The environment and settings of Intensive Care Units can seem hostile for patients and their family members. The description of the experiences of anonymous patients1 and patients with social relevance2,3 attest this. Although in these descriptors it is hard to distinguish which part is associated with the settings and which is inherent to the pathology for which the patient was admitted to the Intensive Care Unit. Based on these and other arguments, “humanization” plans for Intensive Care Units have started to be implemented.4
Is it necessary to “humanize” Intensive Care Units? The dictionary of the Real Academia Española (Royal Spanish Academy) defines humanizing as making something or someone human, familiar or affable. If the goal is linked to this last meaning (making something human, such as the work environment), this initiative is very welcome. The main causes of patient dissatisfaction are related to the environmental aspects of the units (lack of intimacy and excess light and noise5–9). However, in the plan's introduction, the authors put greater emphasis on changing health professionals: “The definite goal is to achieve greater closeness, understanding, affection and tenderness, increasing our capacity for self-criticism and persevering in our constant desire for improvement. Recovering the commitment of service and delivery, which originally fueled our vocation as professionals, constitutes a challenge and a necessity of great magnitude and general interest”. Why do the authors assume that the professionals who work or have worked in Intensive Care Units lack or have lost the qualities that they wish to promote? Is there any study supporting a statement that disregards the work of many professionals since the beginning of Intensive Care Units in Spain? Based on the satisfaction surveys answered by patients admitted to our Intensive Care Units and their family members, it can be concluded that a high percentage of respondents were satisfied with health staff's care and empathy.5–8,10,11 Although, the results of these studies prove that there is still room for improvement, not only with regard to the units’ design, but also to the staff's degree of empathy with the family members’ feelings and concerns6,8,12,13 and to the transmission of medical and nursing information.12,13
The first program of the plan that was implemented was called “open-door ICUs”. After observing that the measure could be benefitial,13,14 Henneman,15 proposed several steps, prior to modifying the visits toward a more flexible approach tending to what is known as “family-centered critical care”, which entails, among others:
- 1.
Knowing the real needs of the family members. There is no evidence that a prior analysis of the family members’ needs was carried out in those units in which the program has already been implemented. Although, in general terms, the visiting policy is considered to be restrictive,5,8,13,16 this fact has its nuances. The family members of conscious patients tend to demand more visiting time, whereas the family members of intubated patients and those under analgesia or sedation consider that the established visiting time is adequate, probably due to the fact that they do not know how to behave in these conditions.5 In a recently published survey asking the following question: “Would it seem appropriate to have open access to visit your family member from 10 am to 11 pm?”, 78% of respondents answered no11. Furthermore, a state of anxiety and “guilt” may arise and, in fact, has already been evidenced in some units, among family members who, for several reasons, cannot stay with their loved ones on a permanent basis but they “feel obliged” to be there all the time. In a study carried out in an Intensive Care Unit in Paris (France), with a 24-h open access policy, it was observed that most visits from family members took place between 14h and 20h, and had a mean duration of 1–2h/day, very few visits were received at night and only two family members of the total of 209 patients included in the study, spent the night in the patients’ rooms.17 Therefore, we recommend that the visiting schedule be agreed upon between the patient (whenever he or she is competent for such task), the family members and the nursing staff.18
- 2.
Integrating these values into the unit's usual standards and policies. The plan of the Community of Madrid states that, prior to increasing the flexibility of visits, an assistance visiting protocol must be developed, including an assessment of the opinions of health professionals, the conduct of training activities and the drafting of a consensual document regarding the visiting and accompaniment policy. To this day, health professionals have not been taken into account19 and no assistance protocol has been published despite the fact that the measure has already been implemented in some units.
- 3.
