La prevención de las lesiones por presión (LPP) adquiridas en el hospital en pacientes críticos sigue siendo un reto clínico importante debido a su alto riesgo de comorbilidad asociada. Se evaluó la eficacia preventiva de los apósitos de silicona en los pacientes ingresados en las unidades de cuidados intensivos y en entornos no relacionados con dichas unidades.
MétodosSe realizó una búsqueda bibliográfica en 3bases de datos electrónicas (MEDLINE, EMBASE, Cochrane Central) desde el inicio hasta diciembre de 2021. Se incluyeron los estudios que evaluaban la eficacia de los apósitos de silicona en la incidencia de LPP en la zona sacra. Las evaluaciones se informaron como ratios de riesgo relativo (RR) con intervalos de confianza al 95% y el análisis se hizo mediante un modelo de efectos aleatorios.
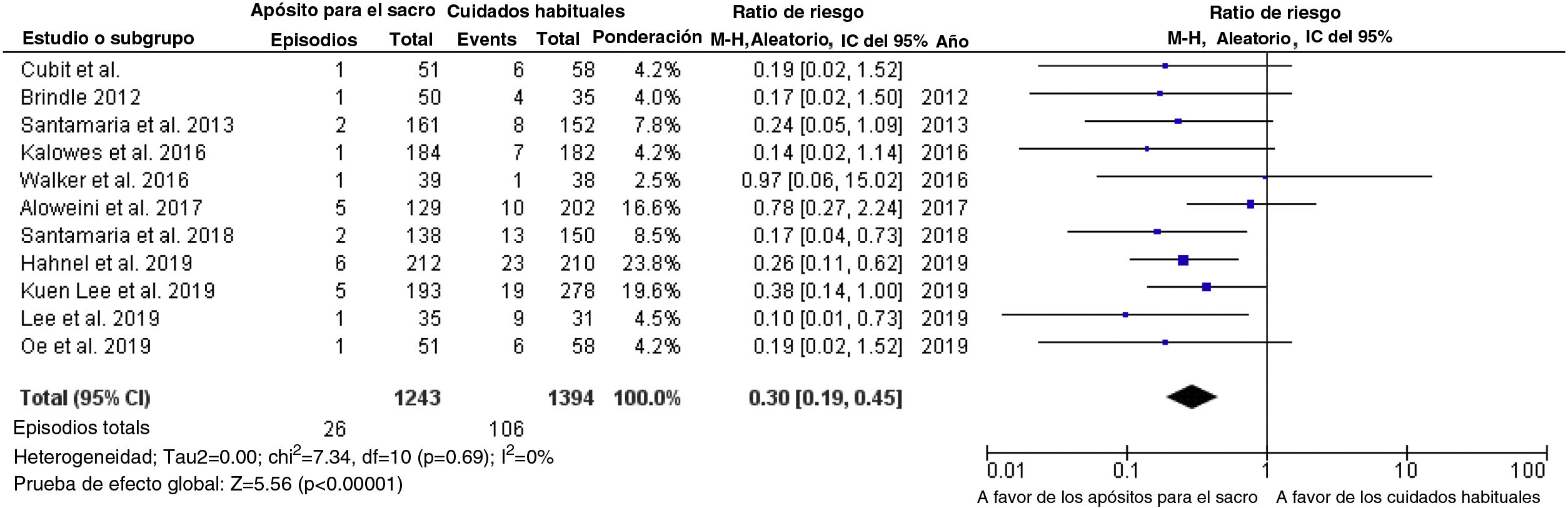
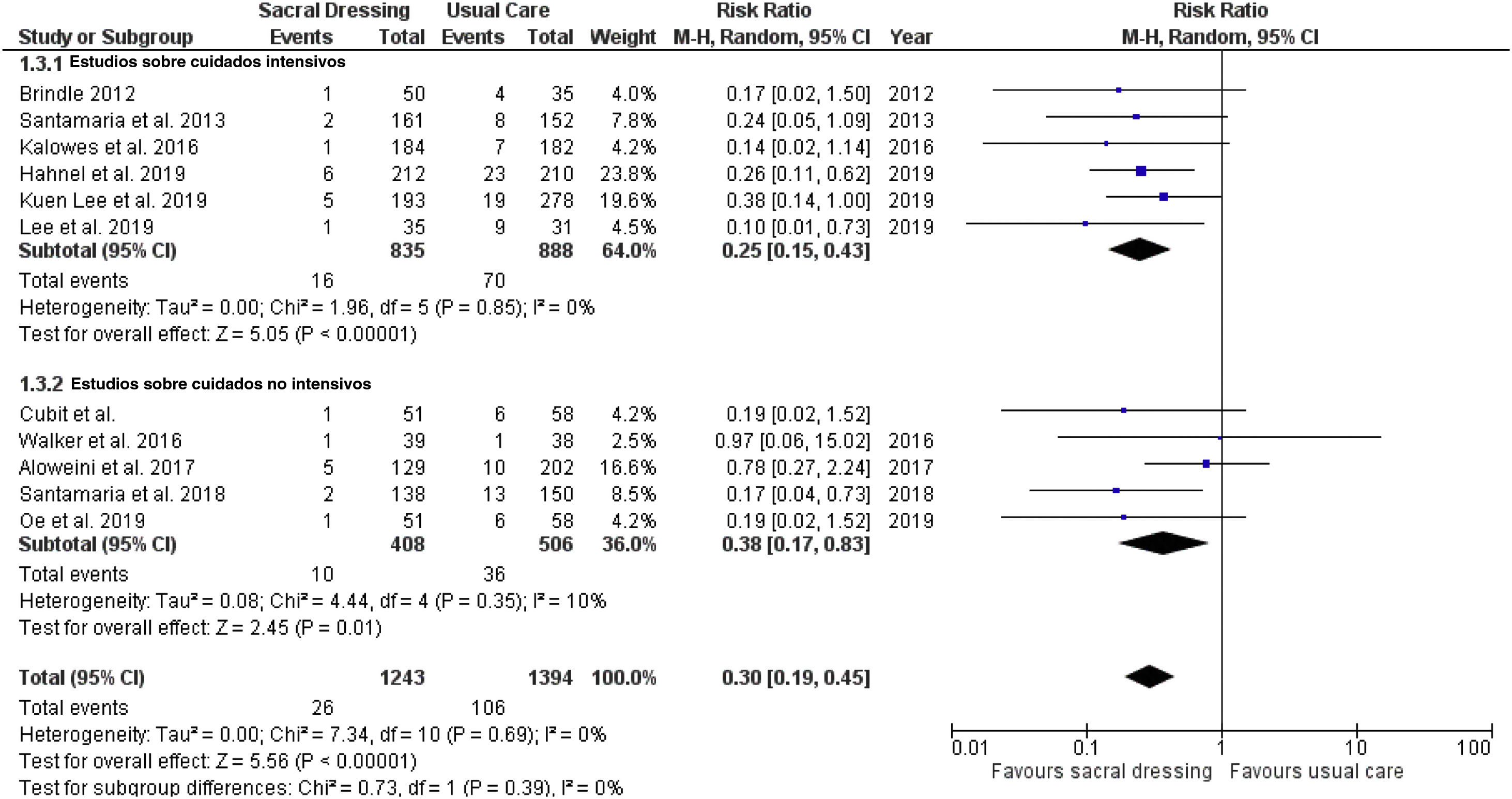
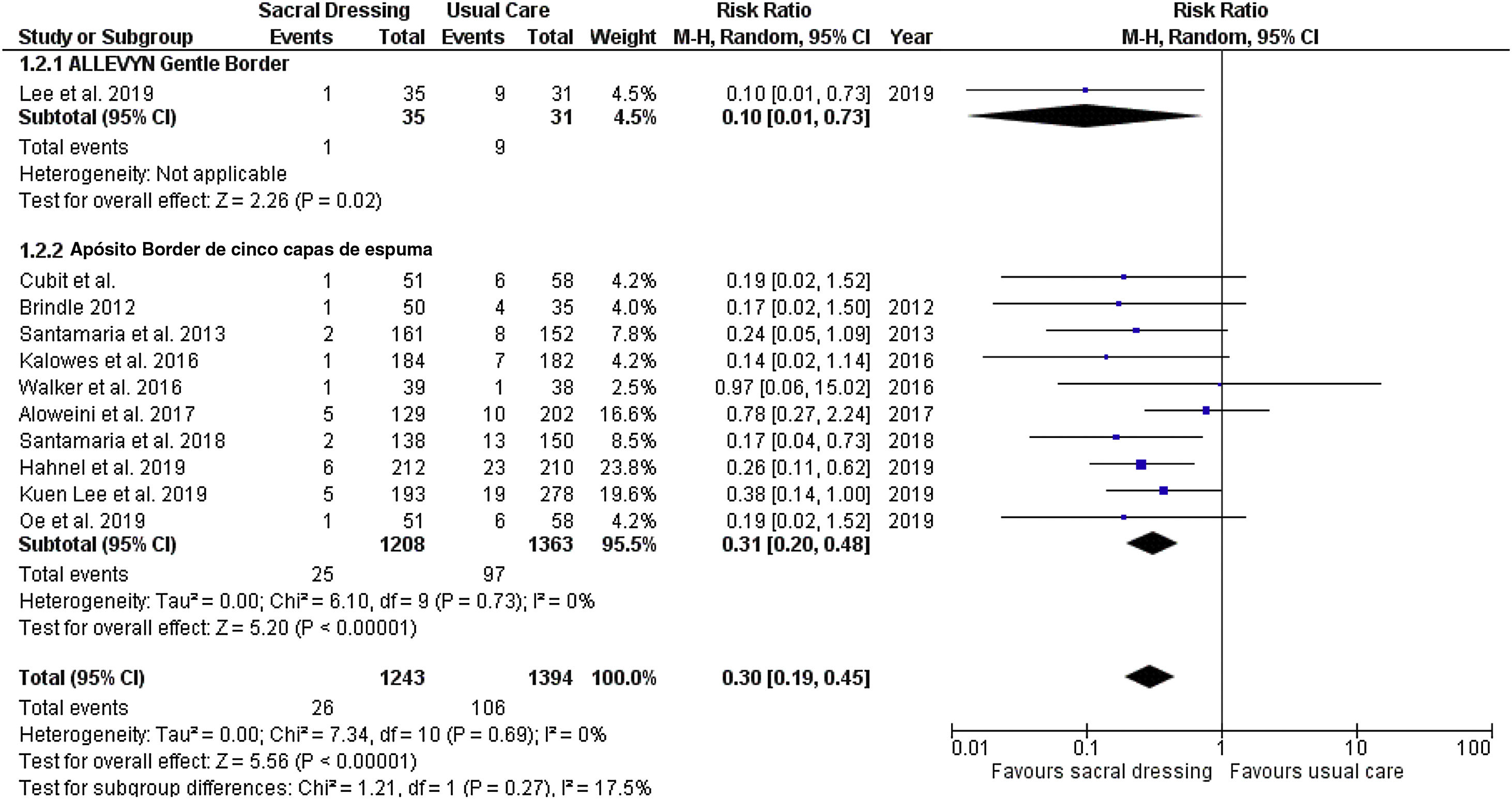
