Main aim: to discover the Spanish intensive care units (ICU) that assess and record pain levels, sedation/agitation, delirium and the use of physical restraint (PR) as standard practice.
MethodAn observational, descriptive, cross-sectional, prospective and multicentre study using an ad hoc survey with online access that consisted of 2 blocks. Block I: with questions on the unit’s characteristics and routine practice; Block II: aspects of direct care and direct assessments of patients admitted to participating units.
ResultsOne hundred and fifty-eight units and 1574 patients participated. The pain of communicative patients (CP) was assessed and recorded as standard in 109 units (69%), the pain of non-communicative patients (NCP) in 84 (53%), sedation/agitation in 111 (70%), and delirium in 39 units (25%). Validated scales were used to assess the pain of CP in 139 units (88%), of NCP in 102 (65%), sedation/agitation in 145 (92%), delirium in 53 units (34%). In 33 units (21%) pain, sedation/agitation and delirium of PC and NPC was assessed, and in 8 of these units there was a specific PR protocol and register. Among the patients who could be assessed, an absence of pain was reported in 57%, moderate pain in 27%; 48% were calm and collaborative, and 10% agitated; 21% had PR, and 12.6% of the patients had delirium.
ConclusionsThe assessment of pain, sedation and delirium is demonstrated, and low percentages of agitation and delirium achieved. We observed a high percentage of patients with pain, and moderate use of PC. We should generalise the use of protocols to assess, prevent and treat pain and delirium by appropriately managing analgesia, sedation, and individual and well-considered use of PC
Objetivo principal: conocer qué unidades de cuidados intensivos (UCI) españolas valoran y registran, de forma normalizada, niveles de dolor, sedación/agitación, delirio y uso de contenciones mecánicas (CM). Objetivos secundarios: determinar utilización de herramientas validadas de valoración y explorar niveles de dolor y sedación/agitación de los pacientes, prevalencia de deliro y uso de CM.
MétodoEstudio observacional, descriptivo, transversal, prospectivo y multicéntrico mediante una encuesta ad hoc con acceso on line, de 2 bloques. Bloque I: enfocado a preguntas sobre características de las unidades y práctica habitual; Bloque II: aspectos de asistencia directa y evaluaciones directas de pacientes ingresados en unidades participantes.
ResultadosParticiparon 158 unidades y 1574 pacientes. La valoración normalizada y registro del dolor de pacientes comunicativos (PC) se realizaba en 109 unidades (69%), dolor de pacientes no comunicativos (PNC) en 84 (53%), sedación/agitación en 111 (70%), delirio en 39 unidades (25%). Registrado uso de CM en 39 unidades (25%). Se utilizaban escalas validadas para valorar dolor en PC en 139 unidades (88%), en PNC en 102 (65%), sedación/agitación en 145 (92%), delirio en 53 unidades (34%). En 33 unidades (21%) se valoraba dolor a PC y PNC, sedación/agitación y delirio y en 8 de estas unidades existía protocolo específico de CM y registro. Entre aquellos pacientes que pudieron ser evaluados, se reportó ausencia de dolor en 57%, dolor moderado 27%; tranquilos y colaboradores 48% y 10% agitados; tenían CM 21% y delirio el 12.6% de los pacientes.
ConclusionesLa valoración del dolor, sedación y delirio está acreditada, obteniéndose bajos porcentajes de pacientes con agitación y delirio. Observamos elevado porcentaje de pacientes con dolor y moderado uso de la CM. Debemos generalizar el uso de protocolos para valorar, prevenir y tratar dolor y delirio mediante un adecuado manejo de la analgesia, sedación y un uso individual y reflexivo de las CM.
Clinical practice guidelines recommend systematic assessment of pain, sedation/agitation and delirium of patients admitted to intensive care units (ICU), and the rational use of physical restraint. This study determines the regular practice in Spanish ICUs, covering the existence of protocols and assessment of pain and agitation levels, together with the prevalence of physical restraint and delirium.
Study implicationsThis study is a starting point. It offers an opportunity to improve critical care for the patient and it reflects the protocols, results and/or strategies of all participating units, as a reflection on care practice with regards to the assessment and management of pain, sedation and the tranquillity/agitation of the patient in the intensive care unit. On sharing this information each unit may set real, possible objectives, adapted to each care context.
Most procedures performed in intensive care unit (ICU) patients are associated with pain.1 This acute pain triggers an inflammatory response to stress which may affect the patient’s evolution. Several studies have shown that the use of strategies against pain, prior to other sedation strategies may reduce mechanical ventilation time and the stay in the ICU.2–4 The latest published clinical practice guidelines2,5,6 recommend the application of sedation strategies based on analgesia and the administration of minimal doses of sedatives to achieve the desired sedation objective, prioritizing superficial or conscious sedation, provided it is possible.7–9 Inappropriately treated pain is the cause of anxiety or agitation.9 A major proportion of patients in the ICU - estimated to be between 24% and 80% in several series - present a moderate to severe anxiety-agitation level.10 Also, fluctuations in sedation levels may lead to the development of delirium, and this risk may be reduced by maintaining a stable sedation level or by the absence of sedación.11
Another of the factors which may contribute to agitation and delirium is the use of physical restraint. From an ethical viewpoint, we find ourselves confronting principles of non malficence and beneficence in the use of physical restraint, trying to keep a safe environment for the patient with its use and the principle of autonomy, since physical restraint endangers the freedom and dignity of the patient. The use of strategies on pain, agitation/sedation and delirium strategies, which may affect the patient’s well-being could be a powerful tool to minimize the use of physical restraint in the ICU, as shortcomings have been detected in this aspect in the units, with frequent use of these restraints.12
As a result of all of the above, both pain and the level of sedation must be monitored systematically to assess the administration of analgesics and/or sedatives.
As far as we are aware, no common clinical practice assessment has been published in Spanish units, except data from 12 units included in a European survey, where it was stated that in Spain and Portugal (from 5 units involved) sedation scales are used in 65% of the units.13
From the Workgroup on Analgesia, Sedation, Restraints and Delirium (GT-ASCyD for its initials in Spanish) of the Spanish Society of Intensive Care and Coronary Unit Nurses (SEEIUC for its initials in Spanish), we are covering the need for a national level assessment to be made because we are aware of the importance of a good pain and anxiety assessment for our patients and the essential quality it could have in determining regular practice in Spanish ICUs.
The main aim of this study was to determine which units assessed and recorded as standard practice (according to a written regulation or protocol) levels of pain, sedation/agitation, delirium and physical restraint. Secondary aims were to determine the use of validated assessment tools and explore patient’s levels of pain, sedation and agitation together with the prevalence of delirium and physical restraint.
MethodAn observational, descriptive, cross-sectional, prospective and multicentre study was conducted to determine standard (audit) practice on existing protocols in critical care units and assessment of pain, sedation, delirium and the use of physical restraint.
Direct assessment was then made of the level of pain, sedation/agitation and the presence of delirium in all adult patients who were in the participating units at the time of the cut-off point and who had been in the unit for a minimum of 24 h.
ProcedureIn order to obtain the greatest representation of Spanish ICUs, a network of research nurses was created with coordinators in each autonomous community. The function of the coordinators was to contact, recruit critical care adult patient units within their community. Each coordinator, contacted the centres (both public, private), creating their network of nurses in the units who stated their willingness to participate, who obtained authorization from their clinical research ethnics committee. Each unit was then requested to provide contact details of a nurse who would be, in charge of project participation.
Once the national network of participating nurses was established, each nurse was given a pin number and password to get into the platform created for data processing. Each unit was coded with the variable “unit code”, automatically created by the system. The “unit code” was only known by the project nurse coordinator and the collaborating nurse of each unit. The community coordinator nurse only knew the codes of the units which they coordinated.
The platform offered access to all the documents (methodology, timeline, recommended assessment tools, tutorial of platform browsing) and a link to tutorial videos where explanations were given of how to apply the tools validated into Spanish and recommended by the GT-ASCyD-SEEIUC for patient assessment.
Data collectionThe tool used was an ad hoc survey with online access, on the SEEIUC server, which consisted of two blocks.
In block 1, the person was asked about the characteristics of the units, nurse to patient ratio, the existence of protocols and standard practice for the control of pain, sedation/agitation, delirium and the use of physical restraint in the unit.
In block 2, the person was asked questions about direct care of the patients, recording the use of tools (for assessment of analgesia, sedation and delirium) and the direct assessment of the level of pain, sedation/agitation of patients, together with the presence of delirium and physical restraint.
The timeline included details of data collection dates, both in the first and second block. After completion, a follow-up of responses and verification of data was made through electronic mail or telephone calls between the project coordinator and the collaborating nurse of each unit, to filter out possible errors in the data introduced.
Assessment of the patients includedData collection was made using direct observation and in the same period in all participating units. These data were introduced into the platform using a “patient code” automatically created by the system.
To assess pain in communicative patients the visual analogue scale (VAS) was recommended and for non-communicative patients, the scale of the behaviour indicators of pain (ESCID for its initials in Spanish)14 was used. For assessment of the level of sedation/agitation the Richmond Agitation Sedation Scale (RASS),15 was recommended and for delirium, the Confusion Assessment Method for the Intensive Care Unit (CAM-ICU).16
Data on the use of tools to assess pain, sedation/agitation and delirium, and usage records of physical restraint were retrospectively collected on the nursing records of the patients assessed, the day after their assessment.
Statistical analysisFirstly, a descriptive analysis of the general characteristics of the participating units was made and of the study population, presenting the data with means and standard deviations (SD) or medians and interquartile ranges (IQE), as appropriate. The comparison of groups was performed with the Student’s T-test for quantitative variables or non parametric tests, as appropriate and the Fisher or Chi square test for qualitative variables. Data were analysed with the IBM SPSS Statistics 21.0 for Windows (SPSS Inc., Chicago IL, U.S.A.) software.
Ethical considerationsRecommendations from the 1964 Declaration of Helsinki and the 1997 Agreement of Oviedo were followed and confidentiality of information and anonymity of participants was guaranteed, as regulated by Organic Law 15/1999, on protection of personal, and Law 41/2002, on patient autonomy.
The project was approved by the research ethics committee (REC) of the study coordinator centre in Madrid and presented to the REC of each autonomous community. As this was an audit (review of clinical practice) and aggregated information was to be collected, the research team and RECs of the centres did not consider it necessary to request the informed consent of each patient in the unit. Authorisation was requested from each head of medical service and each nursing supervisor of the units involved.
ResultsThe creation of the collaborating nurse network was set up between May 2017 and February 2018. Block 1 questions were completed between 12th and 18th February 2018 and block 2 questions, with direct assessment of pain, sedation/agitation and delirium of the patients, between 19th and 23rd February 2018.
