The side effects of opioids on the gastrointestinal system have been widely recognized in the literature. They exert their action on the enteric nervous system, through the receptors located in the myenteric plexus (Auerbach's plexus) and the submucous plexus (Meissner's plexus), which are distributed throughout the intestinal system. These receptors (named μ, δ and κ) mediate the effects produced in the human gastrointestinal system.1,2
The main adverse effect of opioids studied at the gastrointestinal level has been intestinal dysfunction in the form of constipation, due to the greater understanding of the physiology of opioid receptors in the colon.3 However, the effect on oesophageal motility has been scarcely assessed. There are few clinical studies, and most are retrospective. These studies suggest that the chronic use of opioids leads to a dysfunction in oesophageal motility.
We present the case of a 62-year-old woman with a history of chronic lower back pain, undergoing treatment with transdermal patches of 30mg (52.5μg/h) buprenorphine every 72h for the past 8 months, who was referred to the Functional Digestive Testing Unit with dysphagia. The patient's dysphagia occurred daily and was predominantly to liquids, thus interfering with her daily life (grade 2, Vantrappen et al.4). Other associated symptoms included regurgitation and chest pain, and to a lesser extent the presence of heartburn. A barium swallow study was performed, which was normal, and an upper digestive endoscopy with biopsies was also shown to be normal. The study was continued with a high-resolution manometry (HRM) and a pH-impedancemetry. The manometry was performed after a fasting period of 8h, in supine position, using a device with perfused catheters (Medical Measurement System [MMS], Enschede, Netherlands), based on the protocol of our unit.5 The manometric diagnosis was established according to the Chicago Classification Criteria of Esophageal Motility Disorders, version 3.0.6
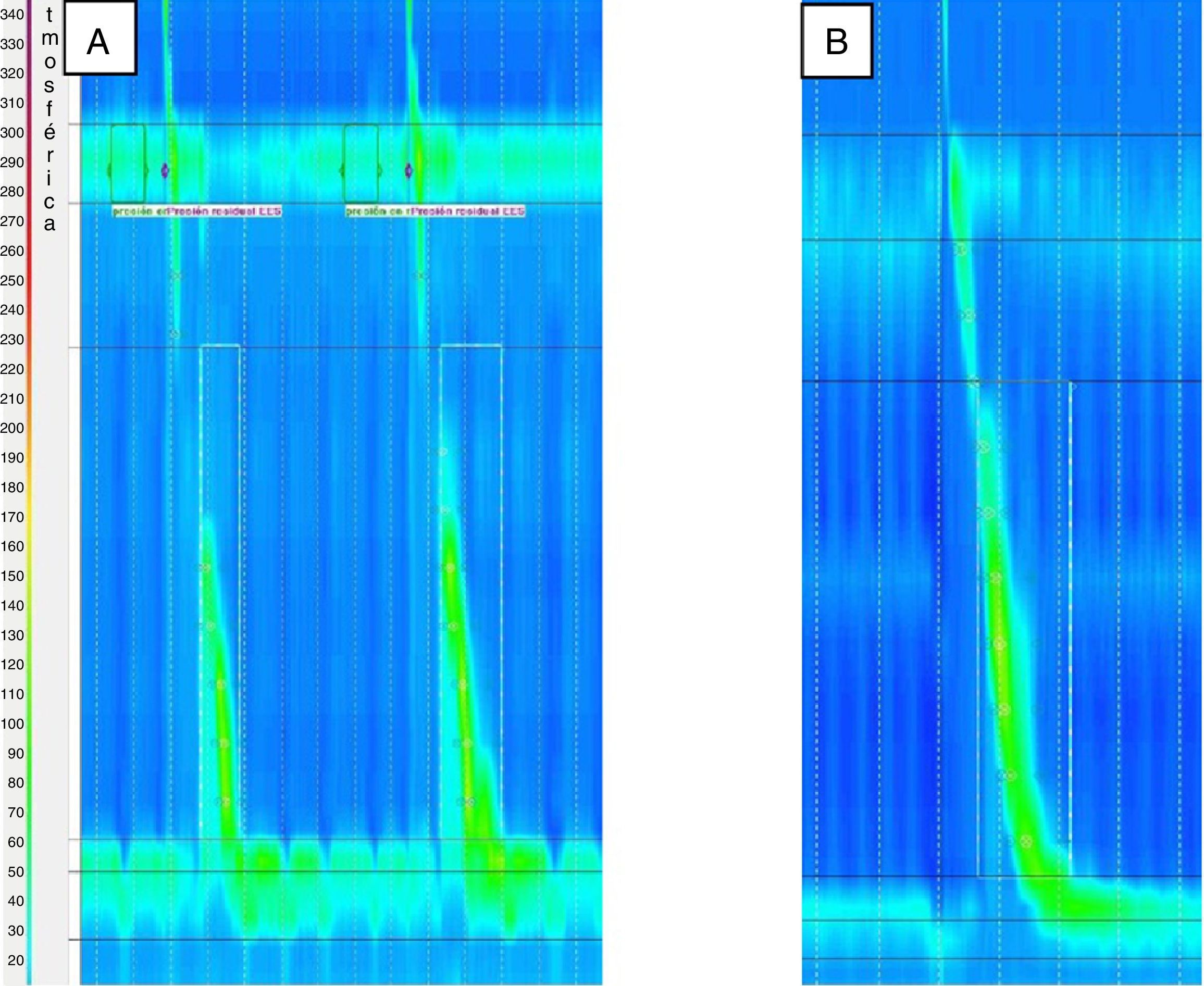
