To determine the incidence and the factors associated with delirium in intensive care unit patients.
MethodsA cohort study conducted on 134 patients in the intensive care unit at a clinic in Bucaramanga, Colombia, who were recruited in the first 24h following admission and on whom the Richmond Agitation-Sedation Scale (RASS), PRE-DELIRIC version in Spanish, and Confusion Assessment method for Intensive Care Unit (CAM-ICU) were applied; the outcome was evaluated through daily monitoring with CAM-ICU.
ResultsThe incidence of delirium was 20.2%, the predominating type was hypoactive at 66.7%, followed by the hyperactive type at 7.4% and mixed at 25.9%. Fifty-two percent of the patients with delirium died. In the bivariate analysis, the use of sedatives (Relative Risk (RR) 2.4, 95% confidence interval (95% CI)=1.2–4.5), infection (RR=2.8, 95% CI=1.3–5.9), metabolic acidosis (RR=4.3, 95% CI=2.3–8.0), mechanical ventilation (RR=4.6, 95% CI=2.0–10.6), aged over 60 years (RR=2.3, 95% CI=1.09–5.3) and APACHE score greater than 14 (RR=3.0) (95% CI=1.1–8.2) were identified as risk factors for delirium. The multivariate analysis only found a relationship with infection (RR=3.8, 95% CI=1.6–9.1) and being aged over 60 years (RR=3.2, 95% CI 1.2–8.3).
Conclusionsdelirium is frequent in patients in the intensive care unit, especially the hypoactive type. Half of the patients with delirium died. The main risk factors for delirium are infection and being over 60 years age, therefore, delirium prevention activities should focus on these critical patients.
Determinar la incidencia y los factores asociados con delírium en pacientes de la Unidad de Cuidados Intensivos.
MétodosSe condujo un estudio de cohortes en 134 pacientes de la unidad de cuidados intensivos en una clínica de Bucaramanga, Colombia. Quienes fueron reclutados en las primeras 24h de ingreso y se les aplicaron las escalas de sedación y agitación de Richmond (RASS), PRE-DELIRIC versión en español y Confusion Assessment Method for Intensive Care Unit (CAM-ICU); el desenlace se evaluó a través de seguimiento diario con CAM-ICU.
ResultadosLa incidencia de delírium fue del 20,2%, predominando el de tipo hipoactivo 66,7%, seguido del hiperactivo 7,4% y mixto 25,9%. El 52% de los pacientes con delírium fallecieron. En el análisis bivariado, se identificaron como factores de riesgo para delírium, el uso de sedantes (riesgo relativo [RR] 2,4, intervalo de confianza del 95% [IC del 95%]=1,2-4,5), infección (RR=2,8, IC del 95%=1,3-5,9), acidosis metabólica (RR=4,3, IC del 95%=2,3-8), ventilación mecánica (RR=4,6, IC del 95%=2-10,6), edad mayor a 60 años (RR=2,3, IC del 95%=1,09-5,3) y puntaje APACHE mayor a 14 (RR=3, IC del 95%=1,1-8,2). En el análisis multivariado, solo se encontró relación con la infección (RR=3,8, IC del 95%=1,6-9,1) y la edad mayor a 60 años (RR=3,2, IC del 95%=1,2-8,3).
ConclusionesEl delírium es frecuente en los pacientes de la Unidad de Cuidado Intensivo, en especial el hipoactivo. La mitad de los pacientes con delírium fallecieron. Los principales factores de riesgo para delírium son infección y la edad mayor a 60 años, por lo tanto, las actividades de prevención de delírium deben ser enfocadas a estos pacientes críticos.
Delirium is associated with higher mortality, greater morbidity and with a lengthier hospital stay. It may be a predictor of long-term cognitive impairment in survivors.
What is the contribution of this?The use of the PRE-DELIRIC scale in its Spanish version is useful for early identification of risk factors. The results dictate the need for interventions focused on prevention and management. These interventions are currently at implementation stages.
Implications of the studyIn clinical practice nurses of the Intensive Care Units (ICUs) are able to carry out preventative actions on patients who are at greater risk of developing delirium, such as those over 60 years of age and those with infection.
From a teaching perspective, curriculums need to focus on tertiary prevention by designing programmes of nursing intervention focused on the prevention of this syndrome. With regard to investigation, the starting point would be to show through controlled clinical trials how effective nursing interventions focusing on the prevention of delirium are.