Participating unitsOne hundred and fifty eight units from 103 hospitals in the 17 autonomous communities in Spain took part. There was no representation from the autonomous cities of Ceuta and Melilla.
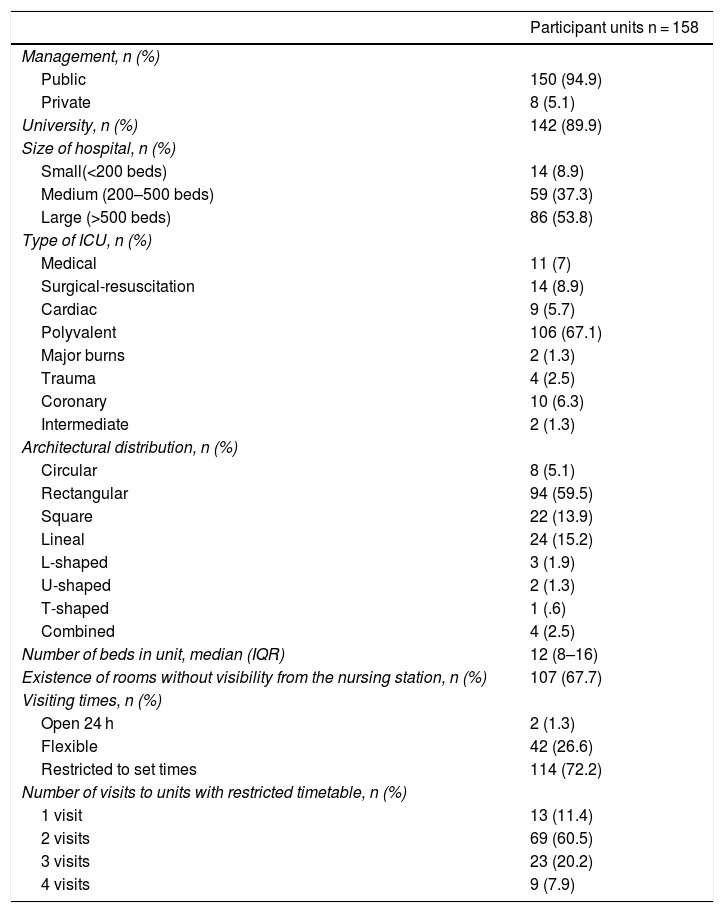
The majority of units were located in public and university hospitals with over 500 beds. 67.1% were multi-purpose units, 59.5% were rectangular in distribution and 67.7% had beds without visibility from the nursing station. The 158 units included 2,061 beds, with a median of 12 beds per unit IQR 8-16) (Table 1).
Characteristics of participating units.
| Participant units n = 158 | |
|---|---|
| Management, n (%) | |
| Public | 150 (94.9) |
| Private | 8 (5.1) |
| University, n (%) | 142 (89.9) |
| Size of hospital, n (%) | |
| Small(<200 beds) | 14 (8.9) |
| Medium (200–500 beds) | 59 (37.3) |
| Large (>500 beds) | 86 (53.8) |
| Type of ICU, n (%) | |
| Medical | 11 (7) |
| Surgical-resuscitation | 14 (8.9) |
| Cardiac | 9 (5.7) |
| Polyvalent | 106 (67.1) |
| Major burns | 2 (1.3) |
| Trauma | 4 (2.5) |
| Coronary | 10 (6.3) |
| Intermediate | 2 (1.3) |
| Architectural distribution, n (%) | |
| Circular | 8 (5.1) |
| Rectangular | 94 (59.5) |
| Square | 22 (13.9) |
| Lineal | 24 (15.2) |
| L-shaped | 3 (1.9) |
| U-shaped | 2 (1.3) |
| T-shaped | 1 (.6) |
| Combined | 4 (2.5) |
| Number of beds in unit, median (IQR) | 12 (8–16) |
| Existence of rooms without visibility from the nursing station, n (%) | 107 (67.7) |
| Visiting times, n (%) | |
| Open 24 h | 2 (1.3) |
| Flexible | 42 (26.6) |
| Restricted to set times | 114 (72.2) |
| Number of visits to units with restricted timetable, n (%) | |
| 1 visit | 13 (11.4) |
| 2 visits | 69 (60.5) |
| 3 visits | 23 (20.2) |
| 4 visits | 9 (7.9) |
IQR: interquartile range.
72.2% of units had restricted visiting hours. In these units the most usual number of visits was twice a day (60.5%), with a median of visiting time permitted of 2 h per day (IQR 1.3-4) (Table 1).
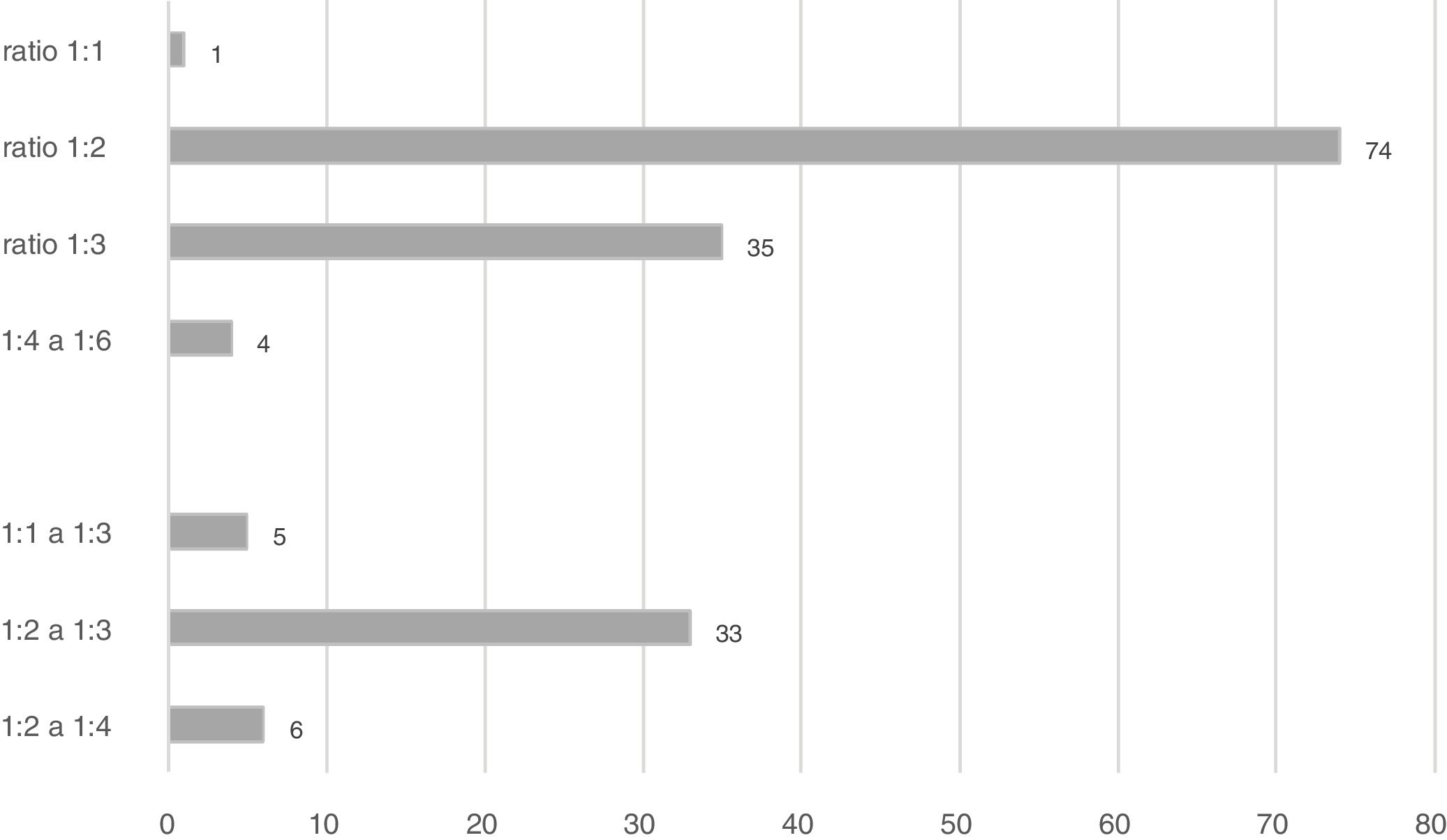
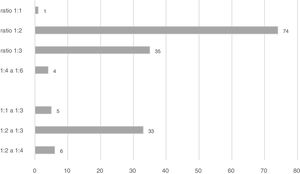
The nurse-patient ratio was highly diverse with the most frequent being 1:2 (74 units [46.8%]). In 44 there was a great variability, influenced by the shifts (day vs. night) or by holidays (Fig.1).