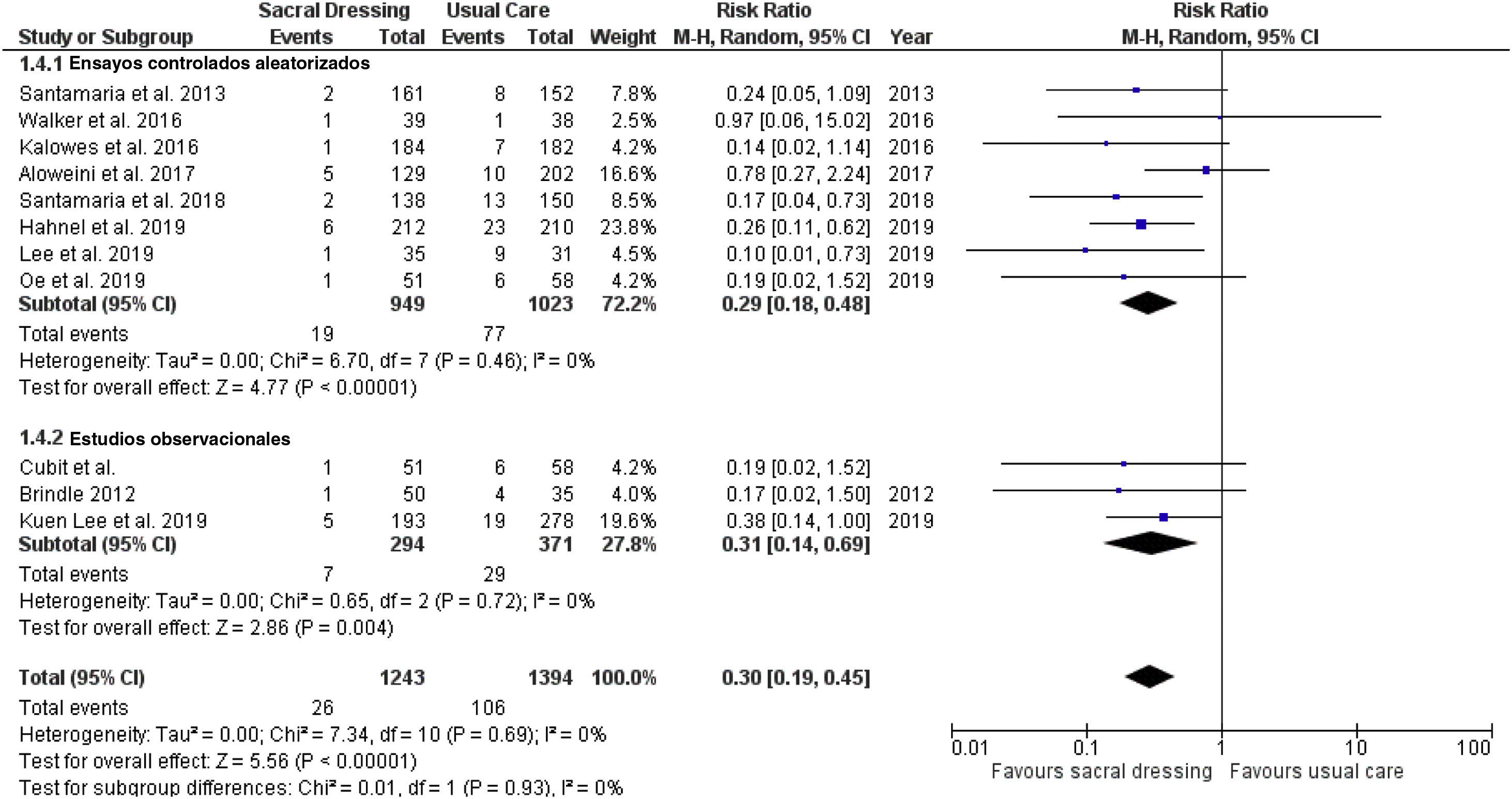
ResultadosDe los 1.056 artículos recuperados en la búsqueda inicial, se incluyeron 11estudios en el análisis final. Los apósitos de silicona redujeron significativamente la incidencia de LPP en comparación con la atención habitual (RR: 0,30; IC 95%: 0,19-0,45; p<0,01). No se encontraron diferencias significativas entre los resultados de los estudios en contextos de cuidados intensivos (RR=0,25; IC 95%: 0,15-0,43; p<0,01) y en contextos de cuidados no intensivos (RR=0,38; IC 95%: 0,17-0,83; p=0,01) (interacción de p: 0,39). Los apósitos de silicona redujeron el riesgo de desarrollar LPP entre los pacientes que utilizaron el apósito de espuma de 5capas Border (Mepilex® Sacrum) (RR: 0,31; IC 95%: 0,20-0,48; p<0,01) y el apósito Allevyn Gentle Border® (RR: 0,10; IC 95%: 0,01-0,73; p=0,02) sin diferencias significativas tras el análisis de subgrupos (interacción de p: 0,27).