Delirium is known as an acute confusional syndrome1 or a neurobehavioural disorder characterised by an acute alteration in one's state of mind, which is fluctuating and with an abnormal attention span.2 This syndrome is frequently overlooked, due to the lack of appropriate screening and identification in the ICUs, rather than any erroneous diagnosis classifying it as any other disorder.3 Clinically delirium may be divided into hypoactive, hyperactive and mixed.4 the former is characterised by lethargy and reduced psychomotor activity. It is generally not acknowledged and its prognosis is worst as a result. The hyperactive form, where the patient is agitated and hypervigilant, usually does not go unnoticed and the last category is characterised by being a mix of the first two.5,6
The incidence of delirium fluctuates between 6% and 56% in older hospitalised adults, and is more frequent in those who are postoperative and those who are in a ICU,7 where patients are defined as people whose state of health is seriously compromised by a normal physiological alteration of the body putting the patient at a high risk of death, but as a non terminally ill patient there is the probability they will recover homeostasis and their life will continue.8
Regarding prevalence, the authors of cohort studies in clinical and surgical patients in the ICU have reported ranges between 20% and 80%. Despite the high prevalence, delirium is often not identified. This may be due to the similarity of symptoms with diseases such as dementia, depression or other syndromes, which results in an under diagnosis, particularly when delirium is hypoactive.1
The factors affecting the development of this cognitive impairment are divided into two: predisposing factors and precipitating factors. Within predisposing factors are: advanced age, male gender, prior dementia, cognitive impairment, a back ground of delirium, depression, anxiety, functional dependence, visual or auditive impairment, polymedication, psychotropic drugs, alcoholism, concomitant diseases and the gravity of them, dehydration and malnutrition. Precipitating factors are those which trigger the delirium and are modifiable, such as the administration of drugs (sedatives and hypnotic, narcotic, anticholinergic, etc.) or abstinence from drugs, sleep deprivation, environmental factors (stay in ICU, physical restraints, invasive devices, stress, multiple procedures, etc.), intercurrent diseases (infection and sepsis, metabolic alterations, hyperaemia/hypercapnia, pain, dehydration/undernourishment, iatrogenesis), surgery (orthopaedic, cardiac) and urinary or faecal retention.9,10
As a result, monitoring and diagnosis of delirium is regarded as an important component of daily evaluation of critically ill patients. This comprises 2 stages, the first of which contains neurological evaluation and is aimed at determining the level of consciousness-sedation of the patient through an objective evaluation. Sedation scales help to provide a common language for the multidisciplinary team in patient treatment goals. The Richmond Agitation-Sedation Scale (RASS) has been validated to differentiate between levels of sedation based on verbal and physical stimulation.11
The second stage consists of evaluation brain function, through the Confusion Assessment Method for Intensive Care Unit scale (CAM-ICU). This tool incorporates the 4 key areas which define delirium in accordance with the diagnostic and statistical manual of mental disorders (DEM-IV) of the American Association of Psychiatry, which are: (1) acute change or fluctuating course of mental state; (2) inattention; (3) disorganised thinking, and (4) altered level of consciousness. Delirium presents with a minimum of 2 points.11
The Pan American and Iberian Federation of Critical Medicine and Intensive Care Societies (FEPIMCTI) recommend using the CAM-ICU scale to assess delirium in all seriously ill patients who are not under profound sedation. Monitoring the presence of delirium is less invasive, less costly and potentially more sensitive than any other tool.12 According to Garrido et al.,13 delirium has been recognised as a common and serious problems in hospitalisation areas, but its diagnosis in critically ill patients is difficult due to the impossibility of interrogating the intubated patient and to the presence of sedatives. The high level of specialisation and invasive procedures means that the ICU is considered to be a stress-inducing area, which has linked it to the appearance of delirium in critically ill patients.
Delirium is associated with higher mortality in the short and long term, to greater morbidity and to an increase in the number of days in hospital.1 This is also linked to multiple complications and adverse results, including the patient removing tubes, removing catheters, lack of success in extubation, prolongation of stay in the intensive care units and increase in healthcare costs. Delirium may also be a predictor of long-term cognitive impairment in the survivors of critical diseases.14
Despite considering delirium as a frequent, avoidable problem with serious consequences for the critically ill patient, ICU healthcare staff do not use a tool for its assessment. Further educational training is therefore needed to disseminate the efficacy and usefulness of the scales for early, accurate diagnosis of delirium.15
One of these scales is the PRE-DELIRIC, which is able to predict the risk of the appearance of delirium in critically ill patients, the Spanish version of which was validated by Torres et al., who analysed the following factors: age, diagnostic group, emergency admission, use of morphine, use of sedatives, infection, coma, urea level, metabolic acidosis and the Acute Physiology and Chronic Health disease Classification System (APACHE II) score.16,17
Furthermore, the absence of early diagnostic protocols and timely intervention of this condition in the ICU has negative effects on the evolution and prognosis of the seriously ill patient.11 Healthcare staff therefore find themselves in a strategic situation to prevent delirium in patients at risk of it.
