In most countries worldwide, general adult psychiatrists look after the mental health of adults with intellectual disabilities (ID) without appropriate specialist training in the field. It is, therefore, necessary to develop a practice guideline to help these clinicians to assess and diagnose psychiatric disorders in adults with ID.
MethodsWe have developed an evidence and consensus-based practice guideline for the assessment and diagnosis of major functional psychiatric disorders in adults with ID. Several senior psychiatrists from different European countries formed a guideline development group who assessed the evidence gathered from a systematic literature search to produce the guideline.
ResultsAdults with ID develop the same psychiatric disorders as their non-ID counterparts. The overall rate of major functional psychiatric disorders such as schizophrenia, depressive disorder, bipolar disorder, and anxiety disorders seems to be somewhere between 14.4-22.4%. However, if a wider definition of psychopathology and mental ill-health is considered including depressive and anxiety symptoms, behaviours of concern, and other neurodevelopmental disorders such as autism spectrum disorder the rate becomes much higher than that in the general population. The risk factors for psychiatric disorders seem similar in both the ID and the non-ID populations. However certain risk factors such as genetic burden, certain comorbidities, psychosocial adversities, and reduced coping capacity are more prevalent among adults with ID.
ConclusionThis guideline describes how the main symptoms of major psychiatric disorders may manifest differently in adults with ID and provides recommendations as to how to address these issues in day-to-day clinical practice.
The historical notion that adults with intellectual disabilities (ID) have underdeveloped intellect and emotion and, therefore, are protected from emotional and cognitive stress and as a result, do not develop psychiatric disorders has been challenged in the last four decades. It is now well recognized that adults with ID suffer from the same range of psychiatric disorders as their counterparts in the general adult population who do not have ID. However, the prevalence rates of psychiatric disorders in adults with ID vary widely among studies for several reasons, which are discussed in the following sections.
Prevalence studiesThe first problem is with the definition of psychiatric disorders. In many prevalence studies, problem (challenging) behaviour (behaviour that challenges or behaviour of concern) is included as a type of psychiatric disorder. This inflated the prevalence rate. However, this notion of defining problem behaviour as a psychiatric disorder is now challenged and no major psychiatric classification system defines problem behaviour as a psychiatric disorder in adults. As a result, more recent prevalence studies excluded problem behaviour from the definition of psychiatric disorders.
Disorders like autism spectrum disorder (ASD) and attention deficit hyperactivity disorder (ADHD) were included in previous prevalence studies as psychiatric disorders. However, in the recent classification systems such as the DSM-51 and proposed ICD-11,2 these disorders are categorised like ID under the broader diagnostic category of neurodevelopmental disorders (NDDs). However, to confuse the matter further, both ASD and ADHD are common comorbidities of ID, and both ASD and ADHD are shown to be associated with increased psychopathology.
For example, a recent European study of 151 adults with ID who were recruited from care homes, rehabilitation centres and from people attending psychiatry outpatients for the first time has reported a psychiatric diagnosis among 63.5% of the participants. However, the diagnosis included 34% with problem behaviour, 13.9% ASD, and 10.6% ADHD.3 Similarly, in Cooper and colleagues’ study4 when problem behaviour and ASD were included, the overall rate of mental ill-health (psychopathology) was reported to be 40.9% among 1023 adults with ID as per the clinician's diagnosis. However, when the diagnoses of problem behaviour and ASD were excluded, the prevalence rate of psychiatric disorders came down to 22.4%. This is supported by Deb and colleagues’ study5 in which they reported an overall rate of ICD-106 psychiatric diagnosis among 90 adults with ID who had sufficient communication ability as 14.4% compared with 16% in the non-ID general population.7 This study excluded the diagnosis of problem behaviour, ASD, and ADHD. Therefore, it appears that if ICD-106 criteria are used and diagnosis of problem behaviour and ASD are excluded, the overall rate of functional psychiatric disorders in adults with ID remains somewhere between 14.4-22.4%.4,5
Diagnostic criteriaThe second problem is to find a diagnostic instrument that could be used for adults with all levels of severity of ID. For example, the standard diagnostic criteria used for diagnosis of psychiatric disorders in the non-ID general population may be used for adults with mild ID and perhaps with some adaptation for adults with moderate ID but are almost impossible to use in adults with severe and profound ID.8 The prevalence rate also varies depending on the diagnostic criteria used. For example, in Cooper and colleagues’ study4 the rates of psychiatric disorder excluding problem behaviour and ASD were reported to be 22.4%, 19.1%, 14.5%, and 13.9% using a psychiatrist's clinical diagnosis, DC-LD (Diagnostic Criteria-Learning Disability),9 ICD-10-DCR (International Classification of Diseases-10th edition-Diagnostic Criteria for Research)6 and DSM-IV-TR (Diagnostic and Statistical Manual-4th revision-Text Revised) criteria respectively.10
Standard diagnostic criteria used for the non-ID general population have therefore been adapted for use in the ID population. For example, DC-LD9 was adapted from ICD-106 criteria for use in the ID population. Similarly, for use in the ID population, DM-ID (Diagnostic Manual-Intellectual Disability)11 was adapted from DSM-IV-TR criteria10 and DM-ID-2 (Diagnostic Manual-Intellectual Disability-2nd revision)8 from DSM-V criteria.1
Sample selectionThe third problem is with the sample selection. In the old prevalence studies, samples comprised institutionalised adults with ID. More recent studies included both hospitalised and community-based populations. Even in the community, it is difficult to detect all adults with ID, particularly those who have a mild ID or borderline intelligence. As a result, the prevalence rate could not be established for the whole population of adults with ID. Instead, those adults who are usually known to the services or those who are attending outpatient clinics have been included in the prevalence studies, providing a potentially higher rate of psychiatric disorders in this population. Therefore, it is difficult to establish true epidemiological prevalence figures for psychiatric disorders in this population.