ConclusiónEl presente metaanálisis señala que los apósitos de silicona reducen de forma consistente la incidencia de las LPP en entornos de cuidados intensivos y no intensivos, independientemente del tipo de apósito utilizado.
Preventing hospital-acquired pressure injuries (PI) in critically ill patients remains a significant clinical challenge because of its associated high risk for comorbid conditions. We assessed the preventive effectiveness of silicone dressings among patients admitted in intensive care units and non-intensive care units settings.
MethodsA literature search was conducted across 3electronic databases (MEDLINE, EMBASE, Cochrane Central) from inception through December 2021. Studies assessing the effectiveness of silicone dressing on the incidence of PI on the sacral area were included. evaluations were reported as risk ratios (RRs) with 95% confidence interval, and analysis was performed using a random-effects model.
ResultsOf the 1,056 articles retrieved from the initial search, 11studies were included in the final analysis. Silicone dressings significantly reduced the incidence of PI compared to usual care (RR: 0.30, 95%CI: 0.19-0.45, P<0.01). We found no significant difference between results of studies conducted in intensive care settings (RR=0.25, 95%CI: 0.15-0.43, P<0.01) and non-intensive care settings (RR=0.38, 95%CI: 0.17-0.83, P=0.01) (P-interaction: 0.39). Silicone dressings reduced the risk of developing PI among patients using five-layer foam Border dressing (Mepilex® Sacrum) (RR: 0.31, 95%CI: 0.20-0.48, P<0.01), and dressing Allevyn Gentle Border® (RR: 0.10, 95%CI: 0.01-0.73, P=0.02) with no significant difference upon subgroup analysis (P-interaction: 0.27).
ConclusionThe present meta-analysis suggests that silicone dressings consistently reduce the incidence of PI in intensive as well as in non-intensive care settings, regardless of the type of dressing used.