The aims of this study were to determine incidence, analyse the relationship between risk factors and the presence of delirium in patients of the intensive care unit, and also estimate the survival of patients with delirium.
Patients and methodsDesign. Qualitative, analytical cohort research study.
Area. The study was conducted in a multipurpose ICU of a clinic in Bucaramanga, Colombia. Data collection was made between February and July 2014.
Subjects. One hundred and twenty five patients from an ICU. Among the criteria for the calculation of the sample size we considered a confidence interval of 95% (95% CI), an expected frequency of 30% and 5% margin of error. Inclusion criteria for the patients were: over 18 years of age, full criteria for ICU stay, negative CAM-ICU and being within the first 24h of admission into the unit. Exclusion criteria were: RASS −4 and −5 scale of sedation, previous mental disorder, a background of alcoholism and the use of psychoactive substances. Patients were included incidentally when meeting this inclusion criteria.
Variables. The outcome variables were as follows: delirium, type and mortality and the covariables were: gender, older adult, origin, diagnostic group, and emergency admission, use of morphine, use of sedatives, infection, metabolic acidosis, mechanical ventilation, APACHE II score, hospital stay and the presence of coma.
Data collection. The patients were recruited during the first 24h of their admission into the ICU. The objective was explained to them and authorisation was requested through informed written consent by the patient, family member or accompanying person. Once their participation had been authorised, the RASS scale was administered (they had to score within a RASS −3 to +4). After this, assessment was made with CAM-ICU, and if this revealed a positive result for delirium the case was closed and the patient was excluded from the study. If a negative score resulted, daily follow-up of the patient was made with the CAM-ICU assessment until the patient presented with delirium, was discharged from the ICU to a hospital ward, or died. For assessment of risk factors in patients the PRE-DELIRIC scale in its Spanish version was applied.16
The tools used were:
- –
RASS scale. This shows significant qualitative concordance with a result of .87 for the expected .80 and quantitative concordance between markers measured by intraclass correlation of .97,18 and is a reliable way of assessing agitation and sedation of patients in the ICU. Agitation ranges from +1 to +4 and sedation levels from −1 to −5.17
- –