Definition of psychiatric disorders and diagnostic instrumentsSome psychiatric disorders, on the other hand, remain undetected in this population. For example, it is known that in the non-ID general population, many patients with depressive disorder or even a mild form of bipolar disorder are not known to the services. A similar problem lies with the detection of these psychiatric disorders in adults with ID, particularly in those with mild ID who are living independently in the community.
Another problem is the distinction between psychiatric symptoms and psychiatric syndromes. For example, many psychiatric symptoms such as depression and anxiety are more common in the population than major depressive disorder and generalised anxiety disorder as psychiatric syndromes. Some studies reported rates of psychiatric symptoms rather than syndromes thus inflating the prevalence rate. A related problem is the use of many different instruments in different studies to diagnose psychiatric disorders in adults with ID. In particular, the studies that used a screening instrument such as Psychiatric Assessment Schedule for Adults with Developmental Disabilities (PAS-ADD) checklist12,13 are likely to report a higher rate of psychiatric disorders in this population than the studies that used the full diagnostic schedule like the full PAS-ADD interview.14
ObjectivesThe possibility of people with ID suffering from several psychiatric disorders is a major public health concern. Therefore, better management of these issues is of utmost importance to improve the quality of life of these people and their family caregivers. However, better management is only possible when a better understanding of these issues is realised. As most psychiatrists in Europe and worldwide have very little training in assessing and diagnosing mental disorders in people with ID, it is of paramount importance to develop a guideline to help with their clinical practice. Given the poor quality of evidence in this area, it is necessary to review and update the literature and develop an updated guideline. Therefore, we have developed this European guideline based on updated evidence and consensus. This guideline is an update of a previously published European guideline15 by the European Association of Mental Health in Intellectual Disabilities. In the current guideline, we have concentrated on issues relating to adults with ID as issues related to children and adolescents with ID are different from those of adults with ID. As in most countries in the world, general adult psychiatrists are expected to look after the mental health of adults with ID without any specific training in this area, we envisage this guideline will be particularly helpful to them.
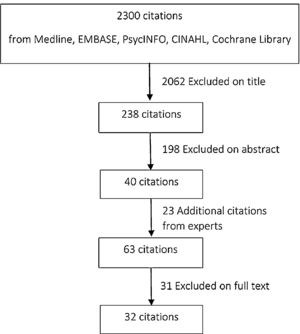
The European GuidelineMethodThis guideline followed standardised guideline development criteria recommended by the National Institute for Health and Care Excellence (NICE), UK (www.nice.org). In brief, we carried out a systematic literature search using the search terms presented in Appendix 1 (supplementary material) using databases Medline, EMBASE, PsycINFO, CINAHL, and Cochrane library (see Fig. 1). Each database was searched between January 2000 to August 2020. In addition, websites of relevant professional bodies such as NICE, UK, Royal College of Psychiatrists (RCPsych), UK, World Psychiatric Association (WPA), European Psychiatric Association (EPA), International Association of Scientific Studies in Intellectual and Developmental Disabilities (IASSIDD), and European Association of Mental Health in Intellectual Disability (EAMHID) were reviewed. Furthermore, suggestions for the inclusion of articles were sought from several experts in the field. Two authors (BP and MO) independently screened records using pre-determined inclusion and exclusion criteria. Any discrepancy was resolved through discussion or arbitration by a third author (SD). One author extracted data from the selected articles using a standardised proforma adapted from the Cochrane library guide.16 Evidence was categorised using standardised methodology17 (see Table 1). Findings are reported using a narrative synthesis of information from included studies. Additionally, using Scottish Intercollegiate Guidelines Network (SIGN) 50 checklist (http://www.sign.ac.uk/methodology/checklists.html), 32 individual studies were rated as overall ‘high quality’ or ‘acceptable.’ The quality of eligible studies was assessed during the data extraction.
Gradation of evidence17.
Evidence was scrutinised by four authors (SD, BP, KK, and MO) and recommendations for clinical practice were made using a standardised method of categorisation (see Table 2).18 This information was further discussed and agreed with the whole guideline development group members which consisted of eight psychiatrists from various European countries, namely Poland (Krysta), Germany (Sappok), UK (Deb, Perera, Ozer), Italy (Bertelli), the Netherlands (Wieland) and Spain (Novell).
Grading of recommendations18
Any studies that described psychopathology including psychiatric disorders in adults with intellectual disabilities.
Exclusion criteriaStudies on both pharmacological and non-pharmacological interventions, single case studies, studies on children, and exclusively on challenging behaviour without any specific data on psychiatric disorders.
