Cytomegalovirus (CMV) is a virus belonging to the family of herpes viruses. Clinically significant CMV infection usually occurs in immunocompromised (ICD) patients. In immunocompetent (ICT) patients, the virus shows low pathogenicity, and the infection is usually asymptomatic or presents as a mononucleosis syndrome. Gastrointestinal tract (GIT) involvement with CMV is well known in ICD patients, but is much rarer in ICT patients.1 We present the case of an ICT patient with ileitis secondary to an initial CMV infection.
A 50-year-old woman was referred to the Emergency Department by her primary care physician due to presenting a high temperature for one month and elevated transaminases. The patient also reported diarrhoea, with four loose stools per day and no pathological products. In the four months prior, she had also lost 10kg in weight after starting a low-calorie diet.
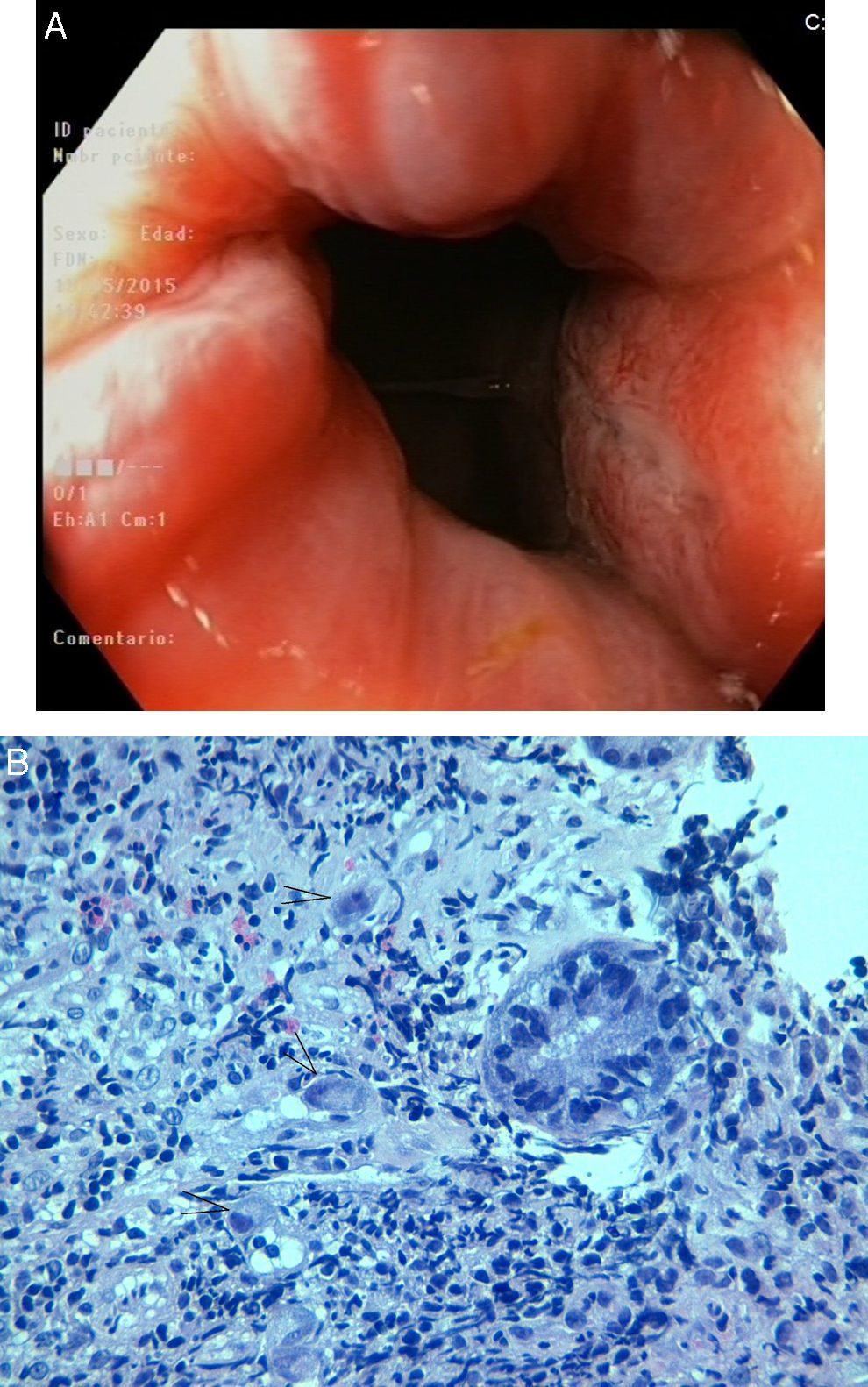
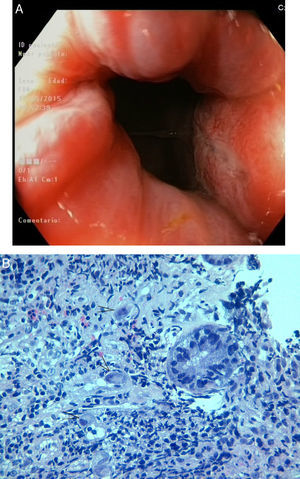
Among her medical notes, an allergy to beta-lactam antibiotics, pyrazolones and iodinated contrasts was particularly notable, along with pulmonary tuberculosis in her youth that was properly treated, bronchial asthma with occasional inhaled steroids and an appendectomy due to perforated appendicitis the previous year. Upon admission, the patient had a fever (temp.: 37.8°C) and there were no relevant findings on physical examination. In the blood tests performed on admission, she presented lymphocytosis and abnormal liver tests with an alkaline phosphatase level of 714U/l, GOT: 132U/l, GPT: 198U/l, GGT: 431U/l and LDH: 761U/l. The clotting test was normal. Upon admission, blood cultures were ordered, which came back negative, as well as serological tests for hepatitis A, B and C, HIV and syphilis, which were also negative. The patient's CMV serology test showed positive IgM and IgG antibodies, while the EBV test revealed negative heterophile antibodies and positive VCA IgM, VCA IgG and EBNA IgG. The CRP test for CMV in blood was negative (<150copies/ml). An abdominal CT scan, which showed a circumferential thickening of the ascending colon wall, and a complete posterior colonoscopy, in which aphthous ulcers in the terminal ileum were described, were performed (Fig. 1A). In the ileum biopsy samples, fragments of mucosa with preserved architecture were identified, alternating with other areas showing zones of erosion and ulceration, with granulation tissue and acute and chronic inflammatory infiltrate. In the ulcerated areas, large, stromal and endothelial cells were identified with intranuclear and intracytoplasmic viral inclusions (Fig. 1B). Immunohistochemical techniques were performed with positive staining for CMV. Colon biopsies showed only mild chronic inflammatory signs. During admission, the patient's evolution was favourable, with her fever disappearing on the 5th day, along with cessation of the diarrhoea and a progressive improvement in transaminase levels. As such, no specific treatment for CMV was proposed. She was assessed one month later at an outpatient clinic, where the normalization of her liver tests was verified. Although the patient's clinical picture was compatible with CMV infection, we decided to carry out clinic-based follow up in order to rule out the future appearance of Crohn's disease beginning with the spontaneously-resolving ileocolitis and associated CMV infection.
