7) | 58.3% (35) | 40% (24) | 96.7% (58) | 11.7% (7) | 36.7% (22) | 66.7% (40) | 23.3% (14) |
| Not very or not at all | 88.3% (53) | 41.7% (25) | 60% (36) | 3.3% (2) | 88.3% (53) | 63.3% (38) | 33.3% (20) | 76.7% (46) |
| Age 30–36 | ||||||||
| Very or quite | 10.6% (5) | 51.1% (24) | 31.9% (15) | 100% (47) | 8.5% (4) | 40.4% (19) | 63.8% (30) | 12.8% (6) |
| Not very or not at all | 89.4% (42) | 48.9% (23) | 68.1% (32) | 0% | 91.5% (43) | 59.6% (28) | 36.2% (17) | 87.2% (41) |
| χ2 age | 0.49 | 2.2 | 1.6 | Fisher's test, p=0.6 | 0.59 | 0.16 | 0.13 | 8.1* |
Chi squared.
The protection methods which were significantly associated with sexual risk were washing after sex (p<0.01), having few partners (p<0.01) and the use of spermicides (p<0.01). Response trends were not linear in all cases, and higher percentages of correct responses were found in high-risk subjects than in low-risk subjects.
When determining associations according to age group, significant associations were only found with respect to undetectable viral load, in which younger subjects had a higher correct response rate. Also in Table 3, the results show little variation with respect to age group, with mostly wrong answers being found in the variable of choosing good partners.
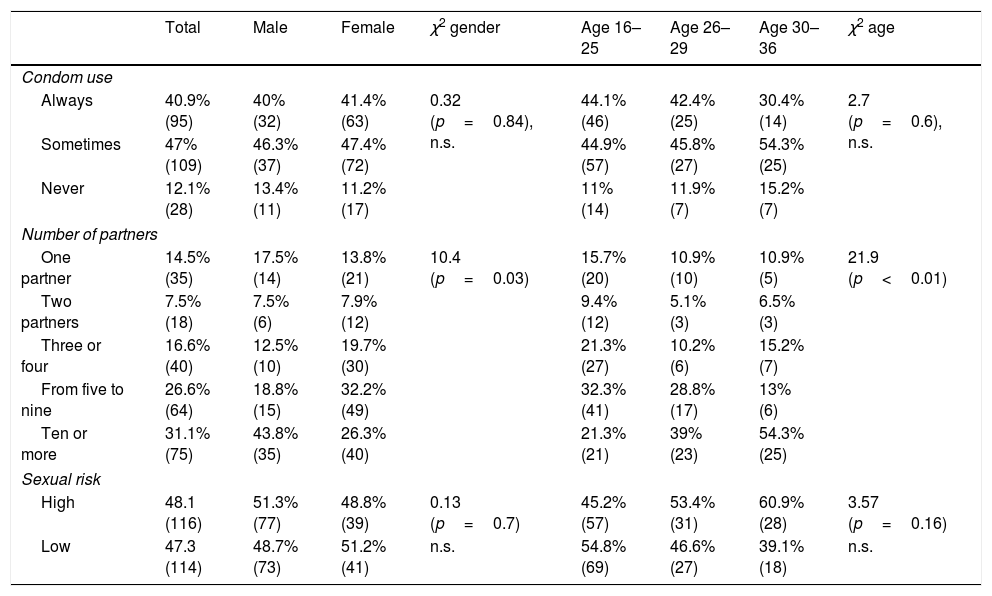
Sexual behaviourWith regard to the risk profile, Table 4 shows that less than half of the young people said that they used condoms in all their sexual relations (40.9%), with no significant differences by gender or level of education. In terms of number of partners, over 74.3% had had three or more partners over the course of their lives, with men more likely to have had ten or more partners (43.8% of men compared to 26.3% of women). Significant associations were also found between the number of partners subjects had had and the actual risk of infection (p=0.00). Breaking down the figures, 48.1% of the young people had a profile considered as high risk (48.7% of males and 51.2% of females, p=0.7). The results by age group are very similar to those filtered according to sexual risk and, once again, there was significant association with the number of partners; a higher percentage of subjects over the age of 30 having had ten or more. There was no such difference in the use of condoms.