ResultsA total of 2300 citations were retrieved initially. Using eligibility criteria 32 articles were ultimately selected for inclusion (see Fig. 1). The findings of these articles are summarised in Appendix 2 (supplementary material) (references to the studies on dementia, eating disorders, personality disorders, and sleep disorders are removed from the revised version of the manuscript). All the excluded studies were on interventions either pharmacological or non-pharmacological (psychosocial). For all studies, evidence grades were assigned as per recommendations in Table 1. Most studies reached evidence level I or II. Five are level I evidence (five systematic reviews including one meta-analysis), 16 are level II evidence, and 11 are level III evidence. There are five expert reviews in journals and 11 expert reviews in book chapters. There are nine cross-sectional cohort studies, one prospective cohort study, and one case series. Most studies (n = 22) were classed as high quality and ten as acceptable according to the SIGN overall ratings. Three recommendations are at level B, four at level C, and one at level D. The recommendations primarily involved the description of differential manifestation of symptoms in people with ID to aid clinical assessment and diagnosis of the main functional psychiatric disorders, (a) schizophrenia, (b) major depressive disorder, (c) bipolar disorder, and (d) anxiety disorders.
Aetiology/ risk factorsCertain risk factors for psychiatric disorders like genetics and environment are similar in both ID and non-ID general populations. However certain factors such as genetic burden, comorbid physical and psychological/behavioural problems and NDDs, psychosocial adversities including life events, and reduced coping capacity are more prevalent among adults with ID (see Table 3). Chronic stress, psychosocial stressors, stigma, loss, negative life events, chronic physical illness, low self-esteem are all common risk factors for psychiatric disorders in the ID and the non-ID population alike. Sleep problems could be both a symptom as well as a cause of psychiatric disorders in both ID and non-ID populations. Sensory impairment may be an important risk factor for psychiatric disorders specifically in adults with ID. Although epilepsy is common in adults with ID19 and psychopathology may be observed during the peri-ictal phase of epileptic seizures, their relationship with inter-ictal psychopathology in ID is less clear.20 The underlying brain damage in the case of severe/ profound ID and negative psychosocial impacts in the case of mild/ moderate ID are likely to be stronger determinants of psychopathology than epilepsy per se.21
The risk factors for psychiatric disorders in adults with intellectual disabilities.
The relationship between age, gender, the severity of ID, and the rate of psychiatric disorders is not clear.22 Some have shown an increase in the rate of psychiatric disorders with increasing age. Apart from dementia other functional psychiatric disorders may not be related to age in adults with ID. Some showed an increase in psychiatric disorders in adults with more severe ID. However, this finding will have to be interpreted with caution because of the unreliability of making a diagnosis of psychiatric disorder in adults with severe and profound ID.
ASD is common in adults with ID and ASD itself is associated with increased psychopathology particularly psychotic disorders, anxiety, and also problem behaviour. One meta-analysis found23 the overall rate of psychiatric disorders among 54.8% of adults with ASD in the general population. Schizophrenia was prevalent among 11.8%, affective disorder 18.8%, anxiety disorders 17.8%, and ADHD in 25.7% of adults with ASD. However, the relationship between ID, ASD, and psychopathology is complex. Both ID and ASD on their own could mimic symptoms of psychiatric disorders and disentangling this could be impossible in many cases.24 The use of psychotropic medication, particularly antipsychotics is common among adults with ID which could precipitate psychiatric symptoms through their side effects.25 Genetics may play an important part in predisposing psychiatric disorders in adults with ID. For example, a European study of the largest ever sample (n = 100) found a high rate of pathogenic copy number variants (13%) among people with ID who had co-morbid psychiatric disorders.26,27
AssessmentRecommendation (D)It is important to make reasonable adjustments (allow more time than usual, use appropriate communicative aids including pictures and sign languages) to ensure the proper assessment of the mental state of an adult with ID. The assessment should include history taking (see Table 4), mental state examination (see Table 5), physical examination, and relevant investigations. It is important not to accept historical diagnoses made many years ago without a challenge.
History taking in an adult with intellectual disabilities.
Mental state examination of an adult with intellectual disabilities.
The interview setting may need to be adjusted. For example, interviews can occur in a wide variety of settings (e.g., the person's home, a day centre, an outpatient clinic, and so on). As much as possible, the adult with ID should be seen in a surrounding that is familiar to her/him. There should be flexibility in the choice of the setting for assessment. A clinician may need to see the adult with ID in different settings as certain psychopathology may manifest in certain environments/ situations, not in others. It is helpful if the assessor is familiar with the adult with ID. Where family or caregivers attend with the adult with ID, they should know the person well and have a good relationship with them. Issues about confidentiality need to be borne in mind (e.g., the adult with ID may wish the caregiver not to be present during the interview). There should be flexibility in the length of the interview (e.g., several shorter interviews instead of a long interview). It is important to gather information from as many sources as possible such as the person with ID, their family members, support staff, other professionals such as the teachers and the nurses etc. (including written records).
Special issues concerning psychiatric diagnosis in adults with IDRecommendation (B)As psychiatric disorders are often difficult to diagnose in adults with ID, particularly in those who have a severe and profound ID, both a false positive and a false negative diagnosis are possible. In the case of a false-positive diagnosis, problem behaviour may be mistaken or misclassified as a psychiatric disorder. In the case of a false negative diagnosis, a psychiatric disorder is not made either because the symptoms are thought to be part of the ID phenotype (diagnostic overshadowing)28 or maybe simply the symptoms are diagnosed as problem behaviours instead. Indeed, many signs and symptoms which are common in psychiatric disorders, such as social withdrawal, excessive agitation, lack of concentration, stereotyped movement disorders, sleep problems, and certain other behaviours can be found in adults with ID who do not have a psychiatric disorder.
