To explore the experiences, emotions and coping skills among emergency medical technicians and emergency nurses after performing out-of-hospital cardiopulmonary resuscitation maneuvers resulting in death.
MethodAn exploratory qualitative research was performed. Seven emergency medical technicians and six emergency nurses were selected by non-probability sampling among emergency medical system workers. The meetings took place up to information saturation, achieved after six individual interviews and a focal group. The meetings were then transcribed and a manual and inductive analysis of the contents performed.
Main resultsAfter a failed resuscitation several short and long-term reactions appear. They can be negatives, such as sadness or uncertainty, or positives, such as the feeling of having done everything possible to save the patient's life. Emotional stress increases when ambulance staff have to talk with the deceased's family or when the patient is a child. The workers do not know of a coping strategy other than talking about their emotions with their colleagues.
ConclusionsDeath after a failed resuscitation can be viewed as a traumatic experience for rescuers. Being in contact with the suffering of others is an emotional, stress-generating factor with direct repercussions on the working and personal lives of emergency staff. Nevertheless, structured coping techniques are not common among those professionals.
Explorar las experiencias, emociones y estrategias de afrontamiento de las enfermeras y técnicos de emergencias extrahospitalarias tras la realización de maniobras de resucitación con resultado de muerte.
MétodoEstudio de análisis de contenido cualitativo. Participaron 7 técnicos en emergencias y 6 enfermeras seleccionados mediante muestreo no probabilístico entre los trabajadores del ámbito de las emergencias sanitarias del País Vasco. Se realizaron reuniones hasta saturación de la información, lográndose tras realizar 6 entrevistas individuales y un grupo focal. Se procedió a la transcripción de las reuniones y se realizó un análisis de contenido de las entrevistas de forma manual e inductiva.
Principales resultadosTras una reanimación fallida afloran diversas reacciones a corto y a largo plazo. Pueden ser negativas, como la tristeza o la incertidumbre, o positivas, como la sensación de certeza con respecto a haber hecho todo lo posible por salvar la vida del paciente. El estrés emocional aumenta a la hora de interactuar con la familia del fallecido o cuando el paciente es un niño, pero los profesionales no contemplan técnicas de afrontamiento más allá de compartir sus emociones con los compañeros de trabajo.
ConclusionesLa muerte tras una reanimación cardiopulmonar fallida puede suponer una experiencia traumática para los reanimadores. Convivir en contacto con el sufrimiento ajeno es un elemento generador de estrés emocional con implicaciones directas sobre la vida profesional y personal de los trabajadores de emergencias. A pesar de ello, las estrategias de afrontamiento estructuradas no son habituales en este colectivo profesional.
More than 80% of people suffering from cardiopulmonary arrest outside of a hospital environment die where they are, despite the cardiopulmonary resuscitation efforts performed by emergency services. Continuous contact with death and the process thereof may present an impactful experience for healthcare professionals resulting from their work in the health emergency system.
What's the effect?The emotional impact seen in healthcare personnel after a failed resuscitation is a variable phenomenon depending on multiple factors. Healthcare professionals lack standardized coping strategies after experiencing a traumatic or stressful situation.
Implications of the studyIt is important not to underestimate the emotional effects experienced by professionals working in the area of emergency health services. Reporting bad news or providing psychological support to the families of the deceased are aspects to be improved.
Every year in the Basque Country, Emergency Services admit approximately 850 patients with cardiorespiratory arrest outside hospital settings, with over 80% of patients passing away at the healthcare facility despite the cardiopulmonary resuscitation (CPR) techniques applied by health professionals.1
Basic life support (BLS) or advanced life support nursing (ALSn) units participate in over 80% of out-of-hospital actions for cardiac arrest recorded in our community. These units generally constitute the first line of health assistance provided on the spot,1 and they take the lead of the intervention until the arrival of medical staff or the termination of the resuscitation maneuvers by indication of the coordinating emergency center. Within the context of urgent out-of-hospital care, there is little time and information available to make decisions to initiate or terminate life support maneuvers, which is a challenge for the health personnel, whose professional expertise, as well as previous values and experiences, are involved. Furthermore, the assistance does not end after terminating the CPR techniques, and it should be further extended to providing information and support to the patients’ family members, a task of great importance which can be difficult, particularly when it is likely that the team of health professionals itself experiences feelings of sadness or when the family's reaction to the sudden loss of their loved one is manifested in the form of denial, anger, incoercible crying or mental shutdown.