Risky sexual behaviour and profile according to gender and age.
| Total | Male | Female | χ2 gender | Age 16–25 | Age 26–29 | Age 30–36 | χ2 age | |
|---|---|---|---|---|---|---|---|---|
| Condom use | ||||||||
| Always | 40.9% (95) | 40% (32) | 41.4% (63) | 0.32 (p=0.84), n.s. | 44.1% (46) | 42.4% (25) | 30.4% (14) | 2.7 (p=0.6), n.s. |
| Sometimes | 47% (109) | 46.3% (37) | 47.4% (72) | 44.9% (57) | 45.8% (27) | 54.3% (25) | ||
| Never | 12.1% (28) | 13.4% (11) | 11.2% (17) | 11% (14) | 11.9% (7) | 15.2% (7) | ||
| Number of partners | ||||||||
| One partner | 14.5% (35) | 17.5% (14) | 13.8% (21) | 10.4 (p=0.03) | 15.7% (20) | 10.9% (10) | 10.9% (5) | 21.9 (p<0.01) |
| Two partners | 7.5% (18) | 7.5% (6) | 7.9% (12) | 9.4% (12) | 5.1% (3) | 6.5% (3) | ||
| Three or four | 16.6% (40) | 12.5% (10) | 19.7% (30) | 21.3% (27) | 10.2% (6) | 15.2% (7) | ||
| From five to nine | 26.6% (64) | 18.8% (15) | 32.2% (49) | 32.3% (41) | 28.8% (17) | 13% (6) | ||
| Ten or more | 31.1% (75) | 43.8% (35) | 26.3% (40) | 21.3% (21) | 39% (23) | 54.3% (25) | ||
| Sexual risk | ||||||||
| High | 48.1 (116) | 51.3% (77) | 48.8% (39) | 0.13 (p=0.7) | 45.2% (57) | 53.4% (31) | 60.9% (28) | 3.57 (p=0.16) |
| Low | 47.3 (114) | 48.7% (73) | 51.2% (41) | n.s. | 54.8% (69) | 46.6% (27) | 39.1% (18) | n.s. |
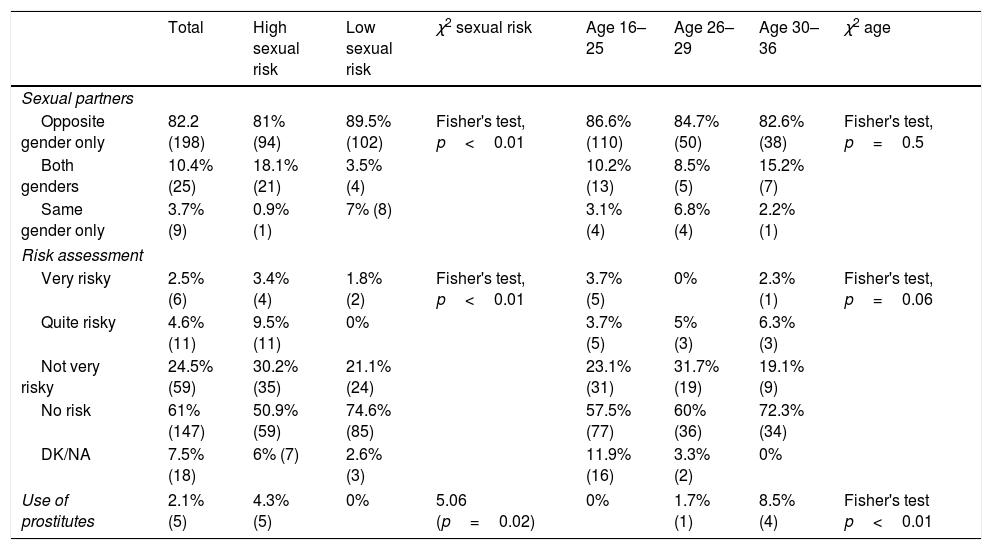
Table 5 shows that 82.2% of the subjects reported having relations with partners of the opposite sex only. The greatest difference regarding sexual risk was found in the subjects who reported having both male and female sexual partners (18.1% of high risk vs 3.5% of low risk, p<0.01). Among high-risk subjects, 81.1% said that their personal perception was of little or no risk of infection, compared to 95.7% of low-risk subjects who responded in the same way (p<0.01). Also among high-risk subjects, 4.3% reported having been clients of prostitution at some time, but no subjects in the low-risk group did (p=0.02).