The PRE-DELIRIC model, which includes the following items: socio-demographic and clinical data evaluates whether the patient presented with an emergency admission to the ICU or not, the use of morphine during the stay in groups, the presence of infection, of coma, sedation with benzodiazepines and dose, level of urea, diagnosis of metabolic acidosis and APACHE II score. In the previous study16 validation of the scale in its Spanish version was made and the discriminatory capacity of the prediction model PRE-DELIRIC was determined to be good, given by the area under the ROC curve of 85.4% with 95% CI from 77.6% to 93.3%, i.e. it succeeded in appropriately predicting and classifying the outcome of delirium or no delirium in approximately 8–9 of every 10 patients.16
- –
The CAM-ICU is a practical instrument, with an appropriate internal consistency with a Cronbach alpha of .84, sensitivity of 83%, and specificity of 96%, and is valid and reliable for delirium diagnosis. The confusion of a critically ill patient in the ICU may be assessed. The following items are included: acute change, inattention, disorganised thinking and altered level of consciousness.19,20
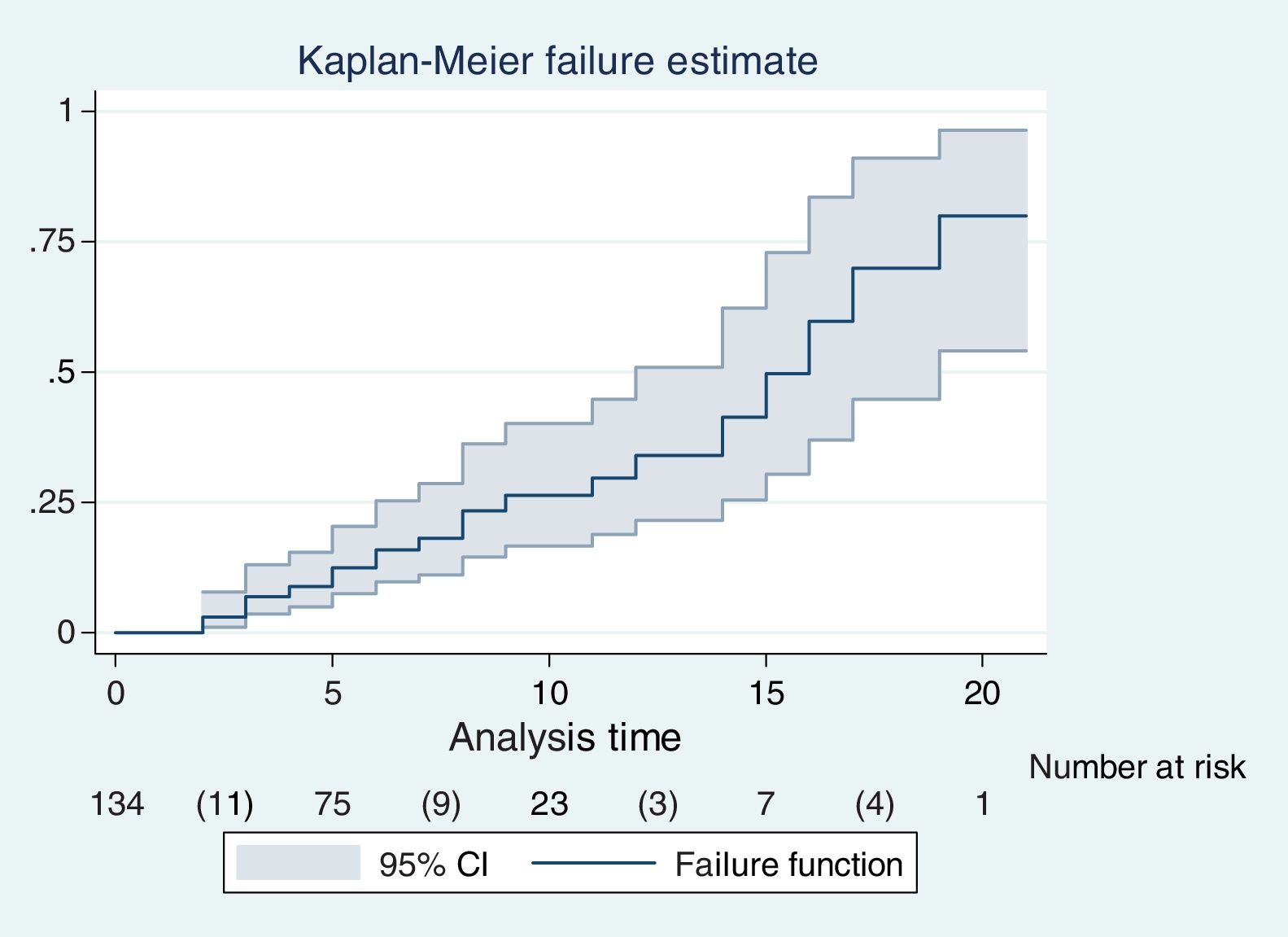
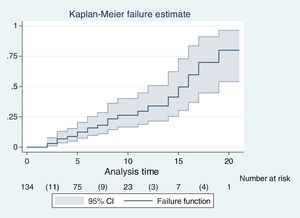
Data analysis. Regarding the tabulation plan and data analysis, the structure of the database in Epidata was designed,21 double digitation and information validation was made which was then exported to Stata22 for analysis. The description of the study variables was then made using frequency tables and percentages. Averages and medians were calculated for the continuous quantitative variables with normal and non normal distribution respectively. The rate or risk of delirium was estimated in ICU patients using the Kaplan–Meier method. The association between the explanatory variables with delirium through relative risks with their CI and χ2 tests were also calculated. After this a multivariate binomial regression model was conducted with the preselected variables of bivariate analysis with a p value of .20. A p value under .05 was considered statistically significant.
Our research took into account the regulations established by the Minister of Health of Colombia, in resolution 8430 of 4th October 1993,23 by which scientific, technical and administrative norms were established for health investigation. Furthermore, respect for dignity and the protection of the rights and well-being of the participants prevailed. In keeping with this resolution, this research was classified as minimal risk and participants’ informed consent was written. The ethical principles of beneficence, non-maleficence, autonomy and justice were respected. In addition, this research study was approved by the ethics committee of the University of Santander (UDES), and the ethics committee of the clinic where the information was collected.