Although emergency professionals frequently coexist with death and its process, it is still not an easy event to cope with and can be considered as one of the most shocking experiences related to their field of work.2,3 Working in direct contact with the suffering of others and death is an important stress-generating element that may have direct implications on a worker's professional and personal life. Hence, the purpose of this study is to explore experiences, emotions and coping strategies of nurses and out-of-hospital emergency medical technicians after performing CPR maneuvers resulting in death.
MethodDesignAn exploratory study was carried out through the analysis of qualitative data. The study was approved by the Ethics Committee of the University of the Basque Country.
Scope and subjectsAn intentional sampling was carried out among emergency medical technicians (EMTs) and nurses working at BLS and ALSn units of the emergency ambulance transport network of the Basque Country. The size of the sample was determined progressively throughout the course of the study, until reaching a saturation point. As a prerequisite for their inclusion in this study, the health workers were required to have carried out at least 5 CPR techniques resulting in death over their entire professional career. No volunteer staff was included in the study. One of the researchers served as a contact point for each group of professionals and, given the small size of the sample population and the difficulty to access it, the “snowball” technique was used as a complement to carry out the sampling procedure. All candidates were contacted personally and, after verifying that they met the relevant selection criteria and that they volunteered to participate in the study, they were summoned to be interviewed.
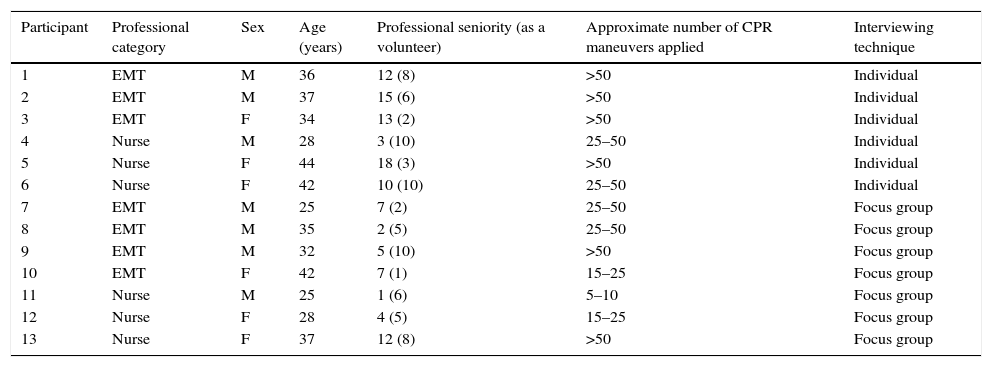
In order to ensure heterogeneity, the study included healthcare professionals of different ages, both genders and varying years of experience, working at different institutions. Finally, our study sample consisted of 7 EMTs and 6 nurses (Table 1).
Profile of the interviewed participants.
| Participant | Professional category | Sex | Age (years) | Professional seniority (as a volunteer) | Approximate number of CPR maneuvers applied | Interviewing technique |
|---|---|---|---|---|---|---|
| 1 | EMT | M | 36 | 12 (8) | >50 | Individual |
| 2 | EMT | M | 37 | 15 (6) | >50 | Individual |
| 3 | EMT | F | 34 | 13 (2) | >50 | Individual |
| 4 | Nurse | M | 28 | 3 (10) | 25–50 | Individual |
| 5 | Nurse | F | 44 | 18 (3) | >50 | Individual |
| 6 | Nurse | F | 42 | 10 (10) | 25–50 | Individual |
| 7 | EMT | M | 25 | 7 (2) | 25–50 | Focus group |
| 8 | EMT | M | 35 | 2 (5) | 25–50 | Focus group |
| 9 | EMT | M | 32 | 5 (10) | >50 | Focus group |
| 10 | EMT | F | 42 | 7 (1) | 15–25 | Focus group |
| 11 | Nurse | M | 25 | 1 (6) | 5–10 | Focus group |
| 12 | Nurse | F | 28 | 4 (5) | 15–25 | Focus group |
| 13 | Nurse | F | 37 | 12 (8) | >50 | Focus group |
M: male; F: female; CPR: cardiopulmonary resuscitation; EMT: emergency medical technician.