Number of partners and personal assessment of risk and use of prostitutes according to sexual risk.
| Total | High sexual risk | Low sexual risk | χ2 sexual risk | Age 16–25 | Age 26–29 | Age 30–36 | χ2 age | |
|---|---|---|---|---|---|---|---|---|
| Sexual partners | ||||||||
| Opposite gender only | 82.2 (198) | 81% (94) | 89.5% (102) | Fisher's test, p<0.01 | 86.6% (110) | 84.7% (50) | 82.6% (38) | Fisher's test, p=0.5 |
| Both genders | 10.4% (25) | 18.1% (21) | 3.5% (4) | 10.2% (13) | 8.5% (5) | 15.2% (7) | ||
| Same gender only | 3.7% (9) | 0.9% (1) | 7% (8) | 3.1% (4) | 6.8% (4) | 2.2% (1) | ||
| Risk assessment | ||||||||
| Very risky | 2.5% (6) | 3.4% (4) | 1.8% (2) | Fisher's test, p<0.01 | 3.7% (5) | 0% | 2.3% (1) | Fisher's test, p=0.06 |
| Quite risky | 4.6% (11) | 9.5% (11) | 0% | 3.7% (5) | 5% (3) | 6.3% (3) | ||
| Not very risky | 24.5% (59) | 30.2% (35) | 21.1% (24) | 23.1% (31) | 31.7% (19) | 19.1% (9) | ||
| No risk | 61% (147) | 50.9% (59) | 74.6% (85) | 57.5% (77) | 60% (36) | 72.3% (34) | ||
| DK/NA | 7.5% (18) | 6% (7) | 2.6% (3) | 11.9% (16) | 3.3% (2) | 0% | ||
| Use of prostitutes | 2.1% (5) | 4.3% (5) | 0% | 5.06 (p=0.02) | 0% | 1.7% (1) | 8.5% (4) | Fisher's test p<0.01 |
The results obtained focusing on age groups do not show significant differences in the gender of partners, or in the personal assessment of risk, although here the p-value is very close to significance. In the three groups, most of the subjects said overall that their perceived risk was low. Significant associations were found in the use of prostitutes, although the number of subjects giving affirmative responses was very small.
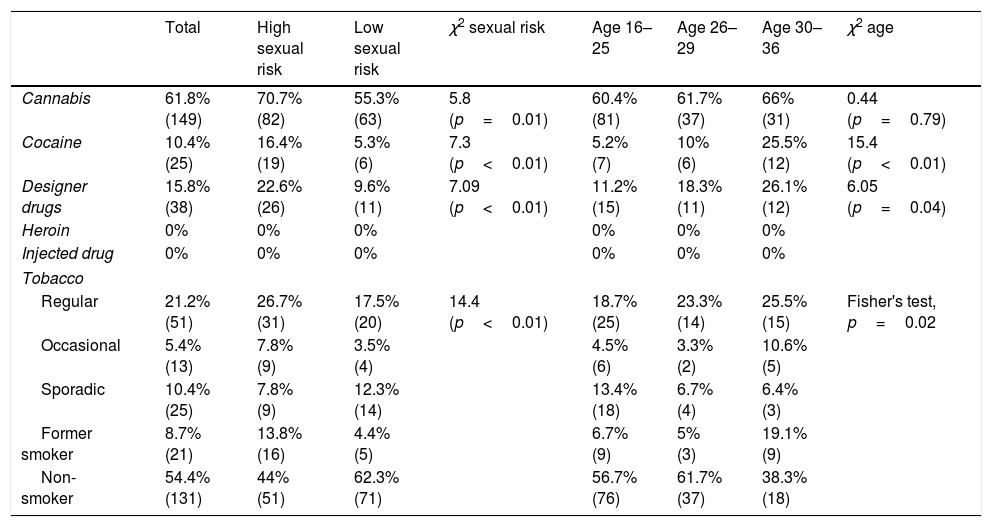
Drug useOf all cases in which there was an affirmative response, a higher percentage of high-risk subjects than low-risk subjects had used drugs at some point (Table 6). None reported injecting drug use. Drug use (at least once) was significantly associated with the high-risk profile in all cases: cannabis (p=0.01); cocaine (p<0.01); designer drugs (p<0.01); and tobacco-frequency of use (p<0.01). The significant associations found in the distinction by age groups show differences in use (at least once) of cocaine and designer drugs, and also with the frequency of tobacco use, with percentages being higher among subjects aged over 30.