The study with high resolution manometry showed a pathological relaxation of the lower oesophageal sphincter (LOS), determined by a 4-second integrated relaxation pressure (4s-IRP) of 12.5mmHg and increased baseline LOS pressure with a value of 40mmHg. Based on the Chicago Classification, a functional oesophago-gastric junction (OGJ) obstruction was diagnosed. The pH-impedancemetry study was normal and ruled out reflux disease. Given the findings of the manometry, a computed tomography (CT) scan of the cervicothoracic region was requested to rule out an underlying organic disease. The CT scan was normal.
In light of the patient's symptoms, drug treatment with calcium antagonists was initiated. Nevertheless, the patient's symptoms improved only slightly, and her dysphagia persisted. We then decided to perform a pneumatic dilation session due to the severity of the dysphagia. However, the patient refused. Her medical history was reviewed and, since there were no previous conditions explaining the dysphagia and the initiation of opioid treatment preceded the onset of her symptoms, we decided to discontinue the analgesic treatment with transdermal buprenorphine patches. One month after the withdrawal of the opioids, another clinical and manometric assessment was performed. The HRM showed normal relaxation with a 4s-IRP of 1.4mmHg and a decrease in baseline LOS pressure from 40mmHg to 29mmHg, meeting the Chicago Classification (Table 1 and Fig. 1). From the clinical point of view, the patient presented a significant improvement with occasional symptoms (grade 1, Vantrappen et al.).
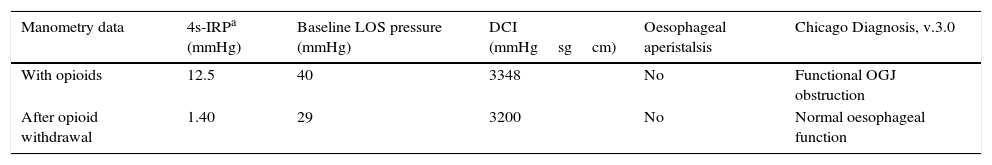
Recording of high-resolution manometry data during opioid treatment and after opioid withdrawal.
| Manometry data | 4s-IRPa (mmHg) | Baseline LOS pressure (mmHg) | DCI (mmHgsgcm) | Oesophageal aperistalsis | Chicago Diagnosis, v.3.0 |
|---|---|---|---|---|---|
| With opioids | 12.5 | 40 | 3348 | No | Functional OGJ obstruction |
| After opioid withdrawal | 1.40 | 29 | 3200 | No | Normal oesophageal function |
LOS: lower oesophageal sphincter; DCI: distal contractile integral; 4s-IRP: 4-second integrated relaxation pressure; OGJ: oesophago-gastric junction.