ResultsOne hundred and sixty five patients were recruited, of whom 8 were excluded because they presented with delirium on admission to the UCI, 21 due to death and 2 due to persistent neurological impairment. These patients were considered lost as it was not possible to make assess final outcome and analysis was therefore concluded with 134 patients.
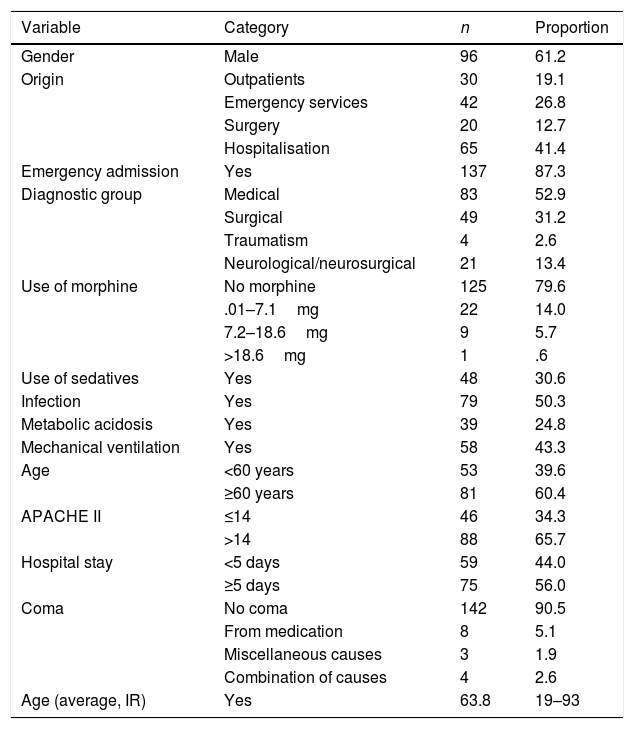
In Table 1 we may observe that the majority of patients were men (61.2%), the average age was 63.8, with a range between 19 and 93. Patients came from hospitalisation services (41.4%) and emergencies (26.8%). The prevalent diagnostic group was medical (52.9%); a high percentage of patients did not use morphine (79.6%) or sedatives or benzodiazepines (69.4%). Approximately half the patients had infection and mechanical ventilation, a quarter exhibited metabolic acidosis and over half were older adults, presenting with an APACHE score above 14, over 5 days of hospital stay and were not in a coma (90.5%).
Characteristics of the patients in the Intensive Care Unit of a clinic in Bucaramanga (n=134).
| Variable | Category | n | Proportion |
|---|---|---|---|
| Gender | Male | 96 | 61.2 |
| Origin | Outpatients | 30 | 19.1 |
| Emergency services | 42 | 26.8 | |
| Surgery | 20 | 12.7 | |
| Hospitalisation | 65 | 41.4 | |
| Emergency admission | Yes | 137 | 87.3 |
| Diagnostic group | Medical | 83 | 52.9 |
| Surgical | 49 | 31.2 | |
| Traumatism | 4 | 2.6 | |
| Neurological/neurosurgical | 21 | 13.4 | |
| Use of morphine | No morphine | 125 | 79.6 |
| .01–7.1mg | 22 | 14.0 | |
| 7.2–18.6mg | 9 | 5.7 | |
| >18.6mg | 1 | .6 | |
| Use of sedatives | Yes | 48 | 30.6 |
| Infection | Yes | 79 | 50.3 |
| Metabolic acidosis | Yes | 39 | 24.8 |
| Mechanical ventilation | Yes | 58 | 43.3 |
| Age | <60 years | 53 | 39.6 |
| ≥60 years | 81 | 60.4 | |
| APACHE II | ≤14 | 46 | 34.3 |
| >14 | 88 | 65.7 | |
| Hospital stay | <5 days | 59 | 44.0 |
| ≥5 days | 75 | 56.0 | |
| Coma | No coma | 142 | 90.5 |
| From medication | 8 | 5.1 | |
| Miscellaneous causes | 3 | 1.9 | |
| Combination of causes | 4 | 2.6 | |
| Age (average, IR) | Yes | 63.8 | 19–93 |
Proportion: %; IR: interquartile range.