Drug use at least once and frequency of tobacco smoking.
| Total | High sexual risk | Low sexual risk | χ2 sexual risk | Age 16–25 | Age 26–29 | Age 30–36 | χ2 age | |
|---|---|---|---|---|---|---|---|---|
| Cannabis | 61.8% (149) | 70.7% (82) | 55.3% (63) | 5.8 (p=0.01) | 60.4% (81) | 61.7% (37) | 66% (31) | 0.44 (p=0.79) |
| Cocaine | 10.4% (25) | 16.4% (19) | 5.3% (6) | 7.3 (p<0.01) | 5.2% (7) | 10% (6) | 25.5% (12) | 15.4 (p<0.01) |
| Designer drugs | 15.8% (38) | 22.6% (26) | 9.6% (11) | 7.09 (p<0.01) | 11.2% (15) | 18.3% (11) | 26.1% (12) | 6.05 (p=0.04) |
| Heroin | 0% | 0% | 0% | 0% | 0% | 0% | ||
| Injected drug | 0% | 0% | 0% | 0% | 0% | 0% | ||
| Tobacco | ||||||||
| Regular | 21.2% (51) | 26.7% (31) | 17.5% (20) | 14.4 (p<0.01) | 18.7% (25) | 23.3% (14) | 25.5% (15) | Fisher's test, p=0.02 |
| Occasional | 5.4% (13) | 7.8% (9) | 3.5% (4) | 4.5% (6) | 3.3% (2) | 10.6% (5) | ||
| Sporadic | 10.4% (25) | 7.8% (9) | 12.3% (14) | 13.4% (18) | 6.7% (4) | 6.4% (3) | ||
| Former smoker | 8.7% (21) | 13.8% (16) | 4.4% (5) | 6.7% (9) | 5% (3) | 19.1% (9) | ||
| Non-smoker | 54.4% (131) | 44% (51) | 62.3% (71) | 56.7% (76) | 61.7% (37) | 38.3% (18) | ||
Both positive and negative conclusions can be drawn from the information the young participants in this study have about HIV transmission routes and protection methods, which was the primary endpoint of the study; 17.8% think that HIV can be transmitted by mosquito bites and 4.6% by sharing public toilets. These results do not in themselves represent an actual risk of infection, but they do indicate a lack of precise knowledge about HIV and how it can be transmitted. We should add, however, that the answers about sexual relations or receiving blood were generally encouraging in terms of knowledge about these transmission routes.
According to previous studies, such as the INE report12 or the report by the Fundación para la Innovación y la Prospectiva de Salud en España (FIPSE) [Foundation for Innovation and Planning for Health in Spain],14 university students aged from 18 to 29 stated that effective measures to prevent HIV included having few partners (41.2% vs 39.8% in this study), choosing partners well (63.6% vs 59.8%), washing after having sex (21.9% vs 12.9%) and the use of spermicides (21.7% vs 11.6%); with these results suggesting that, in general, our sample seemed to have a better perception.
However, there are specific deficiencies in the knowledge expressed by the group of young Spaniards surveyed which may act as risk factors in terms of developing appropriate protective behaviour, such as the affirmative responses in washing after having sex, choosing “good” partners and the use of spermicides. That conclusion is supported by previous studies which associate the lack of adequate knowledge and the practising of risk behaviours by young people.3,15
It should also be noted that the different age groups provided similar responses for both the infection routes and the possible forms of protection, suggesting a stability with this variable.