It is, therefore, important to compare the mental state of the person before the onset of the suspected psychiatric disorder with the current one. Therefore, if any of the pre-existing behaviours or symptoms mentioned in the previous section shows a further deterioration, for example, sleep problem or agitation gets worse, this may indicate the start of a psychiatric disorder (baseline exaggeration).29
The psychiatric disorder may manifest as problem behaviours in adults with ID but not all psychiatric disorders will lead to problem behaviours. Similarly, not all problem behaviours are due to a psychiatric disorder as there are many reasons for challenging behaviours.30-33
Assessment instrumentsSeveral instruments are available to assess psychopathology in adults with ID.34 For adults with ID who can communicate their thoughts a structured interview like PAS-ADD,12 or Assessment of Dual Diagnosis (ADD) can be used.35 For adults with more severe ID an instrument like the Diagnostic Assessment for the Severely Handicapped-Revised (DASH II) can be used.36 It is outside the remit of this paper to provide a full account of all instruments available for the assessment of psychopathology in adults with ID. However, a comprehensive list of instruments used in the assessment of psychopathology in adults with ID is presented in Appendix 4 (supplementary material).
Functional psychiatric disordersSchizophreniaSchizophrenia is characterized by the presence of (a) delusions, (b) hallucinations, (c) disorganized thinking (speech), (d) abnormal motor behaviour including catatonia, and (e) negative symptoms.1
Schizophrenia is more common in adults with ID than those who do not have ID. Point prevalence in adults with ID has been reported to be between 3.4% and 4.4%4,5 compared with 1% in the non-ID general population.7 This higher rate could be explained by shared etiopathology both genetics and environmental. For example, a higher rate of schizophrenia is associated with certain genetic syndromes such as Velocardiofacial (22q11.2 deletion) syndrome which is also associated with ID.37 Similarly, many environmental factors such as obstetric complications are common etiological factors for both schizophrenia and NDDs in general and ID in particular.38,39
Recommendation (C)The diagnosis of schizophrenia in adults with ID is based on the presence of several complex subjective symptoms (delusions, hallucinations, abnormal thoughts, etc.), and thus a certain level of communicative ability is needed to describe such symptoms to an interviewer. It is, therefore, difficult for people who lack communication skills to describe their thoughts and feelings which may be the case for many adults with ID. It may, therefore, be impossible to diagnose schizophrenia in some people with ID particularly those who are at the severe and profound end of the spectrum. There may be several reasons for this. For example, the neuronal networks necessary for the production of psychotic symptoms may be damaged or may not exist in adults with severe and profound ID. It is not possible to assess reality testing reliably in adults with severe and profound ID. There are no valid tools available to diagnose schizophrenia in adults with severe and profound ID. However, every attempt should be made to communicate with the person with ID, if necessary making reasonable adjustments such as allowing more time for interviews, using pictures and sign languages etc., and using communication partners (https://spectrom.wixsite.com/project).
DelusionsTo elicit paranoid delusions the person may be asked whether they feel someone is trying to harm them or plotting against them.14 It is, however, possible for an adult with ID to think that someone is trying to harm them if they do not get on with a support staff (paid caregiver) or a relative, or one of their peers. Similarly, an adult with ID may feel that they are controlled by support staff as they may not have much control over their own routine and activities. For example, if suffering from a persecutory delusion, a person with ID may avoid a certain person or hide in their presence or get upset but the same may happen if the person is simply afraid of that person for some reason but is not experiencing any delusion.
It is important to distinguish between ‘psychotic-like’ symptoms from true ‘psychotic’ symptoms in adults with ID. Certain types of ‘fantasy thinking’ can be part of the ASD phenotype. This is characterized by a pretend mode of thinking like an inner world that is disconnected from the outside. As such, the interpretation of a situation is unrelated to the reality of other people. However, it is also important to recognise that adults with ASD may show genuine psychotic symptoms, and in fact, psychosis is shown to be a common association of ASD.23,24 Given that ASD is common in ID, this makes the picture very complex indeed, in terms of deciding whether some of these symptoms are part of psychosis or ID or ASD.
Psychotic-like behaviours such as talking to oneself, regression, and abnormal postures, for example, in response to stressful events, can be part of symptoms of ID with or without ASD.22,40-42 Unique ways of experiencing the world in ASD and some consequent symptoms, such as a bizarre expression or fantasy thinking related to impaired emotional development, may be mistaken as psychotic symptoms.24,40,43
HallucinationsIt is possible that instead of auditory hallucinations, visual hallucinations can be the presenting symptoms of schizophrenia in adults with ID. This is consistent with the finding that visual hallucination is more common in organic psychosis when associated with illicit drug use or epilepsy or brain tumour and most adults with ID are likely to have some underlying brain impairment.44-46 A person with ID who is experiencing visual hallucination may cover their eyes to avoid the image, but this behaviour has to be distinguished from covering of eyes done by many people with autistic trend who are hypersensitive to light.47 Other hallucinatory behaviours in adults with ID may include suddenly turning towards or away from a sound source (auditory hallucinations), moving gaze (visual hallucinations), making gestures as if to remove something from the skin or body (tactile hallucinations), sniffing the air intensely to check for unusual smell (olfactory hallucinations), wearing heavy, tight-fitting clothes or dressing with many layers of clothing (proprioceptive hallucination).48 The latter has to be distinguished from certain symptoms of ASD such as impaired proprioceptive stimulation and problems with decision making.47
Adults with ID may experience what is known as ‘pseudo hallucination’ instead of a true hallucination.49 In true hallucination, the person will think that the voice is originating from within their own head but in pseudo hallucination, they may think that the voice is coming from outside their body. Some unusual experiences during focal seizures particularly during the peri-ictal phase have to be distinguished in adults with ID from symptoms of schizophrenia, although post-ictal psychosis also remains a possibility.20,24
Some adults with ID may look as if they are hallucinating when they speak to themselves, speak or look at an imaginary person, speak to an object such as a tree or a table. These behaviours could be indirect evidence of hallucination, but these behaviours could also be part of the person's long-standing abnormal behavioural repertoire or part of the ASD phenotype.24 In the absence of other diagnostic features, a diagnosis of schizophrenia should not be made in an adult with ID only based on these possible indirect features of hallucinations.