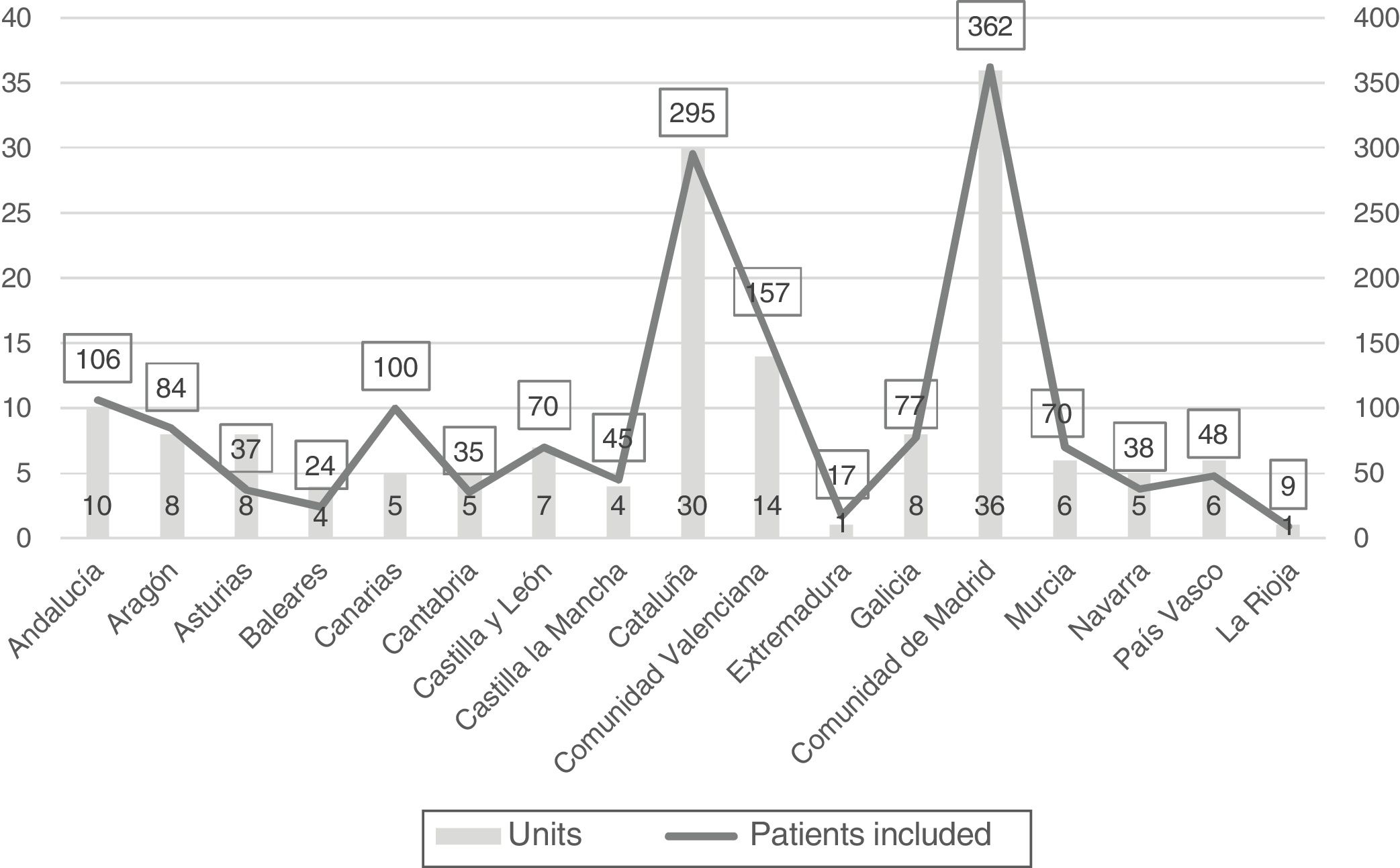
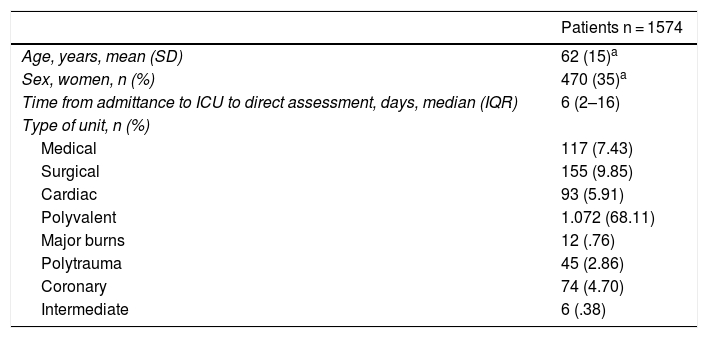
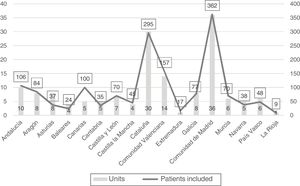
Patients includedThe collaborating units and the patients included in each community are contained in Fig. 2. There were 1,698 patients in the 158 units on the day of observation occupation rate of 82.4%. The patients who met with the inclusion criteria and were assessed and observed by the collaborating researchers were 1,574 92.7% of admitted patients). The majority of patients assessed (68.1%) were admitted into polyvalent units (Table 2).
Patients included in the study.
| Patients n = 1574 | |
|---|---|
| Age, years, mean (SD) | 62 (15)a |
| Sex, women, n (%) | 470 (35)a |
| Time from admittance to ICU to direct assessment, days, median (IQR) | 6 (2–16) |
| Type of unit, n (%) | |
| Medical | 117 (7.43) |
| Surgical | 155 (9.85) |
| Cardiac | 93 (5.91) |
| Polyvalent | 1.072 (68.11) |
| Major burns | 12 (.76) |
| Polytrauma | 45 (2.86) |
| Coronary | 74 (4.70) |
| Intermediate | 6 (.38) |
SD, standard deviation; IQR, interquartile range.
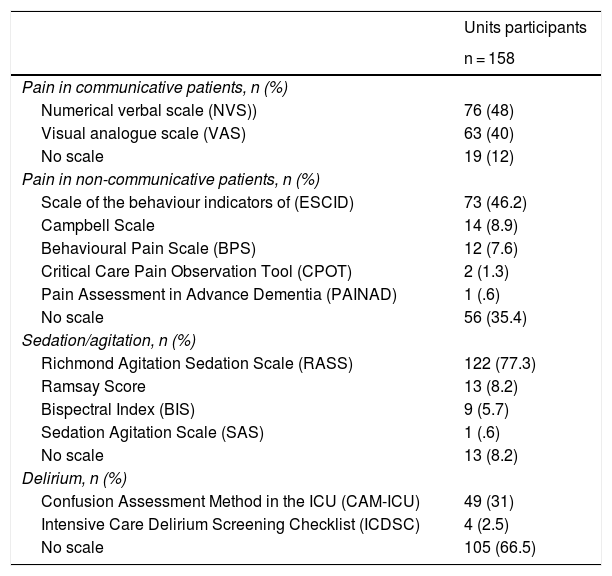
Out of the 158 units, 19 (12%) did not use scales to assess pain in communicative patients and in 56 (35.4%) pain was not assessed in non communicative patients (Table 3).
Use of assessment tools in the units.
| Units participants | |
|---|---|
| n = 158 | |
| Pain in communicative patients, n (%) | |
| Numerical verbal scale (NVS)) | 76 (48) |
| Visual analogue scale (VAS) | 63 (40) |
| No scale | 19 (12) |
| Pain in non-communicative patients, n (%) | |
| Scale of the behaviour indicators of (ESCID) | 73 (46.2) |
| Campbell Scale | 14 (8.9) |
| Behavioural Pain Scale (BPS) | 12 (7.6) |
| Critical Care Pain Observation Tool (CPOT) | 2 (1.3) |
| Pain Assessment in Advance Dementia (PAINAD) | 1 (.6) |
| No scale | 56 (35.4) |
| Sedation/agitation, n (%) | |
| Richmond Agitation Sedation Scale (RASS) | 122 (77.3) |
| Ramsay Score | 13 (8.2) |
| Bispectral Index (BIS) | 9 (5.7) |
| Sedation Agitation Scale (SAS) | 1 (.6) |
| No scale | 13 (8.2) |
| Delirium, n (%) | |
| Confusion Assessment Method in the ICU (CAM-ICU) | 49 (31) |
| Intensive Care Delirium Screening Checklist (ICDSC) | 4 (2.5) |
| No scale | 105 (66.5) |
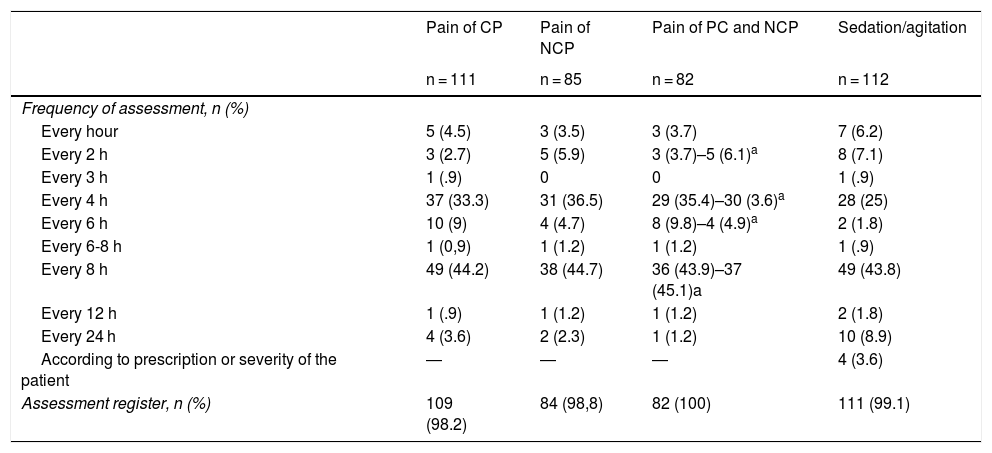
Standard assessment of communicative patients was made in 111 units (70.2%). Out of these, 46 (41.4%) stated they assessed pain every 4 h or less, respecting night sleep and in 60 (54%) every 6–8 h. Standard assessment of non-communicative patients was made in 85 units (53.8%). In 39 of these units, (45.%) pain was assessed every 4 h or less and in 43 (50.6%) every 6–8 h. Assessments were recorded in 98.2% of those which assessed pain in communicative patients in a standardised manner and in 98.8% of those assessed in non-communicative patients (Table 4).
Units which assess pain in a standardised manner and sedation/agitation.
| Pain of CP | Pain of NCP | Pain of PC and NCP | Sedation/agitation | |
|---|---|---|---|---|
| n = 111 | n = 85 | n = 82 | n = 112 | |
| Frequency of assessment, n (%) | ||||
| Every hour | 5 (4.5) | 3 (3.5) | 3 (3.7) | 7 (6.2) |
| Every 2 h | 3 (2.7) | 5 (5.9) | 3 (3.7)–5 (6.1)a | 8 (7.1) |
| Every 3 h | 1 (.9) | 0 | 0 | 1 (.9) |
| Every 4 h | 37 (33.3) | 31 (36.5) | 29 (35.4)–30 (3.6)a | 28 (25) |
| Every 6 h | 10 (9) | 4 (4.7) | 8 (9.8)–4 (4.9)a | 2 (1.8) |
| Every 6-8 h | 1 (0,9) | 1 (1.2) | 1 (1.2) | 1 (.9) |
| Every 8 h | 49 (44.2) | 38 (44.7) | 36 (43.9)–37 (45.1)a | 49 (43.8) |
| Every 12 h | 1 (.9) | 1 (1.2) | 1 (1.2) | 2 (1.8) |
| Every 24 h | 4 (3.6) | 2 (2.3) | 1 (1.2) | 10 (8.9) |
| According to prescription or severity of the patient | ― | ― | ― | 4 (3.6) |
| Assessment register, n (%) | 109 (98.2) | 84 (98,8) | 82 (100) | 111 (99.1) |
CP, communicative patients; NCP, Non-communicative patients.
In 82 units, pain was assessed in both communicative and non-communicative patients. The frequency of assessment in these units was different if the patient was able to communicate or not, and carried out every 4 h or less in at least 35 units (42.7%) and every 6–8 h in at least 42 (51.2%) (Table 4).