Accommodating the necessary hospital resources. The plan of the Community of Madrid recognized that the physical settings of ICUs must ensure that the healthcare process is linked to a healthy environment that helps improve the physical and psychological condition of patients, health professionals and family members. An environment avoiding structural stress and promoting well-being.4 Therefore, the plan4 envisages that at the end of 2019, 100% of “boxes”–which should probably be called rooms, as this term is considered to be more human, although the dictionary of the Real Academia Española uses the term “box”, to define the compartment reserved to patients admitted to an emergency room or who need to be isolated, as well as for stables and racing cars–must be private and 60% of “boxes” shall be individual; however, to this day there is no record that this modification will be implemented in units that do not meet these standards. There is only information regarding the reform of a waiting room of a private hospital of the Community of Madrid.20 In fact, the Director General of Coordination of Citizen Care and Humanization of Healthcare of the Community of Madrid has recognized that, for the moment, said program has no budget.19
The plan of the Community of Madrid does not contemplate the assessment of the impact of this measure. Because, despite the extensive literature available in this respect, few studies have assessed its impact on the patients’ relevant outcomes, such as the need for sedation and analgesia, the incidence of delirium or the length of stay at the Intensive Care Unit.14
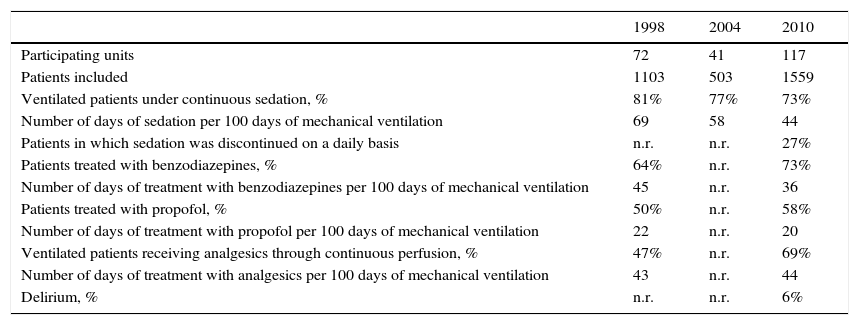
Also, the plan does include the impact assessment of other measures included within it, such as the management of patients’ sedoanalgesia and the incidence of delirium. In this sense, it should be noted that Spanish intensivists had already gradually implemented improvement measures in this regard. Recent studies on the implementation of protocols21 and evolutionary analyses of observational studies (Table 1) attest to this.
Evolution of sedoanalgesia in patients receiving mechanical ventilation in Spanish units participating in three international studies on mechanical ventilation.
| 1998 | 2004 | 2010 | |
|---|---|---|---|
| Participating units | 72 | 41 | 117 |
| Patients included | 1103 | 503 | 1559 |
| Ventilated patients under continuous sedation, % | 81% | 77% | 73% |
| Number of days of sedation per 100 days of mechanical ventilation | 69 | 58 | 44 |
| Patients in which sedation was discontinued on a daily basis | n.r. | n.r. | 27% |
| Patients treated with benzodiazepines, % | 64% | n.r. | 73% |
| Number of days of treatment with benzodiazepines per 100 days of mechanical ventilation | 45 | n.r. | 36 |
| Patients treated with propofol, % | 50% | n.r. | 58% |
| Number of days of treatment with propofol per 100 days of mechanical ventilation | 22 | n.r. | 20 |
| Ventilated patients receiving analgesics through continuous perfusion, % | 47% | n.r. | 69% |
| Number of days of treatment with analgesics per 100 days of mechanical ventilation | 43 | n.r. | 44 |
| Delirium, % | n.r. | n.r. | 6% |
Unpublished data, personal communication of the VENTILA Group. Abbreviation: n.r.: not recorded.
In conclusion, Spanish Intensive Care Units and, especially, the healthcare staff working at such units, are already considered to be “human”. Nevertheless, an improvement in the units’ degree of comfort and the coordination with the patients’ family members in order to ensure an optimal stay in the case of patients who require our assistance is still required.22 To this end, we must rely on all professionals involved.
Please cite this article as: Arias-Rivera S, Sánchez-Sánchez MM. ¿Es necesario «humanizar» las Unidades de Cuidados Intensivos en España? Enferm Intensiva. 2017;28:1–3.