Affective (including negative) symptomsIn the acute phase, the person may show incongruent mood (laughing when the person should be feeling sad or crying when the person should be feeling happy) and labile mood showing a lot of ups and downs in affect. Anxiety is often a presenting feature in the acute phase. In the chronic phase, however, the mood tends to become either flattened or depressed (so-called negative symptoms). Both anxiety and depressed mood could also be precipitated by the antipsychotic medications that are used to treat schizophrenia. Antipsychotics are also commonly used to manage problem behaviours in adults with ID and up to 24% of adults with ID may receive antipsychotics50 as opposed to less than 1% in the non-ID general population.51 However, negative symptoms may remain undetected in adults with ID because of the diagnostic overshadowing.52,28
Abnormal behaviour including catatoniaIn the acute stage bizarre behaviour, excessive agitation, aggression, and self-harm may be present. The person may act under the influence of their delusions or hallucinations. These features, along with stereotyped movement disorders should be distinguished from the similar features that are associated with ASD and other NDDs. Antipsychotic medications may cause both agitation (akathisia) and negative symptoms.
Odd postures and slowness are common in catatonia which could be seen in patients with schizophrenia. The disorder needs to be differentiated from movement disorders, adverse effects of medication (especially antipsychotics),53 autistic-like regression in adults with Down syndrome,54 and bizarre movements sometimes seen in adults with ID. Also, worth remembering that catatonic features mimicking similar symptoms are common in many adults with ASD.23
Disorganized thinking (speech)This is often difficult to detect in many adults with ID because of their underlying communication difficulties. Their disorganised thoughts may manifest as anxiety and problem behaviour. Sometimes this may manifest as disorganised and odd behaviours with or without accompanying disorganised speech.55 Disorganised speech and behaviour may also be observed during the peri-ictal phase of an epileptic seizure.20
There are now online resources available in an accessible format on psychosis in people with ID (https://peterbates.org.uk/home/linking-disabled-people-and-communities/easy-read-information-about-mental-health/easy-read-information-explaining-about-mental-health-issues/).
Major Depressive disorderDepressive symptoms could be present in up to 16.5% of adults with ID but a diagnosis of a major depressive disorder has been reported among 2.2%-8% of adults with ID,4,5,56 which compares with a 2.1% point-prevalence and 7% 12-months prevalence rate in the non-ID general population.7,1
Recommendation (B)It is important to explore the causes of depression, such as physical illness (hypothyroidism, which is common in Down syndrome, cancer, infection, etc.),57 prescribed medication (especially antipsychotics), certain genetic disorders associated with the ID,58,59 and environmental factors that could perpetuate the problem (for example, ongoing conflicts with another resident at home). Dementia may have a similar initial presentation.60
Although self-neglect and self-harm may be prominent features of depression, in people with ID self-injurious behaviour may not always be associated with depression. There are other important genetic (for example, Lesch Nyhan syndrome)61-63 and environmental factors (lack of stimulation in the immediate environment) related to self-injurious behaviour in adults with ID.62,63 Anxiety is a commonly associated symptom of depressive disorder in the non-ID general population. However, in the case of adults with ID, anxiety may manifest as a problem behaviour. On the other hand, anxiety is a common symptom associated with ASD and ASD is common in ID, so anxiety symptoms are common in adults with ID even without the presence of a depressive disorder.
Like in the non-ID general population, psychosocial stressors, negative life events, abuse (past and present-physical, sexual, and other types) and other psychological trauma, loss, chronic physical illness, loneliness, low self-esteem, stigma are all important risk factors for depression in adults with ID.64 Support including family support, on the other hand, maybe a protective factor for depressive symptoms.65
Recommendation (C)The following recommendations are made for the assessment and diagnosis of major depressive disorder in adults with ID.
Assessment should include a physical examination and appropriate investigations such as thyroid function, full blood count, serum iron, and vitamin levels. Physical causes such as chronic pain/discomfort in the body should be excluded. A detailed medication history (antipsychotics, antihypertensives, steroids, etc.) should be acquired, including an assessment of adverse effects of medications (including antidepressants and antipsychotics). Assessment for other causes of depression that may give a similar picture (differential diagnosis such as hypothyroidism, dementia, psychosocial reason, grief, etc.) is important. It is important to recognize that the assessment of thoughts related to helplessness, hopelessness, worthlessness, and suicide may be difficult and in some adults with ID is almost impossible to determine if the person cannot communicate their feelings and thoughts.