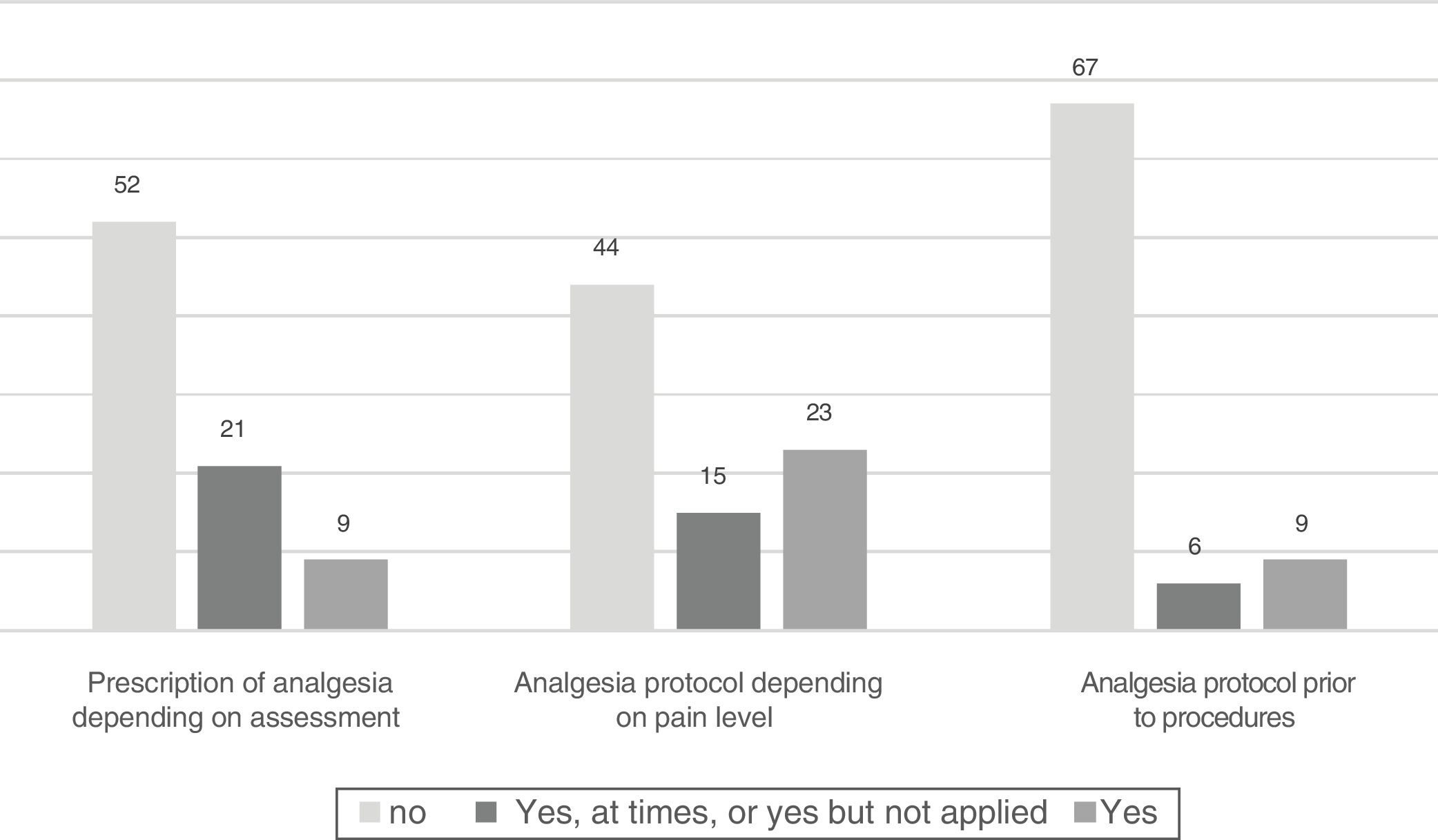
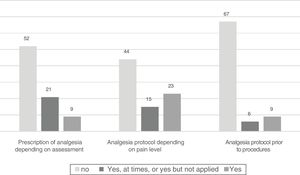
In units where pain assessment for both communicative and non-communicative patients was not standardised, analgesic drug prescription according to level of pain was not made in 52 (63.4%) of them. In 53.7%, there were no protocols for the administration of analgesics in keeping with level of pain and in 81.7% of the units there were no protocols for the administration of analgesics prior to painful procedures (Fig. 3).
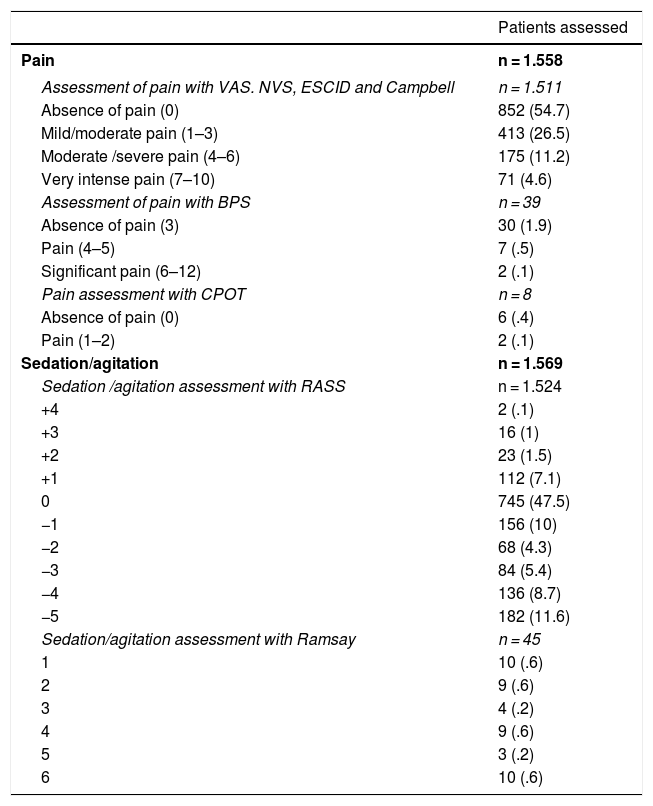
Patient dataOf the 1,574 patients included in the study, pain assessment in 13 of them was not possible due to perfusion of neuromuscular relaxants and in 3 due to lost data. Of the 1,558 assessed, 57% stated they did not have any pain (Table 5).
Direct assessments of the level of pain and sedation of the patients.
| Patients assessed | |
|---|---|
| Pain | n = 1.558 |
| Assessment of pain with VAS. NVS, ESCID and Campbell | n = 1.511 |
| Absence of pain (0) | 852 (54.7) |
| Mild/moderate pain (1–3) | 413 (26.5) |
| Moderate /severe pain (4–6) | 175 (11.2) |
| Very intense pain (7–10) | 71 (4.6) |
| Assessment of pain with BPS | n = 39 |
| Absence of pain (3) | 30 (1.9) |
| Pain (4–5) | 7 (.5) |
| Significant pain (6–12) | 2 (.1) |
| Pain assessment with CPOT | n = 8 |
| Absence of pain (0) | 6 (.4) |
| Pain (1–2) | 2 (.1) |
| Sedation/agitation | n = 1.569 |
| Sedation /agitation assessment with RASS | n = 1.524 |
| +4 | 2 (.1) |
| +3 | 16 (1) |
| +2 | 23 (1.5) |
| +1 | 112 (7.1) |
| 0 | 745 (47.5) |
| −1 | 156 (10) |
| −2 | 68 (4.3) |
| −3 | 84 (5.4) |
| −4 | 136 (8.7) |
| −5 | 182 (11.6) |
| Sedation/agitation assessment with Ramsay | n = 45 |
| 1 | 10 (.6) |
| 2 | 9 (.6) |
| 3 | 4 (.2) |
| 4 | 9 (.6) |
| 5 | 3 (.2) |
| 6 | 10 (.6) |
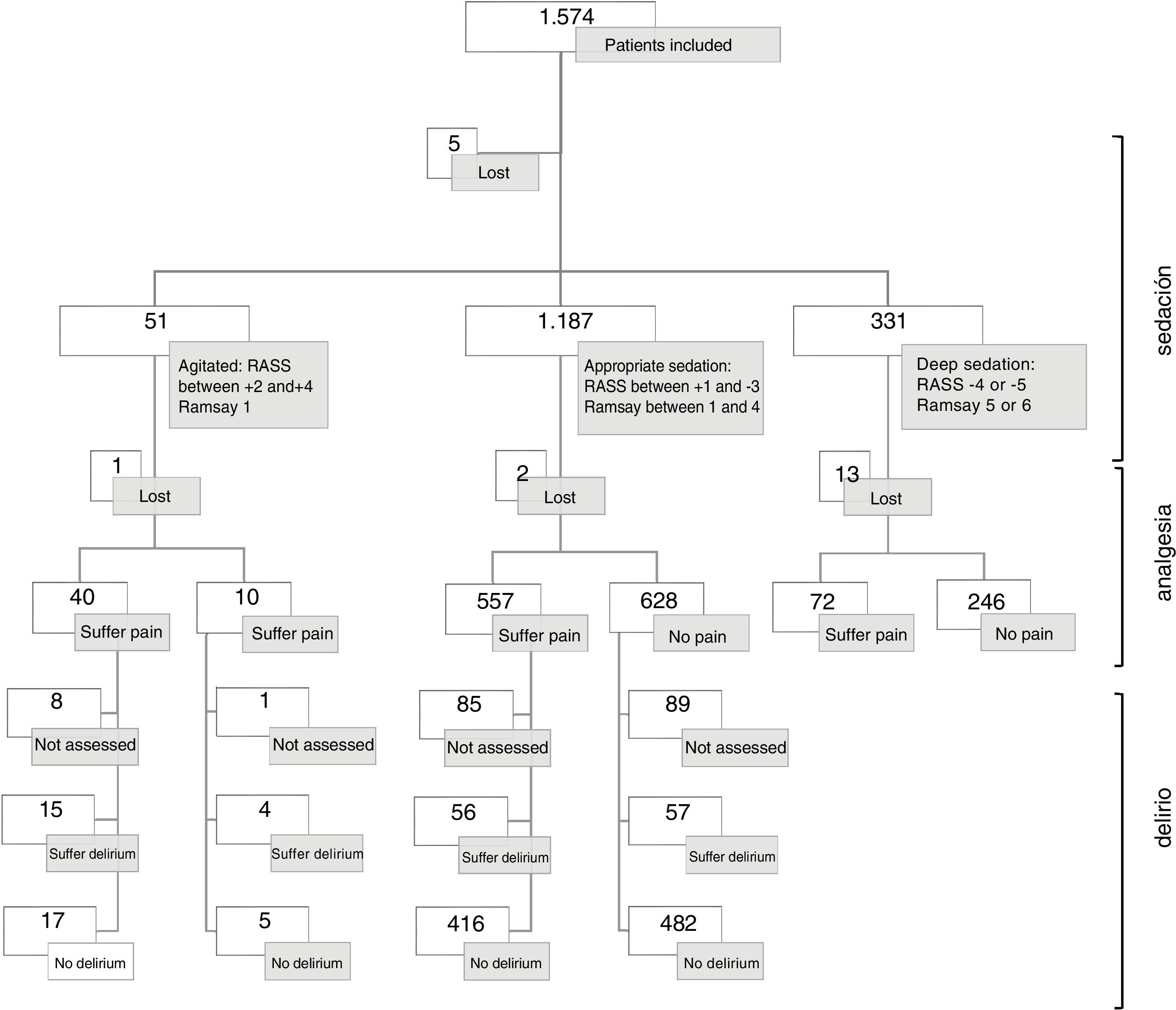
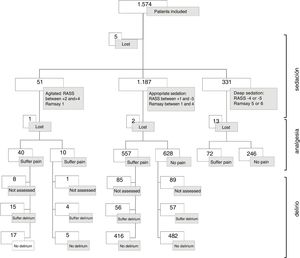
80% of agitated patients suffered pain, 46.8% of whom were considered to have appropriate sedation and 22.6% of patients with deep sedation (Fig. 4).