However, of the 134 patients who completed follow-up, 27 presented with delirium according to the CAM-ICU delirium diagnosis tool, equivalent to an accumulated incidence of 20.2%. The median age of these patients was 72 years, with a range between 37 and 89. Furthermore, the average of days for developing delirium was 7.2, with a 95% CI of 7.1–9.2 days. Also, for patients with delirium, the hypoactive one was most predominant (66.7%), followed by the mixed (25.9%) and hyperactive (7.4%).
The average of follow-up days or stay in the ICU of patients was 5.8, with a range between 1 and 21 days. In addition to this, the total duration time in the ICU, i.e. the time the 134 patients were at risk of delirium was 815 days. Fig. 1 shows the risk of delirium each day of the participants’ stay in the ICU and risk of delirium on day five is observed at 13.7% and on day ten at 28.2%. After 16 days stay in the ICU, risk of delirium was 50%.
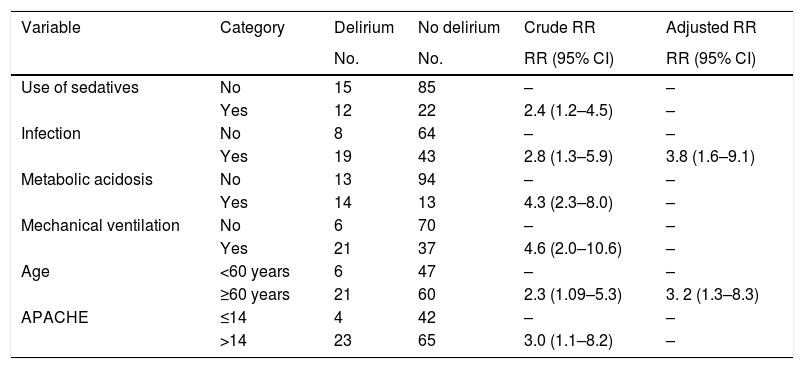
In bivariate analysis, the following risk factors were identified for the triggering of delirium: the use of sedatives: relative risk (RR) 2.4, 95% CI of 1.2–4.5; infection: RR 2.8, 95% CI of 1.3–5.9; metabolic acidosis: RR 4.3, 95% CI of 2.3–8.0; mechanical ventilation: RR 4.6, 95% CI of 2.0–10.6; age over 60 years: RR 2.3, 95% CI of 1.09–5.3, and APACHE score over 14: RR 3.0, 95% CI of 1.1–8.2. After this, in the multivariate binomial regression analysis only a relationship with infection (RR 3.8, 95% CI of 1.6–9.1) and age over 60 years (RR 3.2, 95% CI of 1.3–8.3) Table 2) was found.
Factors associated with delirium in patients from the Intensive Care Unit of a clinic in Bucaramanga, Colombia.
| Variable | Category | Delirium | No delirium | Crude RR | Adjusted RR |
|---|---|---|---|---|---|
| No. | No. | RR (95% CI) | RR (95% CI) | ||
| Use of sedatives | No | 15 | 85 | – | – |
| Yes | 12 | 22 | 2.4 (1.2–4.5) | – | |
| Infection | No | 8 | 64 | – | – |
| Yes | 19 | 43 | 2.8 (1.3–5.9) | 3.8 (1.6–9.1) | |
| Metabolic acidosis | No | 13 | 94 | – | – |
| Yes | 14 | 13 | 4.3 (2.3–8.0) | – | |
| Mechanical ventilation | No | 6 | 70 | – | – |
| Yes | 21 | 37 | 4.6 (2.0–10.6) | – | |
| Age | <60 years | 6 | 47 | – | – |
| ≥60 years | 21 | 60 | 2.3 (1.09–5.3) | 3. 2 (1.3–8.3) | |
| APACHE | ≤14 | 4 | 42 | – | – |
| >14 | 23 | 65 | 3.0 (1.1–8.2) | – |
95% CI: 95% confidence level; RR: relative risk.