Gastrointestinal involvement with CMV is rare in ICT patients. Any segment of the GIT, from the oesophagus to the rectum, may be involved. The most common is the involvement of the colon, with small intestine involvement being much rarer. Most cases of CMV colitis in ICT patients occur in older patients, which probably reflects the physiological deterioration of the immune system with ageing.2
Clinical manifestations of CMV GIT infection include diarrhoea (76%), abdominal pain (52%), and bleeding (27%). Intestinal perforation is a very rare complication (less than 1%), but is potentially fatal in these patients. The most characteristic endoscopic findings are the presence of well-defined medium or large ulcers, separated by areas of normal mucosa, as was the case in our patient. The presence of a friable and oedematous mucosa, thickened folds, pseudopolyps or even pseudomembranes can also be observed. These findings are non-specific and, occasionally, CMV enteritis may be confused with other entities such as inflammatory bowel disease, ischaemic colitis and Clostridium difficile colitis.3,4 The definitive diagnosis of CMV enteritis is based on histological findings. CMV produces a characteristic cytopathic effect, giving rise to basophilic intranuclear inclusions, sometimes surrounded by a lighter halo, and intracytoplasmic inclusions. Haematoxylin–eosin staining of the biopsy specimens is not 100% sensitive. The use of immunohistochemical techniques with monoclonal antibodies against CMV results in better detection. Other findings, such as positive anti-CMV IgM titres, CMV antigen detection in blood or positive CRP in blood or urine, may confirm the diagnosis but have a low sensitivity.5
As for the pathogenesis of CMV enteritis, two theories have been proposed: (1) The primary theory proposes that CMV can proliferate in vascular endothelial cells, leading to vasculitis and thrombosis of small vessels with local mucosal ulceration; (2) In contrast, the secondary theory sustains that other previous diseases, such as ischaemic colitis or inflammatory bowel disease, are responsible for the destruction of the colonic mucosa, leading to a local immunosuppression that favours superinfection by CMV.6
Treatment of clinically significant infections requires the use of antivirals such as ganciclovir, valganciclovir, foscarnet and cidofovir. In a meta-analysis performed on ICT patients, the overall mortality of CMV colitis was 31.85%. Spontaneous resolution occurred mainly in patients below 55 years of age, with no comorbidities, and the authors thus recommended not treating these patients. In contrast, other factors such as an age of over 55 years, being male, the presence of comorbidities affecting the immune system and the need for a colectomy, negatively affected survival, and it is thus recommended that antivirals be used in this group of patients.7 Our patient matched the group described by these authors as having a good prognosis, and also evolved favourably without the need for antiviral treatment.
In conclusion, CMV enteritis is a rare entity in ICT patients. Macroscopically, it can simulate other diseases, so its diagnosis requires a high degree of suspicion. The performance of specific techniques, such as immunohistochemistry with monoclonal antibodies against CMV, improves the performance of the biopsy samples. In these patients, it is also necessary to exclude any cause of occult immunodeficiency, and to identify the poor prognostic factors that indicate the need to initiate early antiviral treatment.
Please cite this article as: Ameneiros-Lago E, Fernández-Fernández FJ, Mosquera-Martínez MT. Ileítis por citomegalovirus en una paciente inmunocompetente. Gastroenterol Hepatol. 2017;40:294–295.