Comparing pain assessment in admitted patients in units with standardised pain assessment (837 patients) vs. units without standardized assessment (721 patients), the absence of pain was significantly more common in units where there was a standardized pain assessment (528 patients [63.1%] vs. 360 patients [49.9%]; p < .0001).
Analgesia was prescribed for 1,266 patients 80.4%), but only 157 (9.9% drugs were prescribed according to level of pain. 1,202 patients 76.4%) received analgesics (in boluses and/or perfusion).
Once thousand and sixty two patients (67, 5%) were monitored for pain level, or whom 929 (59%) were assessed at least once per shift and 133 (8.4%) once per day.
Sedation assessmentUnit dataOnly 57 units (36.1%) stated there was a specific analgesia and sedation protocol. In these units, individual adjustment of analgesics and sedatives were essentially performed according to the medical prescription of the dose (30 units [52.6%]), 12 units according to the algorithm by medical referral, 12 according to the autonomous algorithm by the nurse and in 3 units this was adjusted according to combinations of these options.
Sedation/ agitation assessment of patients was not made or was made without scales, in 3 units (8.2%) (Table 3); in 33 units (20.9%) this was performed occasionally and in 112 (70.9%) in a standardized manner. The level of sedation was monitored at least once per shift, in 96 units (60.8%) (Table 4).
The most commonly used scale was the RASS (122 units [77.3%]); in 7 units, apart from the RASS, they also used the Ramsay Score and/or the Bispectral Index (BIS) (Table 3).
The level of sedation, in the El 111 units which was assessed and recorded in a standardised manner, was performed by the nurses in 75.7% of the units, by the doctor in 2.7% and shared by both in 21.6%. In 70 of these 111 units (63%) sedatives were prescribed depending on the desired aim of sedation for the patient.
Standardised assessment of pain and sedation of all patients was performed in 77 units (48.7%).
Patient dataThe level of sedation/agitation was directly assessed in 1.569 patients (5 lost cases). In 1,524, the RASS was used and in 45 the Ramsay.
Seven hundred and fifty eight patients (48.3%) were reported as peaceful and collaborative (RASS 0, Ramsay 2-3); 163 patients (10.4%) as agitated (RASS +1a + 4, Ramsay 1) and 648 patients (41.3%) as sedated (Table 5).
Sedatives had been prescribed to 602 patients (38.4%), although only for 210 (13.3%) of them was this prescription conditioned by a sedation aim. 625 patients (39.7%) received sedatives (in bolus and/profusion). 526 patients (33.5%) were reported with sedation and invasive mechanical ventilation.
The sedation/agitation level of 394 patients (25.1%) was monitored: 333 with records. Every 8 h or less and 61 every 24 h.
Once thousand, one hundred and thirty three patients were included in the 111 units which assessed and registered the sedation in a standardised manner. In these units sedation/agitation was monitored every 8 h or less in 312 patients (27.5%), every 24 h in 39 (3.4%). The remainder of patients (782 [69%]) were not monitored for sedation/agitation level. Out of the 448 patients who received sedatives in these units, 378 (84.4%) had invasive mechanical ventilation.
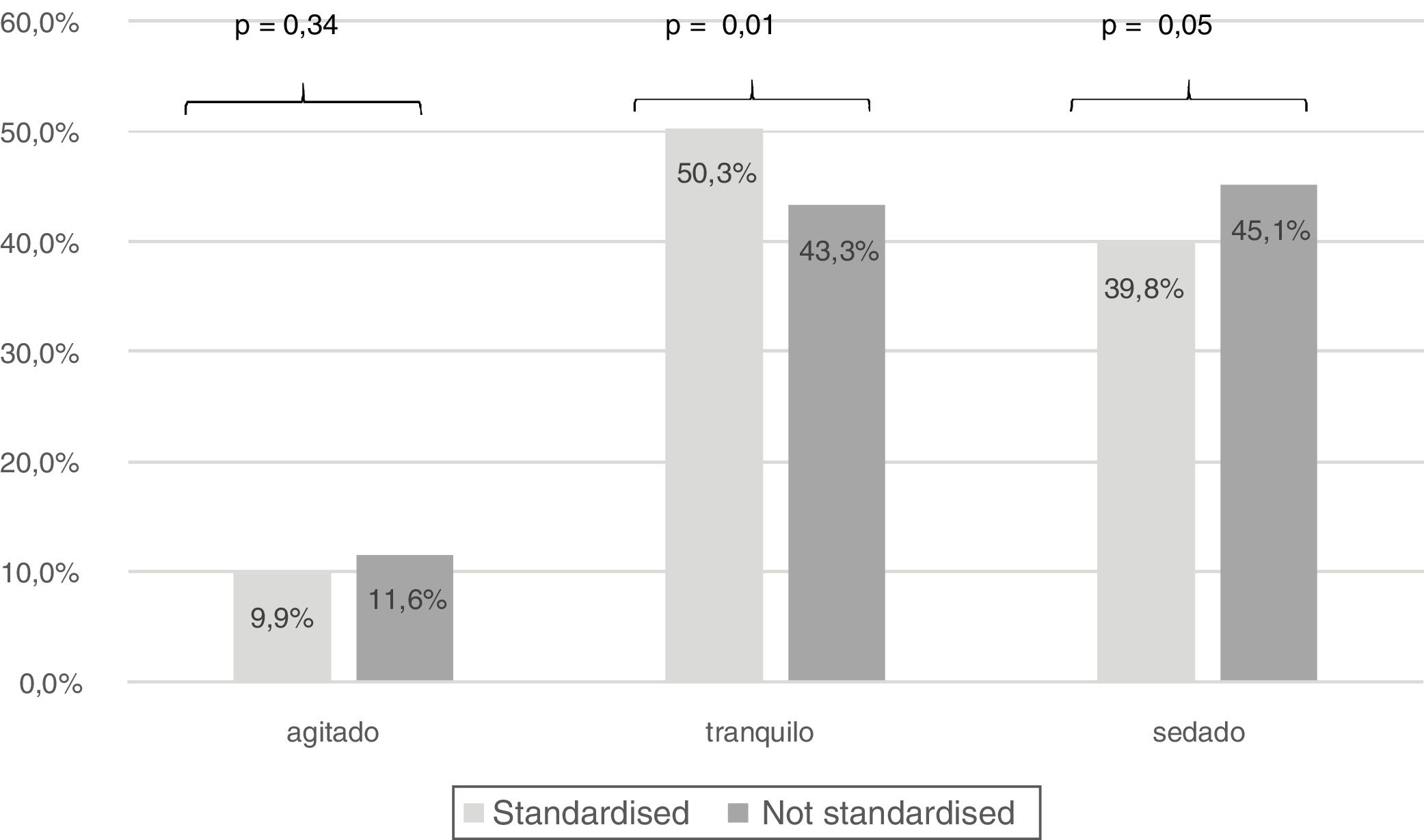
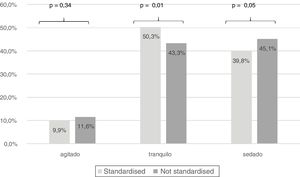
Comparing the assessment of sedation of patients admitted to units who were assessed in a standardised manner compared with the other units, we observed that there was a significant difference among peaceful patients (567patients [50%] vs. 191 other patients [43.8%]; p = .01) (Fig. 5).
Physical restraintUnit dataOut of the 158 participant units, 132 (83.5%) did not have a specific protocol for physical restraint for critically ill patients, and of the 26 units which did have them, in 12 this was not applied.
In 97 units (61.4%) physical restraint was never prescribed, and in the 61 in which it was prescribed, only in 51 exceptional cases (agitated/aggressive or psychiatric patients was physical restraint prescribed). The use of physical restraint was registered in 39 units (24.7%) globally and only in 13 (8.2%) of the 26 was there any specific protocol.
In 84 units (53.2%) it was the nurse who decided to carry out physical restraint, in 70 (44.3%) units this was decided by consensus between doctors and the nursing team and in 4 (2.5%) it was the doctor who took the decision. In 30 units (18.9%) the removal of physical restraint was standardized.
Informed consent for the application of physical restraint was verbally requested in 20 units (12.7%) and in 5 (3.2%) consent was both verbal and written.
Eleven units (6.9%) stated they used standardised assessment and recorded pain and sedation/agitation and also had a specific protocol for physical restraint and recorded its usage.
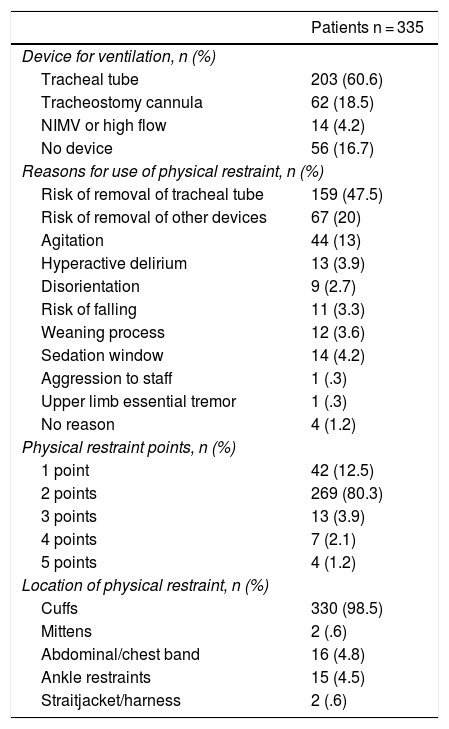
Patient dataThey were some type of physical restraint for 335 patients (21.3%). Only 15 physical restraint procedures were through medical prescription and 149 appeared in the clinical files.
Of the 335 patients with physical restraint, 60.6% had an endotracheal tube. The main reason for use of physical restraint was the risk of removal of the endotracheal tube or of other devices (67.5%). In 4 patients (1.2%) the collaborating nurse did not find any justification for the use of physical restraint. The most common method of restraint was with two point wrist cuffs (Table 6).