Examining the secondary endpoint of identifying risk behaviour, it is important to point out that having specified lack of condom use as the main cause of new infections among young people,5,6 the use of condoms still does not constitute a widespread protection factor, as only 40.9% of the subjects admit to always using them. The rates are similar (around 40%) for both men and women, and among age groups. Our figures are similar to the results provided by Hernán et al.,16 who found that only one in three young people used condoms in all their sexual encounters, but considerably lower than those found in the “CONTROL Barometer 2016”,17 where 74% of young people aged 18 to 35 said they always used condoms. These results are remarkable when we compare them with the 98.8% of respondents who stated that the male condom is a very or quite effective form of protection against HIV, and with the 100% who responded that HIV is transmitted through having sex. It could therefore be concluded that knowledge about risk and protection are not in themselves sufficient protection factors to prompt the use of condoms no matter what, in line with the conclusions of previous studies,8–11 which related condom use to other types of variables, such as action planning and other forms of social cognition.
Focusing on another important factor of sexual behaviour, the number of partners, men generally reported having had more sexual partners than women, with 43.8% of men, but only 26.3% of women, having had ten or more different partners.
Moreover, 61% of the surveyed participants did not perceive their sexual relationships as putting them at any risk of infection, which contrasts with the 48.1% of young people identified as having a high-risk sexual profile in our study. This outcome was consistent across the different age groups, despite differences in the percentage of the sample, and most of the subjects identified their sexual risk as between low and non-existent, regardless of which group they belonged to. The conclusion is that there is a generalised problem of underestimation among subjects in terms of how they perceive their risk of exposure to HIV.
The study's third endpoint was to identify associations with the sexual-risk profile, but we found no significant association between sexual-risk profile and the sociodemographic characteristics examined (Table 1). However, such an association has been reported previously, for example by Bermúdez et al.,18 who found significant differences between the sexual behaviour admitted to by adolescents native to Spain and South American adolescents.
In terms of knowledge about HIV, young people with a high-risk profile seem to be better informed than those with low risk. The subjects included in the low-risk profile were more likely to consider that washing after sex, having few partners and using spermicides are very or quite effective methods to protect them from HIV. Young people in the low-risk group also had more misconceptions about transmission, with 22.6% believing that HIV can be transmitted by mosquito bites.
Our figures on knowledge coincide with those found in other studies on young people in Spain19 and Venezuela.20 The fact that young people with more risky sexual behaviour have better knowledge is in line with other studies,3,15,16,21 which suggest that knowledge of infection routes and protection methods is an influential mediator, but absolutely not a determinant protective factor when it comes to sexual behaviour. Our results are also consistent with those reported by other authors, such as DiClemente11 and Pando et al.,22 who showed that adolescents and the homosexual population with better levels of knowledge were the ones with the most risky behaviours.
Again relating the perceived sexual risk to the third endpoint of identifying associations with the sexual-risk profile, both groups tended to identify themselves as having little or no sexual risk, and, although those at high-risk did perceive their behaviour as being riskier (p<0.01), only 13.9% identified themselves as being at high or quite significant risk. That coincides with the conclusions made by other authors8–11 that self-perception of risk is particularly important in terms of protective behaviour and key to reducing risk behaviours, in addition to being a good predictor of condom use.8
With regard to patterns of drug use, except in the case of tobacco smoking, a higher rate was found in high-risk subjects. However, this contrasts with the study by Rodríguez et al.,23 in which no direct associations were found between drug use and risky sexual behaviours. We should point out that in our study the pattern of use did not measure frequency, simply having used the substance at least once in their life. The conclusions cannot therefore be compared directly with other studies. They can only be compared save for the differences. The results are consistent with previous studies,9,15,24 which found behaviours in different areas such as drug use, sexual practices or both to be interrelated, and formed a more general risk profile, and others,25,26 which already considered the introduction of drug use in sexual practices. We would conclude that the use of drugs can be either a risk factor directly related to the infection or simply another example of a personal profile of deficient self-care in which risk behaviours are expressed in different areas of functioning.
One limitation of our study is that the proportion of young people with higher education was greater than that for Spain as a whole, and the study is therefore less representative than we had hoped and it is difficult to generalise the results. The survey we used was based on research into risky behaviours from a general and not integral perspective of sexuality, so the conclusions cannot be used by themselves to establish key points of intervention, only to indicate general aspects.