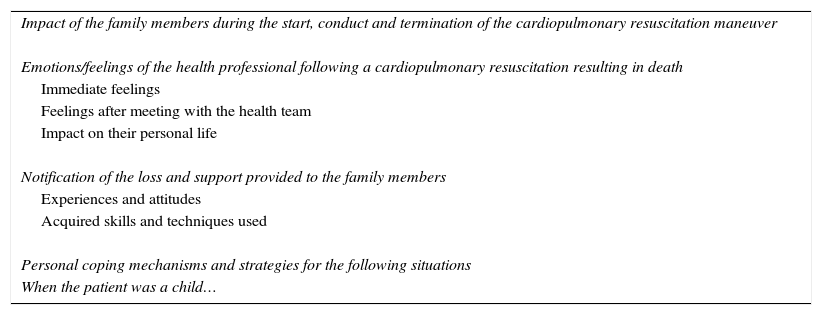
For this research study we used two different data collection techniques: semi-structured individual interviews and focus groups. The study's contents and the matters addressed during the interviews were developed based on the reviewed literature and experts’ opinions (Table 2). The assignment of participants to one or another research technique was based on their availability and preferences. Participants gave their written consent to participate in the study and to be recorded in audio and/or video format.
Matters addressed during the interviews.
| Impact of the family members during the start, conduct and termination of the cardiopulmonary resuscitation maneuver |
| Emotions/feelings of the health professional following a cardiopulmonary resuscitation resulting in death |
| Immediate feelings |
| Feelings after meeting with the health team |
| Impact on their personal life |
| Notification of the loss and support provided to the family members |
| Experiences and attitudes |
| Acquired skills and techniques used |
| Personal coping mechanisms and strategies for the following situations |
| When the patient was a child… |
Data was collected and processed simultaneously in order to guide the sampling procedure. Data saturation was achieved after conducting 6 individual interviews and a focus group. A total of 3 health emergency technicians and 3 nurses were interviewed individually for a total of 11–35min by two of the researchers involved in the study. The focus group was comprised by 4 EMTs and 3 nurses, and it was used to triangulate the information obtained during the individual interviews. The group session lasted 76min and was carried out by two researchers, one acting as a moderator and the other as an observer. None of the researchers involved in the collection of data had a working relationship with any of the participants nor the field of health assistance.
Data analysisAfter completing the literal transcription of all narratives and organizing the relevant observations, a content analysis of the interviews was carried out in a manual and inductive way, consisting of the examination and coding of the data obtained and the categorization of the answers given into different thematic units in order to draw conclusions. Interviews were coded line by line, and categories and subcategories were created by means of the grouping of similar content codes, also taking into account divergent ideas, being an expression of the text's manifest content. The different themes were created by relating meanings, contexts and links between categories, also reflecting the latent content of the data. To ensure the quality of the interpretation and guarantee the reliability of the information obtained, a triangulation between all researchers involved in the interviews was also carried out. Any disagreement was resolved by consensus.
ResultsA total of 3 different themes representing the experiences and emotions of the health professionals after performing CPR maneuvers resulting in death were extracted from the analysis of the contents obtained during the personal interviews and the group discussion. Below we describe the most remarkable results organized according to each theme.
Fluctuating personal impact after failed resuscitation maneuversThe emotions and feelings arising in health professionals after performing a failed CPR maneuver are the result of a combination of sadness for not being able to save a patient's life, and of ease of mind due to the certainty of having made every possible effort. Our participants stated that several negative emotions may arise in members of a health team during the conduct of resuscitation maneuvers, such as feelings of uncertainty, doubt or stress, although they reiterated that these did not affect their performance or decision-making skills when initiating or terminating such maneuvers. However, they did argue that being aware that the maneuvers were performed with the utmost technical rigor is one of the factors that most reassure health professionals when resuscitation techniques do not result in the desired outcome.
Likewise, all participants specified that the feeling of uncertainty or doubt could be alleviated, to some extent, with the support of other health professionals and that, to such effect, the presence of medical staff offers a generalized feeling of professional support.
The immediate emotional responses in the form of sadness or emotional trauma and personal involvement that may arise among emergency health professionals after a failed resuscitation attempt are primarily determined by their relationship with the patient (acquaintances or recurrent patients) or their degree of empathy with the specific situation (events that recall personal experiences) and not expressly by the death itself. Moreover, health professionals point out that the events experienced during their work shift relate to changes in their perception of different aspects of their extra-professional life, such as valuing small daily events that they previously overlooked or that seemed to lack interest for them with greater intensity.