Data relating to the use of physical restraint.
| Patients n = 335 | |
|---|---|
| Device for ventilation, n (%) | |
| Tracheal tube | 203 (60.6) |
| Tracheostomy cannula | 62 (18.5) |
| NIMV or high flow | 14 (4.2) |
| No device | 56 (16.7) |
| Reasons for use of physical restraint, n (%) | |
| Risk of removal of tracheal tube | 159 (47.5) |
| Risk of removal of other devices | 67 (20) |
| Agitation | 44 (13) |
| Hyperactive delirium | 13 (3.9) |
| Disorientation | 9 (2.7) |
| Risk of falling | 11 (3.3) |
| Weaning process | 12 (3.6) |
| Sedation window | 14 (4.2) |
| Aggression to staff | 1 (.3) |
| Upper limb essential tremor | 1 (.3) |
| No reason | 4 (1.2) |
| Physical restraint points, n (%) | |
| 1 point | 42 (12.5) |
| 2 points | 269 (80.3) |
| 3 points | 13 (3.9) |
| 4 points | 7 (2.1) |
| 5 points | 4 (1.2) |
| Location of physical restraint, n (%) | |
| Cuffs | 330 (98.5) |
| Mittens | 2 (.6) |
| Abdominal/chest band | 16 (4.8) |
| Ankle restraints | 15 (4.5) |
| Straitjacket/harness | 2 (.6) |
NIMV, non invasive mechanical ventilation.
Ninety four adverse events were reported, in direct observation of the collaborating nurse, related to the use of physical restraint. The most frequent were oedemas (48 patients) or reddening (38 patients) in the area of physical restraint application. Also, 3 skin lesions were observed, one vascular lesion and in 4 an increase in restlessness or irritability.
In the clinical files, 28 episodes of increase in agitation or disorientation were recorded after applying physical restraint and 25 oedemas, reddening or skin erosions in the area of application.
Assessment of deliriumUnit dataOnly in 53 units (33.5%) was a scale used to diagnose delirium (Table 3). Assessment and recording of the scales was performed in 46 of the 53 units, but only in 39 was this standardized (24.7% of the participating units).
Nineteen (48.7%) of the units with standardised assessment stated they did not assess patients if there were no suspected signs or symptoms of delirium. The other cause to not assess patients was having a RASS score under ―2 (5 units).
There were protocols for the prevention of delirium and for the management of patients with delirium in 29 units (18.3%). Of the 39 units with standardized assessment, 19 (48.7%) did not have these protocols. In 24 units (15.2%) they stated that there was a protocol available to facilitate rest and sleep for the patient.
Regardless of the existence or not of protocols, in 149 units (94.3%) they referred to reorientation in time, person, and space as a non pharmacological activity for patients in the prevention and/or treatment of delirium; managing the stressful environmental conditions in 135 units (85.4%)and the proximity and participation from family members in 125 (79.1%).
Standardized use of assessment and registering of pain, sedation/agitation and delirium was reported by 33 units (20.9%). In 8, of them there was also a specific protocol for physical restraint and its application was recorded.
Patient dataIt was possible to assess delirium in 1,058 patients. The reasons referred to by the collaborating nurses for non assessment were mostly those of deep sedation of patients 64%); non ability to communicate, despite not being deeply sedated for 173 patients (33.9%); suffering from Alzheimer’s for 3 patients, and lost data for 9 patients.
Delirium was identified in 133 patients (12.6%). Of them for 51 (38.3%) this diagnosis had been recorded in their medical file.
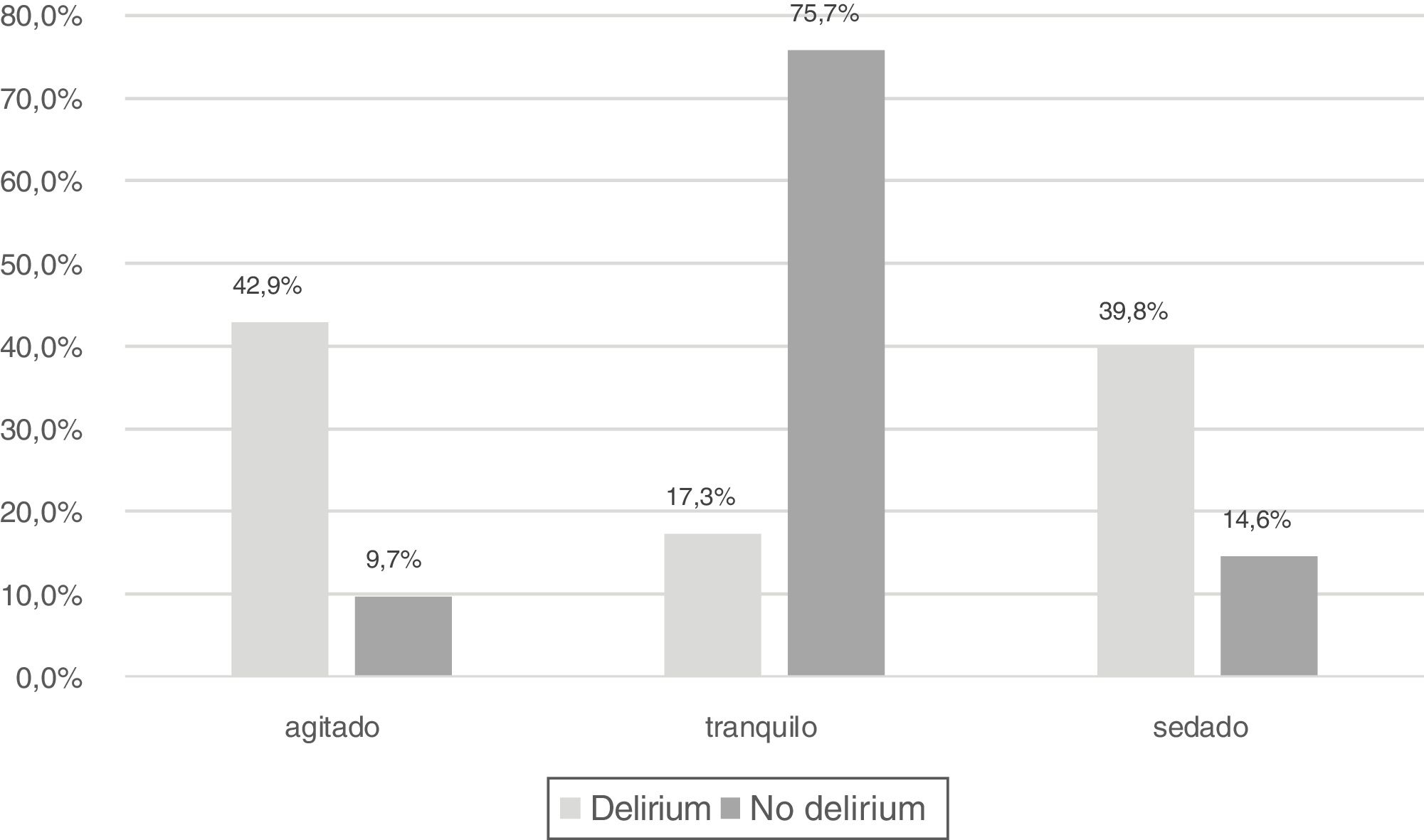
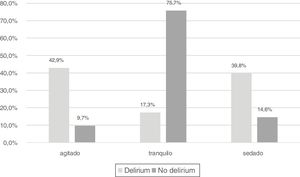
It was observed that 42.9% of those who had delirium were agitated (RASS > 0 or Ramsay 1), 17.3% were peaceful (RASS 0 or Ramsay 2–3) and 39.8% had superficial sedation (Fig. 6).
DiscussionOur main observations were:
- 1
There is moderate follow-up, but higher to that published, of recommendations on the assessment of analgesia, sedation, delirium and the use of physical restraint.
- 2
The assessment of sedation, analgesia and delirium vary greatly between units.
- 3
There is higher standardization in the assessment of sedation than in the assessment of pain and a low to moderate standardisation of assessment of delirium and the use and control of physical restraint.
- 4
Validated tools for assessment of these strategies are well known in the majority of units, with a lower awareness of those of delirium.
- 5
A high percentage of patients referred to pain.
- 6
The proportion of patients with agitation is low.
- 7
A low incidence of delirium was reported.
- 8
A moderate prevalence in the use of physical restraint.
The pain of communicative patients was assessed more than that of non-communicative patients (88% vs. 64%). Although the assessment with scales is high, the proportion of units with standardized follow-up of these assessments is low (69% vs. 53%).Notwithstanding; our data are high when compared with other studies.17-21
After a survey with nurses of 291 ICUs in 22 European countries Egerod et al.17 reported a global formal assessment of pain in 237 units (81%). Their data for assessing pain in communicative patients (70%) are similar to ours. However, only 23 units (8%) use scales for non-communicative patients. Luetz et al.,18 in a European survey in 101 units, refer to assessing pain with scales in 71% of units globally and in 24% in non-communicative patients. Assessment with scales reported in our study is also higher than in other studies.19–21
In a survey conducted in 704 hospitals in China, Wang et al.19 reported 45.8% of clinics that assessed pain with scales; in the survey made by Sneyers et al.20 in 101 Belgian ICUs, only 11% of those surveyed used validated scales to assess pain in non-communicative patients, and Burry et al.,21 in their study in 51 Canadian units, observed a use of scales in 47.1% of units, although none of them used scales to assess pain in non-communicative patients.
Regarding the scales used, we found there were differences to that published. The majority used the BPS17 or CPOT19 scales, as recommended by the clinical practice guidelines of the American College of Critical Care Medicine2, although the guide from the Pan-American and Iberian Federation of Societies of Intensive and Critical care Medicine7 mentions the possibility of assessing with ESCID and does not consider BPS or CPOT to be superior to it. In our study the most commonly used scale was ESCID, possibly because it is a scale that has been created and validated in Spanish,22 whilst BPS and CPOT have not been validated into Spanish.
According to the clinical practice guidelines,2,7,8 the systematic assessment of pain should be standard, at least once per shift (every 8 h), since monitoring improves effective pain control and enables better adjustment to medication. The units surveyed in our study report monitoring every 8 hours or less, to communicative patients, 67% of units, and in 52% to non-communicative patients. In the units which assessed both, the percentage was slightly lower (48.7%). We may therefore consider that adherence to this recommendation is moderate.
One relevant aspect is the fact that, although 80% of patients had analgesics prescribed to them and 59% had pain monitored every 8 h or less, 43% of patients stated they felt pain. This data surpasses that reported by Shehabi et al.,23 in a multicentre study with 251 patients in 25 units in Australia and New Zealand, where 7.2% of patients had pain on the first day of the study and 23.5% during the first 48 h. it is possible that this is related to the fact that only 32% of participating units had analgesia protocols according to pain level and 15% protocols which included analgesia for painful procedures. Also, analgesics were only prescribed according to pain level in 30 units (19%).