A thorough risk assessment is necessary, particularly for both self-harm/ neglect and harm to others. It is important to consider that depression may present atypically (e.g., hypersomnia instead of lack of sleep and increased instead of decreased appetite etc) in this population. In people with severe and profound ID, the diagnosis may depend more on behavioural symptoms. Depression should be suspected where there is a change or onset in problem behaviour, associated with some of the 'biological' symptoms of depression such as changes in sleep and appetite. However, other causes of behaviour change should always be excluded first. Problem behaviour alone in the absence of any other symptom of depression must not be diagnosed as depression.
Deterioration in skills, on the other hand, even in adults with severe ID may indicate the onset of a depressive disorder. It may be useful where there is doubt about the diagnosis, particularly in those with severe or profound ID, for family and other caregivers to carefully record daily, over a period (for example, a week/ month) behaviours that would be suggestive of depression, such as sleep disturbance, social withdrawal, overall appearance, loss of communication (however limited), level of problem behaviour, and how the person appears in mood (for example, "looks sad", “tearful for no apparent reason”). Where diagnosis continues to be in doubt, a trial of antidepressant medication could be considered, although a positive response to antidepressants does not confirm a diagnosis of depression.
Bipolar disorderThe rate of bipolar disorder I is about 1% in the non-ID general population.7 In adults with ID, the rate has been reported to be between 0% to 2.2%.66,67 It is possible that this diagnosis is often missed in adults with ID, and an alternative diagnosis of problem behaviour is used instead. Certain genetic disorders associated with ID may also predispose to bipolar disorder.48,58
Recommendation (C)In adults with ID, the mood may be predominantly irritable rather than elated. It may be associated with aggression. Delusions and hallucinations may be present, but not convincingly diagnosed in those with a moderate or more severe ID. Delusions tend to be simpler. Therefore, an adult with an ID who cannot drive may have a grandiose delusion that he can drive a car, whereas a person who does not have an ID may believe that he is the King of his country. Self-injurious behaviour may be associated with mania or hypomania in adults with ID.
Other symptoms reported, include aggression, destructive behaviour, restlessness, intensified or rambling speech, echolalia (repetitive speech), both increased and decreased appetite, crying, and overactivity. Core symptoms are likely to be irritability, labile mood, overactivity, and sleep disturbance.66 As in the case of major depressive disorder, cognitive features like inflated self-esteem and grandiose delusions are likely to be less commonly detected symptoms in adults with ID. The pressure of speech may manifest as increased vocalisation or gesturing in adults with ID who have otherwise very limited communication skills.66 An adult with severe ID with no speech has been described by Pary and colleagues67 as becoming completely silent during the depressive phase and vocalising continuously during the manic phase.
Several authors have suggested that rapid cycling bipolar disorder may be common in adults with ID.66 However, this diagnosis has to be made with caution. Many adults with ID show cyclical changes in their behaviour, which can be associated with altered mood.68 Many physical factors such as changes around the time of menstrual periods in women, epilepsy that shows 'clustering', etc., and various environmental factors may account for this type of cyclical mood and behaviour changes.48,66 Therefore, bipolar disorder should not be diagnosed in adults with ID only based on the presence of cyclical mood and behaviour changes.
Anxiety disordersIn the non-ID general population, the rate of overall anxiety disorder has been reported to be 10.4%69 compared with 14% in adults with ID.56 However, anxiety symptoms are much more common in adults with ID than the diagnosis of an anxiety disorder. It is also possible that a diagnosis of anxiety disorder is missed in some adults with ID.70 Generalised Anxiety Disorder, on the other hand, has been estimated at 3.1% to 7.9% in the non-ID general population7,69 and between 2.2% and 5.5% among adults with ID.4,5 Panic disorder is reported among 1.1% of both non-ID and ID adults.7,56
A significantly higher rate of phobic disorder (4.4%) is reported among adults with ID in one study5 compared with 1.1% in the non-ID general population.7 Obsessive Compulsive Disorder is diagnosed among 1.1-2.7% adults with ID5,71,72 compared with 1.1-1.8% non-ID general population.1
Recommendation (C)It is worth remembering that adults with ID because of their limited coping skills may find certain situations anxiety-provoking that may not be anxiety-provoking for non-ID adults. Also, many adults with ID, particularly those with autistic traits find the change in routine extremely anxiety-provoking. It is not surprising that many adults with ID find their life stressful given that often the locus of control in their lives is situated externally.
Although the subjective experiences of many anxiety disorders are difficult to determine in many adults with ID, particularly those who have a severe and profound ID, the physical signs associated with anxiety such as sweating, pacing up and down, fearful facial expression, avoidance of certain situations or people, sleep problem, trembling, shortness of breath, etc. may be apparent to the observers.73,74 Subjective feelings of physical symptoms of anxiety such as palpitation, a sinking feeling, butterfly in the stomach, etc. would be difficult to describe by most adults with ID who do not have sufficient communication skills.
Some of these symptoms on their own may not be predictive of an anxiety disorder. For example, sleep problem is common in ID and many other psychiatric and medical conditions. Similarly, shaking and trembling could be associated with stereotypy or other involuntary movements commonly associated with ID or medication-related adverse events. Restlessness could be a side effect of psychotropic medications that are commonly prescribed for adults with ID.25
Selective mutism is also included within the anxiety disorder category in the DSM-V.1 Selective mutism is common in adults with ID, particularly in ASD. This may be precipitated by a stressful life event and maybe a defence mechanism on the part of the adult with ID who wants to protect herself or himself from external stressful stimuli. However, in adults with ID elective mutism may be difficult to distinguish from a depressive disorder, apathy, regression due to traumatic life events or even catatonia.