In order to deal with the negative emotions arising from witnessing the death of others or other traumatic events, our interviewees identified different non-systematized strategies arising spontaneously, such as going on walks or meditating, generally on their own. Most participants claimed that they relied upon co-workers to share their impressions and mitigate negative feelings, either during working hours or during their leisure time. Nevertheless, this behavior seems to be confined to relationships between co-workers who have a close trust bond.
In their narratives, participants stated that some companies working in the health transport sector offer psychological care services for their employees, and although this resource was valued positively by the participants, none of them claimed that they had had to make use of them to receive specialized care to treat the adverse emotional effects arising from their professional activity. No structured or customary techniques aimed at reducing the psychological impact (debriefing or defusing) were described.
Participants considered their family setting as an aseptic place of rest and disconnection from their work. In general terms, it did not represent an appropriate environment to share what had happened during their work shift, and participants claimed that they consider that their family should not be aware of their emotions, concerns or dilemmas, as they believe that they may not be understood or that hearing these events may be unpleasant for others. However, when another family member is also a health professional it seems more feasible to talk about such events without almost any restrictions.
Difficulty to communicate with family members in cases of failed resuscitation maneuversThe presence of family members during the conduct of CPR maneuvers was subject to discrepancies among the interviewees. Some participants claimed that their presence is positive for the family members when it comes to start dealing with the loss of their loved one, and that this is how most professionals prove that they made every possible effort to save the life of the patient. On the other hand, other participants claimed that they consider the presence of family members to be an inconvenience and that it can have a negative impact on the conduct of the maneuvers, increasing the rescuers’ stress or hindering their performance.
Although this is not common, when in the absence of a doctor, these professionals must notify the patients’ death to their family members, and all interviewees coincided in recognizing such moment as one of the most uncomfortable and critical ones of their field of work.
Another matter that tended to be repeated among the group of professionals interviewed was the need for further training in order to acquire skills to communicate such bad news. Only a few participants felt that they were prepared for such task, and most claimed that they resorted to using resources developed with experience, given that adapting the notification of the loss of a family member to each situation is difficult for them, even when the relatives themselves have witnessed the unsuccessful resuscitation attempts. The characteristics that determine how the loss is notified vary greatly based on different factors, among which the initial reaction of the family members to the news stands out. Moreover, participants considered that their behavior can have a strong impact on their ability to reassure the family members or help channel their pain by making use of their most humane side and the good use of language. All personnel interviewed admitted that the overall view is that the notification of losses is not done properly in practice, and that health workers often refuse to inform family members of the loss, delaying this task until the arrival of a doctor who will shoulder such responsibility.
Greater personal impact when the deceased is a child or a young individualParticipants pointed out that providing care for cardiac arrest in young or pediatric patients is related to certain peculiarities and differences, both in terms of the immediate course of action and of the subsequent repercussion on their mood when the resuscitation attempts have failed. In general, participants admitted that their degree of empathy, and the emotions and sensations following the cessation of resuscitation maneuvers, are more intense than those experienced with adult patients. In this sense, it is harder for these professionals to assume the failure, and it entails an exaggerated sense of responsibility that leads them more often to initiate resuscitation maneuvers or delay their termination in cases of certain futility.
All participants stated that dealing with the family members of a pediatric patient is very difficult and extremely delicate, this being the reason why they tend to avoid notifying such loss, a task which, in any case, they believe should be carried out by medical staff.
DiscussionOur results suggest that professional contact with death results in emotional reactions of varying magnitude depending on the circumstances that accompanied the event. Thus, the patient's age, the staffs’ relationship with the patient's family members or with co-workers, or the health professionals’ past experiences, among others, represent conditioning factors of the characteristics of the emotions experienced after an unsuccessful cardiopulmonary resuscitation maneuver.