SedationA high number of units (92%) assessed sedation/agitation of patients with validated scales, although fewer assessed this and monitored it in any standardised manner (70%).
Our data are higher than those reported by Soliman el al.,13 in a survey introduced in 16 European countries published in 2001, with a mean percentage of usage of sedation scales of 43%. The results of the Spanish units were presented with those of Portugal, reporting a usage percentage of sedation scales of 65%. Although Spanish representation was low, our data suggest that in 2018 the implementation of the scales was much broader. Burry et al.,1 in their most recent study conducted in Canada, also reported lower percentages of scale usage (47.1%) in the 51 participating units.
High percentages similar to ours found in recent publications in Europe,17 United Kingdom,24 North America25 and China,19 with usage rates of between 83% and 91%. Lower data of sedation scales use are reported by Martin el al.26 in their survey in Germany where it was monitored in 30% of hospitals, or by Kotfis et al.27 in Poland, with 46% of scale usage.
Although the guides2,5,6 recommend the use of the RASS compared with Ramsay, the latter is the most used in the published studies.13,24–27 In our study, the majority use is that of the RASS (77%), and only 8% of the units used the Ramsay scale. We also found that 5.7% of units used BIS as the only method of assessment for sedation. Although their use for monitoring sedation is only recommended in patients with neuromuscular blocking agents, 4 out of the 9 units using them were surgical units where patients were already admitted into the unit with the BIS sensor.
In direct patient assessment, we observed that 75% had an appropriate sedation level. Also, the units with standardization in assessment and recording of sedation had a higher percentage of peaceful patients and, although not significant, lower percentage of sedated patients. These data could indicate that monitoring of the sedation level would help to better adjust medication and the consequence of superficial or conscious sedation, as recommended in the guides.2,5
Despite the high number of units which refer to monitoring sedation normally (70%) and in which 63% prescribed sedatives with the aim of sedation, only 25% of patients had sedation/agitation records. This would possibly be due to the fact that only 40% of the patients received sedatives and in many protocols only sedation assessment in these patients was considered.
Physical restraintMore than a fifth of the patients assessed (21.3%) received physical restraint. Previous studies in Spain had documented prevalence in the use of physical restraint between 15.6%28 and 44%–45%29,30 Also, international figures of its prevalence in ICUs in some studies go up to 75% of patients with mechanical ventilation.31 Benbenbishty et al.,30 in their study in 34 European units observed that there was a global usage rate of 39%, with high variability (0–100%) between countries and participating units. This variability may be due, among other reasons, to nurse: patient ratios, the percentage of patients with mechanical ventilation, the level of sedation, the sedation strategy or the consideration of lateral bed rails as a method of contention. Further study is needed in the use of sedatives as contention, and sedation level and strategy. Martín et al.28 report that 48% of patients received pharmacological contention. Furthermore, Rose et al.31 report that patients with physical restraint are more agitated and have received higher doses of benzodiazepines, opiates and antipsychotic drugs. We are unaware of the data of possible pharmacological contention in our study, but only 21% of patients were under deep sedation.
The reasons justifying the use of physical restraint are similar to those published,12,26,29,30 underlining the risk of endotracheal tube removal as the main reason for applying them. However, to date it has not been demonstrated that the use of physical restraint is effective and safe to avoid auto-removal of devices and its use is anyway associated with the appearance of adverse events, such as skin lesions or higher agitation and delirium,5 effects which were also observed in the patients in our study.
Another outstanding aspect is the recording of the use of physical restraint in less than half of patients who receive it and that only in 51 units was it prescribed in exceptional cases, with nurses being those who mainly take the decision. Acevedo et al.12 reported the possibility of a nurse’s prescription for physical restraint, which would possibly raise greater awareness on its routine use. Also, only in 25 units did they request some type of family consent. Following the recommendations of the international guidelines,32 on such a sensitive and ethically questionable issue as the immobility of a patient in the bed, the decision for using physical restraint should always be taken in agreement with the team, informing the family and never should be the decision of a single professional. In keeping with this, the invisibility of physical restraint is also evident by the fact only 16.4% of units have a specific protocol of physical restraint for the critical patient, with this being an indicator of quality for their care.33 This figure is below that published by López et al.,34 where after a survey of 68 Spanish ICUs the presence of contention protocols was described in 40% of units. Furthermore, De Jonghe et al.35 reported 21% of units with specific protocols, in a study which included 121 French units. Regulation of the use of physical restraint in the ICU should be optimised, aimed at greater reflection on use, bearing in mind the specificities of the critically ill patient and the risks use entails, without forgetting that the measures of contention must always be assessed in an individual manner with rigour and reflection aimed at not causing greater damage.
DeliriumUsage of delirium diagnosing tools is low and standardisation of its assessment is present in under a fourth of the participating units. The CAM-ICU is the most heavily used tool which coincides with general practice.36
Although this study does not attempt to cover the barrier for non compliance with guideline recommendations and the underutilisation of assessment tools, there is no doubt that staff training and inappropriate development of competences in scale implementation are significant factors, as reported by Rowley-Conwy,37 in addition to the complication of applying it to intubated patients.38
Our data are similar to that presented by Patel et al.25 and Egerod et al.,17 with usage rates of 33% and 37%, respectively, and higher than those reported by Burry et al.21 and Kotfis et al.,27 with rates of 13.7% and 10.9%, respectively.
The rate of delirium prevalence observed in our study between the patients who could be assessed, is below that published.
In a systematic review published in 2015 Salluh et al.36 reported an overall prevalence in the 44 articles analysed of 31.8%, although there was huge diversity (between 9% and 91%), possibly conditioned by the clinical characteristics of the patients included and the study designs. This global prevalence is similar to that reported by Salluh et al.39 in a multicentre study in 2009, with 32% of patients with delirium, and a systematic review published by Zhang et al.40 in 2013, where a global prevalence of 30% was reported, but which was equally quite diverse (between 16% and 81.7%). In our study we assessed the presence of delirium in patients admitted with the ability to communicate, regardless of whether mechanical ventilation was being used or not, and this contributed to the low rate observed.
Another possible cause of our low rate of prevalence could be the rate of patients who could not be assessed due to deep sedation or communication difficulties. Swan et al.41 observed that the rate of patients who could not be assessed significantly dropped after educational intervention (22% vs. 11%; p = .03). In our study we have a higher rate of non assessment, but the collaborating nurses had audiovisual material to be trained in the appropriate manner on the CAM-ICU. It is possible that lack of experience in the use of this tool would increase this rate, lowering that of delirium.
It should be taken into consideration that although only 18% of units had a prevention and treatment of delirium protocol, the units which used non pharmacological methods of prevention were high (higher than 79%). Furthermore, we also consider that the percentage of patients without pain or with moderate pain was 84%., 75% had an appropriate level of sedation and the rate of the use of physical restrain was not very high (21%). All of these are major factors which could have contributed to this low prevalence.
Study limitationsOur study may have the limitations associated with a study based on the completion of surveys. There could be misunderstanding of the meaning of the questions, responses in blank or wrong answers. We attempted to minimize this bias in this study, because the coordinator researcher contacted all the collaborating nurses and resolved doubts. This contact between collaborating nurses and coordinator may also have mitigated the social desirability bias that leads us to answer according to our desires and not according to reality. Another limitation would be the number of participating units. Although there is not official census of the number of ICUs in Spain we believe our sample is representative of the practice of intensive nursing in Spain.
ConclusionsThis study has shown that in a high proportion of Spanish ICUs pain, sedation and delirium of patients is assessed, albeit not in any protocolised or standardized manner, and the use of physical restraint is not high. A high proportion of patients refer to pain, mostly moderate pain, and the percentage of agitated patients is low. We also observed that there was a low rate of delirium, and specific analysis would be required to know the reason for this.
In view of the results obtained, protocols may be generalised and extended, to allow for the assessment, prevention and treatment of pain and delirium using an appropriate management of analgesia, sedation and non pharmacological measures.
FinancingThis study did not receive any financing, but was promoted by the Spanish Society of Intensive Nursing and Coronary Units (SEEIUC).
Conflict of interestThe authors have no conflict of interests to declare.
Coordinator: Cindia Morales Sánchez (Hospital Universitario Virgen del Rocío, Seville). Authors: Juan José García Morales (Hospital de Poniente, El Ejido); Francisco Caballero Moreno (Hospital Universitario Puerta del Mar, Cádiz); María Paines Real Prado (Hospital San Rafael, Cádiz); Ángel Cobos Vargas (Hospital Campus de la Salud, Granada); María Esther Rodríguez Delgado (Hospital Comarcal Santa Ana, Motril); Juan Ángel Hernández Ortiz (Hospital Universitario de Jaén, Jaén); Jorge Castillo Morales (Hospital Costa del Sol, Málaga); María Luisa Amador Mateos (Hospital Universitario Virgen del Rocío, Seville); Ascensión Ruiz Flores (Hospital Nuestra Señora de Valme, Seville); Valle Fernández Vera (Hospital San Agustín, Dos Hermanas).
Coordinator: Delia María González de la Cuesta (Hospital Royo Villanova, Zaragoza). Authors: M. Carmen Pérez Martínez (Hospital Obispo Polanco, Teruel); Elena Casanova Train, Tamara Valero Vicente, Alberto Moya Calvo, Rubén Ramos Abril (Hospital Universitario Miguel Servet, Zaragoza); María Inmaculada Pardo Artero, Marta Palacios Laseca (Hospital Clínico Universitario Lozano Blesa, Zaragoza); M. del Mar Rello Echazarreta (Hospital Royo Villanova, Zaragoza).
Coordinator: Emilia Romero de San Pío (Hospital Universitario Central de Asturias, Oviedo). Autoras: M. Cristina González Leyva (Hospital Universitario San Agustín, Avilés); Yolanda Menéndez Carballo (Hospital Carmen y Severo Ochoa, Cangas de Narcea); Paz de la Peña Ripodas (Hospital Valle del Nalón, Langreo); Ana Wensell Fernández, Diana García García, María Teresa Valdés Fernández, María Vanessa Espeso García (Hospital Universitario Central de Asturias, Oviedo); Vanessa Moriyón Cortina (Hospital Universitario de Cabueñes, Gijón).
Coordinator: María Acevedo Nuevo (Hospital Universitario Puerta de Hierro Majadahonda, Majadahonda). Autoras: Celia Sánchez Calvín, M. José Jovani Martín (Hospital Universitari Son Espases, Palma).