Generalised anxiety disorder73,74In adults with ID who cannot communicate their feelings and thoughts certain anxiety-related symptoms such as persistent nervousness, light-headedness, palpitation, butterflies in the stomach may be difficult to detect but physical signs such as trembling, muscle tension, sweating, etc. could be detected on observation. Some adults with ID may be able to describe persistent generalised anxiety or tension. Other signs such as persistent irritability, difficulty getting to sleep, or physical complaints may be noticed even in adults with severe ID. However, it is worth noting that sometimes anxiety may cause or present as a problem behaviour. The co-existence of depression is common and should be ruled out.
Phobia5,56,73,74Adults with ID may show external signs of anxiety but may not be able to describe their inner agitation or fear. When anxiety cannot be expressed, it may present as a change in behaviour. Many people with ID will not realise that their fears are unreasonable (which is a diagnostic criterion for phobia in the general population) or even if they do, they may not be able to communicate that to others. Phobic disorders are difficult to diagnose in adults with ID, except possibly in those with mild ID, although some signs of anxiety may still be identifiable. Specific phobias to ordinary things that usually won't cause phobia in the general population such as dogs, water, storm, stairs, crowds can be common in adults with ID. However, they should be carefully distinguished from reasonable fears of such things. The behavioural analysis may identify anxiety as the trigger for challenging behaviour (use Comprehensive Assessment of Triggers for beahviours of concern Scale (CATS) for the assessment of triggers for problem behaviour; https://spectrom.wixsite.com/project).75 Like in the generalised anxiety disorder, depression may co-exist with phobia and neede to be detected and treated.
Obsessive compulsive disorder (OCD)71,72One diagnostic criterion for OCD in the general population is that the obsessions or compulsions must be recognised by the person as originating in her/ his own mind. However, adults with ID may find it difficult to recognise this. Another criterion is that obsession and compulsion must be repetitive and unpleasant, and seen as excessive and unreasonable. However, many adults with ID may find it difficult to recognise or communicate these thoughts as excessive and unreasonable. In the general population, the person with OCD will attempt to resist ‘thinking’ the obsessional thought or carrying out the compulsion, although the degree of resistance may be minimal in long-standing disorders. Not all adults with ID would be able to resist ‘thinking’ or communicate these feelings to others.
In the general population, experiencing the obsession or carrying out the compulsion is not pleasurable, although it may bring temporary relief. However, not all adults with ID will be able to communicate their feeling of relief. In the general population, the obsessions or compulsions must cause distress or interfere with the person's social functioning. In the case of an adult with ID, the distress may be expressed through problem behaviours. The symptoms must not be due to another mental disorder, such as a psychotic disorder or an affective disorder.
Importantly OCD in adults with ID has to be distinguished from other forms of stereotyped behaviour and self-injurious behaviours that are common in many people with ID. Similarly, the ritualistic behaviour seen in many people with autistic traits has to be distinguished from true OCD symptoms in many people with ID.
Post-traumatic stress disorder (PTSD)Adults with ID do experience traumatic events and may be at a higher risk for some traumatic experiences than the general population.76 Traumatic events that may appear less traumatic or trivial to the non-ID general population such as a move to a new accommodation may have a profound impact on adults with ID. It is possible that in adults with mild ID the presentation of PTSD symptoms is similar to that in the non-ID general population.77 One recent study found the rate of PTSD among 19.7% of people with mild ID as opposed to 10.4% in the non-ID general population.78,79
Recommendation (B)The diagnosis of PTSD relies on the person being able to describe quite complex internal states. Therefore, it becomes very difficult if not impossible to make this diagnosis in adults with severe and profound ID. Childhood abuse is not uncommon in people with ID which may precipitate psychopathology in adulthood including problem behaviour which has to be distinguished from PTSD.
However, in adults with severe ID, the presentation may be behavioural in the form of post-traumatic enactment which can be mistaken for psychosis and expressed as bizarre behaviours, aggression, agitation, self-injurious behaviour, and avoidance of particular activities (this may indicate avoidance of a stress-provoking situation).80 Some suggested that the higher the cognitive deficit the higher is the risk of developing PTSD and the more severe is the form of PTSD.81,82 However, this suggestion has to be interpreted with caution as the diagnosis of PTSD in people with more severe ID is dependent on behavioural manifestation, which could be indirect evidence of PTSD but there could be many other reasons for the same behaviour change.
Inconsistent definition of trauma and absence of a validated instrument make the diagnosis of PTSD in adults with ID difficult. However, recently some preliminary validation has been carried out in the ID population of a revised version of the Impact of Event Scale-Intellectual Disabilities (IES-IDs)83 and Lancaster and Northgate Trauma Scale (LANTS).84 The dependence on third-party reporting to make the PTSD diagnosis is common in ID but cannot be always relied upon if not backed up by the person's own account.