In conclusion, despite the positive and negative results in terms of knowledge about HIV, the main, and obviously important, difference is the discrepancy between the personal assessment of risk and the actual risk of infection, even though this is not necessarily mediated by the general knowledge expressed by the subjects.
Looking to the future of research on risk factors, we need to develop standardised sexual behaviour assessment tools which specify all the relevant conceptual and relational aspects and spheres of sexual behaviour. This will improve the psychometric characteristics of the results and help us obtain more generalisable conclusions, from which specific prevention campaigns on well-defined risk factors can be designed.
FundingThis work was partially funded by the Fundación para la Investigación y Prevención de Sida (FIPSE) [Foundation for AIDS Research and Prevention in Spain] (FIPSE 24691/07, 3608229/09, FIPSE 240800/09, FIPSE 361910/10), Red Temática de Investigación en Sida (RED RIS) [Thematic Network of Research in AIDS] based at the Instituto de Salud Carlos III (ISCIII) (RD12/0017/0035 and RD12/0017/0037), projected as part of the R+D+I Plan and co-financed by the ISCIII-Sub-directorate General for Assessment and European Regional Development Fund (ERDF). A way to make Europe; Mutua Madrileña 2012/0077; Gilead Fellowship 2013/0071; FIS PI15/00694 (FEDER), CoRISpe (RED RIS RD06/0006/0035 and RD06/0006/0021) RIS-EPICLIN-12/2012. TS funded by the 2014 Research Fellowship Award from the European Society for Paediatric Infectious Diseases (ESPID) and currently by the Spanish Ministry of Innovation and Science (ISCIII, Juan Rodés Contracts). BRS contract funded by ISCIII-Río Hortega [CM 16/0022]. CV currently funded by Madrid Region and ERDF funds (Grants for hiring research assistants and laboratory technicians/Order 2524/2016, of 1 August, BOCM (Boletín Oficial de la Comunidad de Madrid [Official Gazette of the Autonomous Region of Madrid]) No. 188, 8 August 2016).
Conflicts of interestThe authors declare that they have no conflicts of interests.
This study would not have been possible without the collaboration of all healthcare personnel and research professionals who took part in it through the CoRISpe cohort, associated with the RIS network financed by the Instituto de Salud Carlos III through the Red Temática de Investigación Cooperativa en Sida [Thematic Network of Cooperative Research in AIDS].
NeuroCoRISpe project:
María José Mellado, Luis Escosa, Milagros García Hortelano, Talía Sainz (Hospital La Paz, Madrid, Spain)
María Isabel González-Tomé, Pablo Rojo, Daniel Blázquez, Elisa Fernández, Cristina Epalza, Berta Zamora, Cristina García-Navarro, Manuela Martin, Carlos Velo, Ana Martínez de Aragón (Hospital 12 de Octubre, Madrid, Spain)
José Tomás Ramos, Isabel Cuellar (Hospital Clínico San Carlos, Madrid, Spain)
Luis Prieto, Sara Guillén (Hospital de Getafe, Getafe, Spain)
María Luisa Navarro, Jesús Saavedra, Mar Santos, M. Ángeles Muñoz, Beatriz Ruiz, Carolina Fernández McPhee, Santiago Jiménez de Ory, Susana Álvarez (Hospital Gregorio Marañón, Madrid, Spain)
Claudia Fortuny, Ton Noguera (Hospital San Joan de Deu, Barcelona, Spain)
David Moreno, Esmeralda Núñez (Hospital Carlos Haya, Málaga, Spain)
Olaf Neth, Dolores Falcón (Hospital Virgen del Rocío, Seville, Spain).