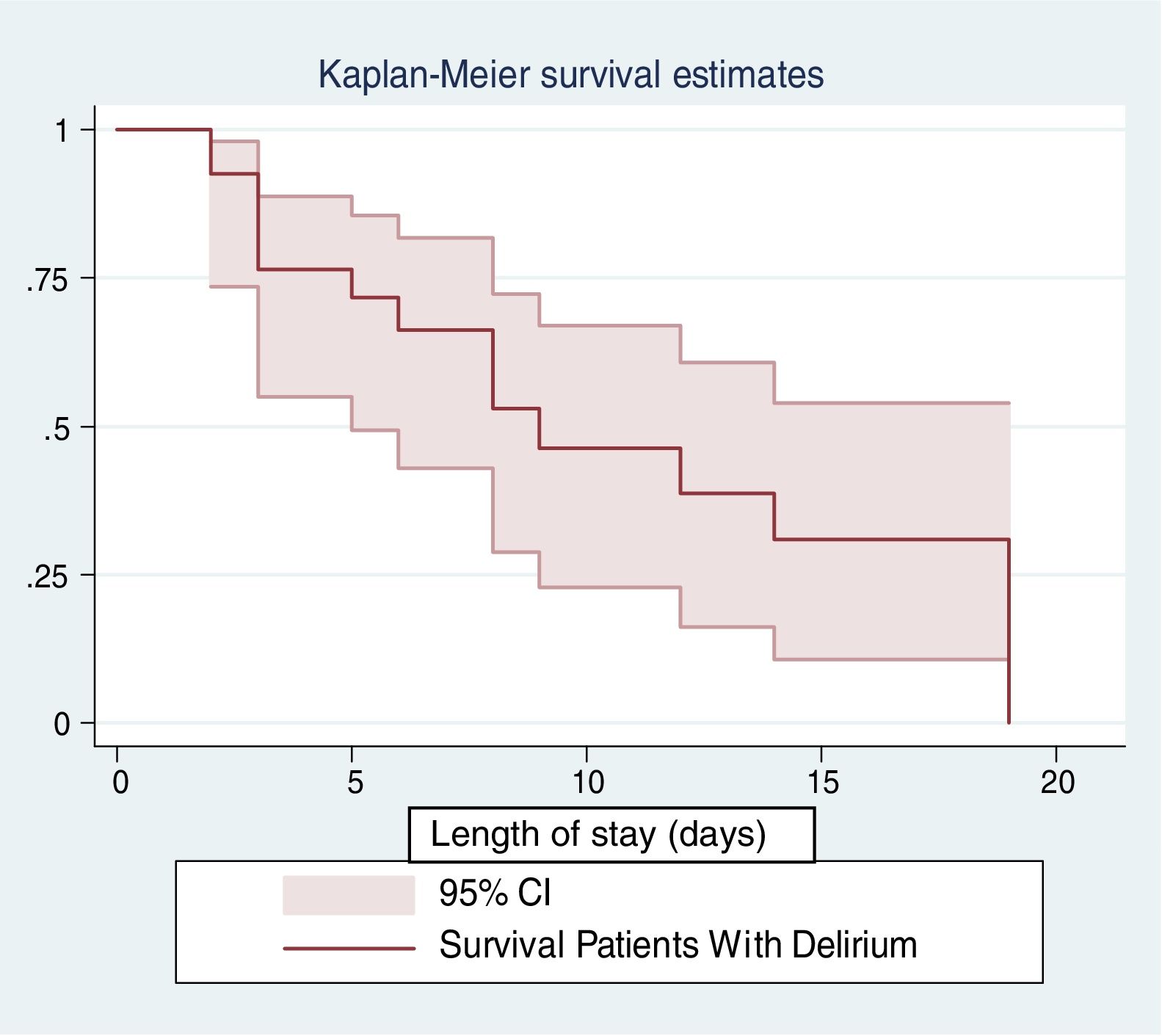
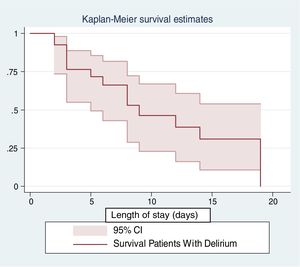
Fourteen of the 27 patients with delirium died, a frequency of 51.85%. Furthermore, after 10 days of hospital stay the survival of patients with delirium was 50%, i.e. that approximately one out of every 2 patients with delirium died by the tenth day in the ICU (Fig. 2). Mortality according to delirium type was 55.6% for hypoactive delirium, 57.1% for mixed delirium and 0% for hyperactive delirium. These findings are descriptive, i.e. they were not adjusted by other covariables as this was not the main aim of the study.