DiscussionA guideline like this is likely to be useful for psychiatrists and other related health care professionals and other people caring for adults with ID. This is particularly likely to be useful for psychiatrists who have very little training and experience in working in the field of ID. A recent survey of 41 European countries has shown very little training available in psychiatry of ID apart from the UK.85 In the UK there is a 3-year higher training available dedicated to the psychiatry of ID. In just over half of the other European countries surveyed there is training in the form of clinical placement, lectures, or courses. Currently available diagnostic manuals such as DC-LD8 and DM-ID-29 are published as books and are not free. A lot of new evidence has become available for updating since the previous guidelines and diagnostic manuals were published, We, therefore, updated and incorporated this evidence within the current guideline. We have excluded grey literature as it was difficult to assess their quality using the SIGN 50 criteria. The existing published papers on the subject primarily concentrate on prevalence and risk factors for various psychiatric disorders among adults with ID and do not provide guidance on the assessment and diagnosis of these disorders. Therefore, a publication of this guideline in a European journal is likely to reach many more clinicians who would benefit from a guideline like this. Also compared with the published books this guideline is much more succinct. However, because of the succinct nature of this guideline, it is not possible to provide in-depth information on each psychiatric disorder. However, this guideline describes the main areas where the psychiatric symptoms are likely to manifest differently in adults with ID compared with those without ID. This should help to improve clinicians’ practice.
Although we wanted the guideline to be evidence- and consensus-based, the quality of evidence we found overall is not so good. Because of this, most recommendations fell into the category B or C. Given the nature of the subject, most papers included in the review are either review articles or book chapters but not primary research. However, reviews and book chapters have already synthesised available evidence on the subject. Therefore, the guideline was primarily consensus-based but we did not use any systematic method such as Delphi to gather consensus. However, NICE does not recommend Delphi for guideline development. That said, the main two international psychiatric diagnostic criteria, DSM and ICD are primarily consensuses- rather than evidence-based as it is difficult to gather evidence on the subject. There is now a move to produce more evidence-based DSM and ICD criteria in the future. The guideline was not put through any stringent quality control process like in our previous treatment guideline that used AGREE criteria.86 We did not have the opportunity to widely discuss the recommendations and gather a large number of feedbacks through worldwide consultation. As a result, only a limited number of experts from Europe remained involved in the development of this guideline. We have not reviewed treatment options for psychiatric disorders on which many clinicians would expect guidelines. This was beyond the remit of our paper as we had to keep the paper succinct. For the same reason, we have not reviewed evidence related to the diagnosis of psychiatric disorders in children with ID. The issue of diagnosis and treatment of problem behaviour in adults with ID is a large one and could not be accommodated within the space of this paper. If this guideline is found useful then in the future further similar guidelines could be developed for children and also on pharmacological and non-pharmacological interventions of psychiatric disorders and also problem behaviours in ID.
Key conclusions and learning points- •
Adults with intellectual disabilities (ID) suffer from the same range of psychiatric disorders as their non-ID counterparts.
- •
The prevalence rate of psychiatric disorders in adults with ID varies depending on how psychiatric disorder is defined, the population studied and the instruments and diagnostic criteria used.
- •
However, it seems that the overall point prevalence of functional psychiatric disorders such as schizophrenia, major depressive disorder, bipolar disorder and anxiety disorders in adults with ID excluding the diagnosis of problem behaviour and ASD is somewhere between 14.4-22.4%, whereas that in the non-ID general population is around 16%.
- •
The prevalence of wider psychopathology including problem behaviour and other NDDs, however, is much higher in adults with ID compared with the general population.
- •
The prevalence of certain psychiatric disorders such as schizophrenia and dementia are significantly higher in adults with ID compared with the general population.
- •
Risk factors for psychiatric disorders in ID seem similar to what is expected in the non-ID general population, with more emphasis on genetic and environmental factors.
- •
Certain psychiatric disorders, for example, schizophrenia is difficult if not impossible to diagnose in adults with severe and profound ID who do not have sufficient communication skills.
- •
There is a major overlap of phenotypes associated with ID and symptoms of many psychiatric disorders.
- •
It is, therefore, of paramount importance to have a baseline of mental state to compare with any possible emergent psychiatric symptoms.
- •
Assessments of the level of intellectual and socio-emotional functioning, as well as physical and sensory impairments, are necessary to define an individual's baseline for the psychiatric evaluation.
- •
Neurodevelopmental disorders such as ASD and ADHD are common comorbidities in adults with ID.
- •
ASD is associated with increased psychopathology such as psychosis and anxiety.
- •
Psychiatric disorders may manifest differently in adults with ID than in the non-ID general population.
- •
It is often difficult to apply diagnostic criteria and diagnostic instruments developed for the non-ID general population to adults with ID.
- •
There is not a diagnostic instrument that can be applied across the board to adults with all levels of severity of ID.
- •
Both false positive and false negative diagnoses of psychiatric disorders are common in adults with ID.
- •
For example, problem behaviour may be a manifestation of underlying psychiatric disorders in some adults with ID. However, not all adults who display problem behaviour suffer from a psychiatric disorder and there are many causes (including genetic, environmental, psychosocial, etc.) of problem behaviour other than a psychiatric disorder.
- •
Similarly, not all adults with ID who have a psychiatric disorder will show problem behaviours.
MO did the literature search. MO and BP screened the abstracts. MO and SD extracted data. SD wrote the initial draft. SD, BP, MO and KK contributed to the guideline. All authors contributed to the manuscript and approved the final version of the manuscript.
Appendix 1: Search terms.
Appendix 2: Summary findings of the included studies.
Appendix 3: Diagnostic and screening instruments.