As in the case of previous research carried out within the field of pre-hospital emergencies,4 this study also makes reference to feelings of impotence, sadness or stress arising from events taking place during the participants’ work shift. When the health professional is exposed to tense, conflictive or traumatic situations, a reaction of distress or emotional trauma may arise, with early intervention (with techniques such as debriefing or defusing, among others) seeming to be an effective measure to mitigate their effects5 or to build personal resilience.6 However, our interviewees did not report knowing or participating in such sort of sessions, with co-workers being their main source of emotional support whenever negative feelings arise from experiencing a death. This differs from the statements of paramedics working at emergency departments of New York, who, despite agreeing that talking with co-workers is the main coping strategy used, also use the mental health care services provided by companies in 75% of cases.7 Furthermore, not even the workers’ family setting seems to be a suitable place to share the difficult events that take place during their provision of health care services, as, given its characteristics, this career in itself is considered by some authors as a limiting factor to build an adequate family atmosphere.8
Nevertheless, the health care professionals’ relationship with the patients’ family members is most likely one of the aspects involving the most doubts and uncertainties among interviewees. In fact, previous local studies have described a significant prevalence of conflicts between emergency staff and patients or their family members, resulting in increased feelings of professional exhaustion.9,10
As in the case of other studies,11,12 the presence of family members during the conduct of resuscitation maneuvers is a topic of discussion, although there is evidence that this fact is associated with beneficial psychological effects for the family members and that it does not interfere with the stress or performance of the health professionals involved.13 In agreement with other authors,14,15 this study also brings to light the fact that emergency health professionals are aware that their work also extends to taking care of the family after an unsuccessful resuscitation maneuver, despite the fact that they may feel uncomfortable or under-supported when offering explanations, especially when the deceased is a child. This may occasionally translate into avoidance maneuvers, and also in an unanimous demand for greater training on the proper techniques to communicate the bad news and to care for the needs of the family members.12,16
The limitations inherent to the qualitative methodology used in this study, along with the small size of the sample used and the regional context in which it was carried out, entail that the extrapolation of the results obtained in our study to all clinical professionals must be done with caution, although they seem to contribute valid information to the knowledge of key aspects in the emotional management of CPR resulting in death.
Furthermore, despite the interviewers’ efforts to ensure asepsis and fluidify the participants’ expression of emotions, some members of the focus group knew each other, owing to the moderate dimensions of the autonomic emergency service and the high personnel turnover rate among companies and bases, which may have restrained the pooling of certain opinions among the interviewees.
Finally, we find it striking that, despite the youth of the interviewees, the vast majority had great experience in the care of out-of-hospital cardiac arrests. This fact may owe to the high burden of care to which the emergency medical teams of our region are subject to, and it has not allowed us to thoroughly explore the specific case of junior professionals. This limitation could be subject to further research, as it has been proven that professional seniority within the health field is associated with stronger feelings of emotional exhaustion and depersonalization.17
ConclusionsBased on the comments made by the emergency professionals interviewed, it seems reasonable to conclude that working in the field of health emergencies is an activity associated with a significant impact on the workers’ emotions and personal life. In certain situations, death following an unsuccessful resuscitation maneuver may entail a traumatic experience for the rescuers. Thus, in general, negative emotional reactions are not associated with the death process itself, but rather with the professionals’ degree of empathy or the circumstances surrounding the death, such as dealing with the patients’ family members or the deceased being a young person or an acquaintance. In this respect, co-workers, and not family members, are the main source of comfort, as there are no structured psychological coping strategies available in this group of professionals.
The act of notifying bad news and providing psychological support to the family members of the deceased is defined by health professionals as one of the most critical, uncomfortable, and noticeably improvable, moments of their career; hence, there is a generalized perception of a need for further training in these skills. The presence of a doctor in the medical team results in feelings of a release of responsibilities and safety when ending the resuscitation maneuvers and offering information to the patients’ family members.
Ethical responsibilitiesProtection of people and animalsThe authors declare that no human or animal experiments were carried out for this research.
Confidentiality of dataThe authors declare that they followed the protocols established by their work center regarding the publication of patient data.
Right to privacy and informed consentThe authors obtained the informed consent of all patients and/or subjects referred to in this study. This document is currently in the possession of the corresponding author.
FundingThis research study received funding from the Research Commission of the Integrated Health Organization of Bilbao-Basurto (Osakidetza).
Conflict of interestThe authors declare no conflict of interest.
Please cite this article as: Fernández-Aedo I, Pérez-Urdiales I, Unanue-Arza S, García-Azpiazu Z, Ballesteros-Peña S. Estudio cualitativo sobre las experiencias y emociones de los técnicos y enfermeras de emergencias extrahospitalarias tras la realización de maniobras de reanimación cardiopulmonar con resultado de muerte. Enferm Intensiva. 2017;28:57–63.