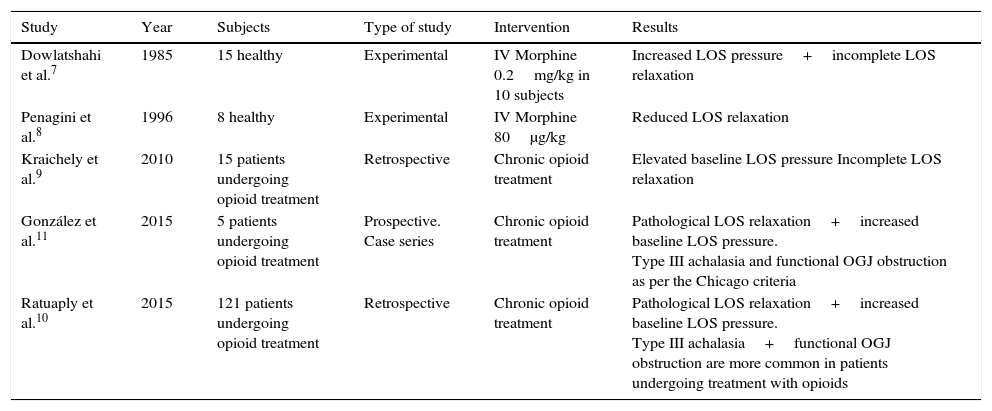
The effect of opioids on oesophageal motility has not been widely studied (Table 2). Experimental studies on healthy subjects have demonstrated an increase in baseline LOS pressure with incomplete relaxation on administering opioids.7,8 In clinical practice, Kraichely et al. confirmed, in a retrospective study of 15 patients with dysphagia and opioid consumption, an oesophageal motility disorder in the form of incomplete LOS relaxation and elevated baseline LOS pressure determined by HRM.9 Recently, a retrospective study of 121 patients on chronic opioid treatment suggested that oesophageal motility disorders with pathological LOS relaxation—such as functional OGJ obstruction and type III achalasia—are more common in patients undergoing chronic opioid treatment. This oesophageal motility disorder has been termed: opioid-induced esophageal dysfunction (OIED).10 On the other hand, it is suggested that suspending treatment with opioids reverses the oesophageal motility disorder.
Different studies addressing the effect of opioids on oesophageal motility.
| Study | Year | Subjects | Type of study | Intervention | Results |
|---|---|---|---|---|---|
| Dowlatshahi et al.7 | 1985 | 15 healthy | Experimental | IV Morphine 0.2mg/kg in 10 subjects | Increased LOS pressure+incomplete LOS relaxation |
| Penagini et al.8 | 1996 | 8 healthy | Experimental | IV Morphine 80μg/kg | Reduced LOS relaxation |
| Kraichely et al.9 | 2010 | 15 patients undergoing opioid treatment | Retrospective | Chronic opioid treatment | Elevated baseline LOS pressure Incomplete LOS relaxation |
| González et al.11 | 2015 | 5 patients undergoing opioid treatment | Prospective. Case series | Chronic opioid treatment | Pathological LOS relaxation+increased baseline LOS pressure. Type III achalasia and functional OGJ obstruction as per the Chicago criteria |
| Ratuaply et al.10 | 2015 | 121 patients undergoing opioid treatment | Retrospective | Chronic opioid treatment | Pathological LOS relaxation+increased baseline LOS pressure. Type III achalasia+functional OGJ obstruction are more common in patients undergoing treatment with opioids |
LOS, lower oesophageal sphincter; IV, intravenous; OGJ, oesophago-gastric junction.
The mechanism of these effects is not clear. The involvement of the nitric oxide pathway has been suggested as an underlying cause of the effects of opioids on oesophageal motility.9
Taking into account both our case and the literature review, it can be concluded that chronic opioid use could lead to oesophageal motility disorders, primarily motility disorders that occur with pathological relaxation and hypertonia of the lower oesophageal sphincter, similar to achalasia or functional OGJ obstruction. As such, these drugs should be taken into account in the differential diagnosis of oesophageal motility disorders and caution should also be exercised in the interpretation of an oesophageal manometry performed on patients receiving opioids.
Conflicts of interestThe authors declare that they have no conflicts of interest.
Please cite this article as: Sáez-González E, Díaz-Jaime FC, García-Morales N, Herreras-López J, Ortiz V, Ortuño J, et al. Obstrucción funcional de la unión esofagogástrica inducida por opiáceos. Gastroenterol Hepatol. 2017;40:296–298.