Coordinador: Yeray Gabriel Santana Padilla. Authors: Yeray Gabriel Santana Padilla (Hospital Universitario Insular de Gran Canaria, Las Palmas de Gran Canaria); Beatriz Yánez Quintana (Hospital Universitario de Gran Canaria Doctor Negrín, Las Palmas de Gran Canaria); Laura Vanesa Saavedra Körbel (Hospital General de Fuerteventura, Puerto del Rosario); Isabel Vanesa Melián Castro (Hospital San Roque Maspalomas, San Bartolome de Tirajana); Francisco J. Clemente López (Hospital Universitario Nuestra Señora de la Candelaria, Santa Cruz de Tenerife).
Coordinador: José Luis Cobo Sánchez. Authors: José Luis Cobo Sánchez (Hospital Universitario Marqués de Valdecilla, Santander); Ignacio Velasco Aja (Hospital Sierrallana, Torrelavega).
Coordinador: Juan Carlos Muñoz Camargo (Hospital General Universitario de Ciudad Real, Ciudad Real). Authors: Lucía Tornero Sánchez (Complejo Hospitalario Universitario de Albacete, Albacete); Anastasio Garrido Avileo (Hospital General Universitario de Ciudad Real, Ciudad Real); Mónica Bascuñana Blasco (Hospital Virgen de la Luz, Cuenca); César Rojo Aguado (Hospital Universitario de Guadalajara, Guadalajara).
Coordinator: Susana Arias Rivera (Hospital Universitario de Getafe, Getafe). Authors: M. Isabel Ballesteros Vega (Hospital el Bierzo, Ponferrada); M. Luz Robles López (Hospital de León, León); Ana Belén Martín Santos, María Teresa García Hernández (Hospital Clínico Universitario, Valladolid); M. del Mar Aroca Gaitán, Sonia del Olmo Núñez (Hospital Universitario Río Hortega, Valladolid); Julio Vicente Gil García (Hospital Nuestra Señora de Sonsoles, Ávila).
Coordinators: Gemma Via Clavero (Hospital Universitari de Bellvitge, l'Hospitalet de Llobregat); Diana Gil Castillejos (Hospital Universitari Joan XXIII, Tarragona); Gemma Robleda Font (Hospital de la Santa Creu i Sant Pau, Barcelona). Authors: Gemma Via Clavero, Olga Vallés Fructuoso (Hospital Universitari de Bellvitge, l'Hospitalet de Llobregat); Marta Navarro Colom, Inés Loder (Hospital de la Santa Creu i Sant Pau, Barcelona); Immaculada Amenós Alcaraz (Hospital de Mataró, Mataró); Miriam E. Secanella Martínez (Consorci Corporació Sanitària Parc Taulí, Sabadell); Gemma Martínez Estalella, Miquel Àngel Sanz Moncusí, Miguel Ángel Giménez Lajara, Mercè González González, Immaculada Carmona Delgado, Joan Roselló Sancho, Ernest Andrés Casamiquela (Hospital Clínic de Barcelona, Barcelona); Elisabeth Gallart Vive, María Alba Riera Badia, Vanesa Estudillo Pérez, Gemma Marín Vivó (Hospital Universitari Vall d’Hebron, Barcelona); Anna Jorge Castillo (Hospital Universitari Mútua de Terrassa, Terrassa); David Manzanedo Sánchez, Gemma Gimeno Palomar (SCIAS Hospital de Barcelona, Barcelona); Diana Gil Castillejos, M. de los Ángeles de Gracia Ballarín (Hospital Universitari Joan XXIII, Tarragona); Cristina Paños Espinosa (Hospital Sant Pau i Santa Tecla, Tarragona); Miguel Querol de Cárdenas (Hospital Universitari de Sant Joan, Reus); Eva María Torondel Capdevilla (Hospital Verge de la Cinta, Tortosa); María Miralles Balagué (Hospital Universitari Arnau de Vilanova, Lleida); Aaron Castanera Duro, Andrea García Lamigueiro (Hospital Universitari Dr. Josep Trueta, Girona).
Coordinator: Susana Arias Rivera (Hospital Universitario de Getafe, Getafe). Autor: José Antonio Casas García (Hospital Universitario Infanta Cristina, Badajoz).
Coordinator: M. del Rosario Villar Redondo. Autoras: M. del Rosario Villar Redondo, M. Cristina Benítez Canosa (Complexo Hospitalario Universitario de Santiago de Compostela, Santiago de Compostela); Paula Boga Veiras (Hospital de Conxo, Santiago de Compostela); María Soledad Rodríguez Bao (Hospital Universitario Lucus Augusti, Lugo); Marta Fórneas Iglesias (Hospital da Costa, Burela); Yolanda García Fernández (Complexo Hospitalario Universitario de Ourense, Ourense); MauIQRio Díaz Alvarez (Complexo Hospitalario Universitario de Pontevedra, Pontevedra); Carmen Pazos Jardón (Hospital Povisa, Vigo).
Coordinator: Susana Arias Rivera (Hospital Universitario de Getafe, Getafe). Autora: Sofía Pérez Rovira (Complejo Hospitalario San Millán y San Pedro, Logroño).
Coordinators: M. Jesús Frade Mera (Hospital Universitario 12 de Octubre, Madrid); Susana Arias Rivera (Hospital Universitario de Getafe, Getafe). Authors: Verónica Bazán Vega (Hospital Universitario Príncipe de Asturias, Alcalá de Henares); Josefa Escobar Lavela (Hospital Universitario del Sureste, Arganda del Rey); Fernando Pascual Basurto (Hospital General de Villaba, Collado Villalba); Verónica Munuera Monzo (Hospital Universitario del Henares, Coslada); M. del Mar Sánchez Sánchez, Juan Carlos Quintero Olivares (Hospital Universitario de Getafe, Getafe); Ana Isabel Nogales Mancera, Sara Herrero Jaén (Hospital Universitario Severo Ochoa, Leganés); Noelia Regueiro Díaz, Luis Fernando Carrasco Rodríguez-Rey, M. del Rosario Hernández García, Candelas López López (Hospital Universitario 12 de Octubre, Madrid); Tamara Raquel Velasco Sanz, Ana Belén Sánchez de la Ventana (Hospital Universitario Clínico San Carlos, Madrid); Moisés García Martínez (Hospital Central de la Defensa Gómez Ulla, Madrid); M. José Toraño Olivera, Luis Guerra Sánchez, Mónica Juncos Gozalo (Hospital General Universitario Gregorio Marañón, Madrid); Juan Ángel Toledano Peña, Susana Rodríguez Domínguez (Hospital Universitario de la Princesa, Madrid); M. Cruz Morales Cobo, Olga Hernández Fernández, María Aguilar Mora, M. del Mar Buñuel González, Jesús Morente López (Hospital Universitario de la Paz, Madrid); Ana Castillo Ayala, Rocío González Blanco, Lourdes Moreno-Manzano Rodríguez-Palmero (Hospital Universitario Ramón y Cajal, Madrid), María Acevedo Nuevo, Ignacio Latorre Marco (Hospital Universitario Puerta de Hierro Majadahonda, Majadahonda), Saúl García González (Hospital Universitario de Móstoles, Móstoles), Alba Camacho Fernández (Hospital Universitario Infanta Cristina, Parla), Concepción Faura Santos (Hospital Universitario de Torrejón, Torrejón de Ardoz), Sergio Domínguez García (Hospital Universitario Infanta Elena, Valdemoro), M. Clotilde Aguilera Sevilleno (Hospital Universitario Infanta Leonor, Madrid).
Coordinador: Juan José Rodríguez Mondéjar (Gerencia de Urgencias y Emergencias, Servicio Murciano de Salud, IMIB-Arrixaca). Authors. Antonio Ros Molina (Hospital Universitario Rafael Méndez, Lorca); Daniel Linares Celdrán (Hospital General Universitario Santa Lucía, Cartagena); Nieves Paines Escudero López (Hospital General Universitario Los Arcos del Mar Menor, San Javier); Ana Belén García García (Hospital Clínico Universitario Virgen de la Arrixaca, Murcia); Lucía Navarro Sanz (Hospital General Universitario Reina Sofía, Murcia); Francisco José Martínez Rojo (Hospital General Universitario José M. Morales Meseguer, Murcia).
Coordinator: Andrea Fadrique Hernández (Complejo Hospitalario de Navarra, Pamplona). Autoras: Sandra Arizcun González (Hospital García Orcoyen, Estella-Lizarra); Rosana Goñi Viguria (Clínica Universidad de Navarra, Pamplona); Amparo Martínez Oroz, Bárbara Mailén Moyano Berardo (Complejo Hospitalario de Navarra, Pamplona); María Ángeles Zapata Roig (Hospital Reina Sofía, Tudela).
Coordinator: M. del Carmen Górgolas Ortiz (Hospital Universitario de Basurto, Bilbo). Autoras: Pablo Alegre Orue, Jorge Barrenetxea Gallano (Hospital Universitario de Basurto, Bilbo); Yolanda Gómez Gómez, Maria Luisa Millán Salazar (Hospital Universitario de Cruces, Barakaldo); César Rodríguez Núñez, Marta Martín Martínez (Hospital Universitario de Araba, sedes Txagorritxu y Santiago, Vitoria-Gasteiz).
Coordinator: Gemma Leiva Aguado (Hospital Universitari y Politècnic La Fe, Valencia). Autoras: Pablo Pascual Hervas (Hospital Universitario de La Plana, Villareal); Marian Moran Marmaneu (Hospital General Universitario, Castellón); María M. Adell Artola (Hospital Comarcal de Vinarós, Vinarós); Elena Santiago Cisternas, Yolanda Martínez Gimeno (Hospital Universitari y Politècnic La Fe, Valencia); Asunción Royo Calvo (Hospital de Sagunto, Sagunt); José Luis Tato Tato (Hospital Francesc de Borja, Gandía); Javier Inat Carbonell (Hospital Clínico Universitario, Valencia); Dunia Valera Talavera (Hospital Universitario Dr. Peset Aleixandre, Valencia); Manuela Sarmiento Jara (Hospital de la Vega Baja, Orihuela); Joaquín Morante Martínez, Beatriz Martínez Sánchez (Hospital General Universitario de Elche, Elche); Mónica Yañez Cerón (Hospital General Universitario de Elda, Elda); María Carmen Prieto Pagán (Hospital Universitario de Vinalopó, Elche).
Members of the ASCyD team are enlisted in the Appendix.
Please cite the article as: Arias-Rivera S, López-López C, Frade-Mera MJ, Via-Clavero G, Rodríguez-Mondéjar JJ, Sánchez-Sánchez MM, et al. Valoración de la analgesia, sedación, contenciones y delirio en los pacientes ingresados en unidades de cuidados intensivos españolas. Proyecto ASCyD. Enferm Intensiva. 2020;31:3–18.