DiscussionA similar incidence of delirium was reported in other studies such as that by Wassenaar et al.,24 where the reported incidence was 23.6%, and that of Carrillo and Sosa11 with 21.8%. This ranged between 20% and 80%, depending on the population characteristics. In this study the most prevalent was hypoactive delirium, with the most common being that in persons over 60 years of age, as has been similarly reported in other studies.25,26 Other research studies have revealed much higher incidences. Ely et al.27 reported an incidence of 81.3% of delirium in patients during their stay in the ICU and Garrido et al.1,3 reported incidences of 41.3%.
With regard to hospital stay, we observed that on average the patients developed delirium after 7 days, with a greater risk of its progression as their stay in the ICU increased. Prior to this Ely et al.,25 reported that the majority of patients developed delirium in the ICU and hospital stay length was the strongest predictor.
The figures above show that, despite the efforts made some years ago for an early diagnosis of this syndrome, diagnosis still goes unnoticed or the syndrome is under diagnosed, which prevents the right intervention to prevent persistent cognitive impairment after hospital discharge and reduce the risk of associated morbidity.6 In addition to this other major aspects are the costs generated for the healthcare system. In some studies the impact on healthcare costs has been reported. This includes more days in the ICU and more days on mechanical ventilation, where resources used to care for this type of patient are considerably higher.28,29
Regarding bivariate analysis a statistically significant relationship between the variables of sedative usage, infection, metabolic acidosis, mechanical ventilation, patients over 60 and an APACHE II score higher than 14 was found. The incidence of delirium was made through the calculation of relative risks, i.e. that a differential behaviour of delirium exists with its risk being higher when the patient presents with these conditions. This is similar to data reported in another study in Colombia, where a higher relationship was found regarding age (63.5±16.8 years), length of stay (8.82±18.7 days) and mechanical ventilation (34.67%), but different with regard to that found with the use of benzodiazepines (27.83%) and analgesics (50.6%).30
With regard to multivariate analysis, in this research the risk of delirium increased 3.8 times in the presence of infection and 3.2 times in adults over 60 years of age. Similarly to the findings in the study by Lin et al.,29 in which it was shown that the risk of developing delirium increases in patients with mechanical ventilation and infection. Moreover, age is still an important factor in the presence and development of delirium, which is consistent with that reported in other studies, where it is shown that a predisposing factor for presenting with delirium is advanced age.5,24
In a similar manner, shock was analysed as a predictor factor of the presence of delirium.29 In this research study, the presence of metabolic acidosis in the patients was a differential factor in the development of delirium, and was related to both the presence of sepsis and septic shock, as well as other types of infection in the critical patient.
With regard to mortality, in this study we observed through the Kaplan–Meier descriptive survival analysis that approximately half of the critical patients with delirium die, a fact that is very similar to that reported by other authors5,25,31 who have studied this phenomenon. For example, Restrepo et al.32 identified that 13.8% of patients with delirium died during hospitalisation, and it was therefore concluded that delirium is a frequent clinical condition related to lengthier hospital stay and raised mortality.28 Furthermore, Lin et al.28 found that delirium is a separate predictor of the increase in mortality among patients on mechanical ventilation. In another study29 it was found that the patients with delirium were more likely to die in the ICU (p<.005). In other words, delirium increased mortality in all patients (p=.0022) after making an adjustments for age and the APACHE II score.
Based on results there is clearly a need for interventions focused on prevention and its management, with delirium being clearly a pathological condition characterised by a reversible disorder, but which leads to physiological and psychological alterations that influence patient outcome.33,34
One study limitation was the follow-up time of the population studied. This was prolonged in patients with neurological impairment or high levels of sedation. In cases where follow-up could be resumed, a final result was achieved and in contrary cases these patients were considered to be lost to the study.
The results of this study will enable the research team to suggest interdisciplinary interventions to prevent, diagnose and treat delirium in order to improve safety, reduce care costs and optimise patient outcome.
ConclusionsThe incidence of delirium in ICU patients of a clinic of Bucaramanga was 20.15% and the incidence rate was 3.2 per 1000 days-patients. Hypoactive delirium was the most predominant in the patients. A statistically significant relationship was found between age and infection with the development of delirium. Mortality of patients with delirium was 51.95%.
FinundingThis project was approved and financed at the internal 2013–2014 meeting of the University of Santander with Code 007-13.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Torres-Contreras CC, Páez-Esteban AN, Hinestrosa-Díaz del Castillo A, Rincón-Romero MK, Amaris-Vega A, Martínez-Patiño JP. Factores asociados con el delírium en pacientes críticos de una institución de salud de Bucaramanga, Colombia. Enferm Intensiva. 2019;30:13–20.