This section is included in the Madrid CoRISpe cohort:
María José Mellado, Luis Escosa, Milagros García Hortelano, Talía Sainz (Hospital La Paz, Madrid, Spain)
María Isabel González-Tomé, Pablo Rojo, Daniel Blázquez, Elisa Fernández, Cristina Epalza, Berta Zamora, Cristina García-Navarro, Manuela Martin, Carlos Velo, Ana Martínez de Aragón (Hospital 12 de Octubre, Madrid, Spain)
José Tomás Ramos, Isabel Cuellar (Hospital Clínico San Carlos, Madrid, Spain)
Luis Prieto, Sara Guillén (Hospital de Getafe, Getafe, Spain)
María Luisa Navarro, Jesús Saavedra, Mar Santos, M. Ángeles Muñoz, Beatriz Ruiz, Carolina Fernández McPhee, Santiago Jiménez de Ory, Susana Álvarez (Hospital Gregorio Marañón, Madrid, Spain)
Miguel Ángel Roa (Hospital de Móstoles, Móstoles, Spain)
José Beceiro (Hospital Príncipe de Asturias, Alcalá de Henares, Spain)
Jorge Martínez (Hospital Niño Jesús, Madrid, Spain)
Katie Badillo (Hospital de Torrejón, Torrejón de Ardoz, Spain)
Miren Apilanez (Hospital de Donostia, San Sebastián, Spain)
Itziar Pocheville (Hospital de Cruces, Bilbao, Spain)
Elisa Garrote (Hospital de Basurto, Bilbao, Spain)
Elena Colino (Hospital Insular Materno Infantil, Las Palmas de Gran Canaria, Spain)
Jorge Gómez Sirvent (Hospital Virgen de la Candelaria, Santa Cruz de Tenerife, Spain)
Mónica Garzón, Vicente Román (Hospital de Lanzarote, Spain)
Abián Montesdeoca, Mercedes Mateo (Complejo Universitario de Canarias, La Laguna-Tenerife, Spain)
María José Muñoz, Raquel Angulo (Hospital de Poniente, El Ejido, Spain)
Olaf Neth, Lola Falcón (Hospital Virgen del Rocío, Seville, Spain)
Pedro Terol (Hospital Virgen de la Macarena, Seville, Spain)
Juan Luis Santos (Hospital Virgen de las Nieves, Granada, Spain)
David Moreno (Hospital Carlos Haya, Malaga, Spain)
Francisco Lendínez (Hospital de Torrecárdenas, Almería, Spain)
Ana Grande (Complejo Hospitalario Universitario Infanta Cristina, Badajoz, Spain)
Francisco José Romero (Complejo Hospitalario de Cáceres, Cáceres, Spain)
Carlos Pérez (Hospital de Cabueñes, Gijón, Spain)
Miguel Lillo (Hospital de Albacete, Albacete, Spain)
Begoña Losada (Hospital Virgen de la Salud, Toledo, Spain)
Mercedes Herranz (Hospital Virgen del Camino, Pamplona, Spain)
Matilde Bustillo, Carmelo Guerrero (Hospital Miguel Servet, Zaragoza, Spain)
Pilar Collado (Hospital Clínico Lozano Blesa, Zaragoza, Spain)
José Antonio Couceiro (Complejo Hospitalario de Pontevedra, Pontevedra, Spain)
Amparo Pérez, Ana Isabel Piqueras, Rafael Bretón, Inmaculada Segarra (Hospital La Fe, Valencia, Spain)
César Gavilán (Hospital San Juan de Alicante, Alicante, Spain)
Enrique Jareño (Hospital Clínico de Valencia, Valencia, Spain)
Elena Montesinos (Hospital General de Valencia, Valencia, Spain)
Marta Dapena (Hospital de Castellón, Castellón, Spain)
Cristina Álvarez (Hospital Marqués de Valdecilla, Santander, Spain)
Ana Gloria Andrés (Hospital de León, León, Spain)
Víctor Marugán, Carlos Ochoa (Hospital de Zamora, Zamora, Spain)
Santiago Alfayate, Ana Isabel Menasalvas (Hospital Virgen de la Arrixaca, Murcia, Spain)
Elisa de Miguel (Complejo Hospitalario San Millán-San Pedro, Logroño, Spain)
Paediatric HIV BioBank, integrated into the Red Española de Investigación sobre SIDA [Spanish Network for AIDS Research]
Please cite this article as: Velo-Higueras C, Cuéllar-Flores I, Sainz-Costa T, Navarro-Gómez ML, García-Navarro C, Fernández-McPhee C, et al. Jóvenes y VIH. Conocimiento y conductas de riesgo de un grupo residente en España. Enferm Infecc Microbiol Clin. 2019;37:176–182.