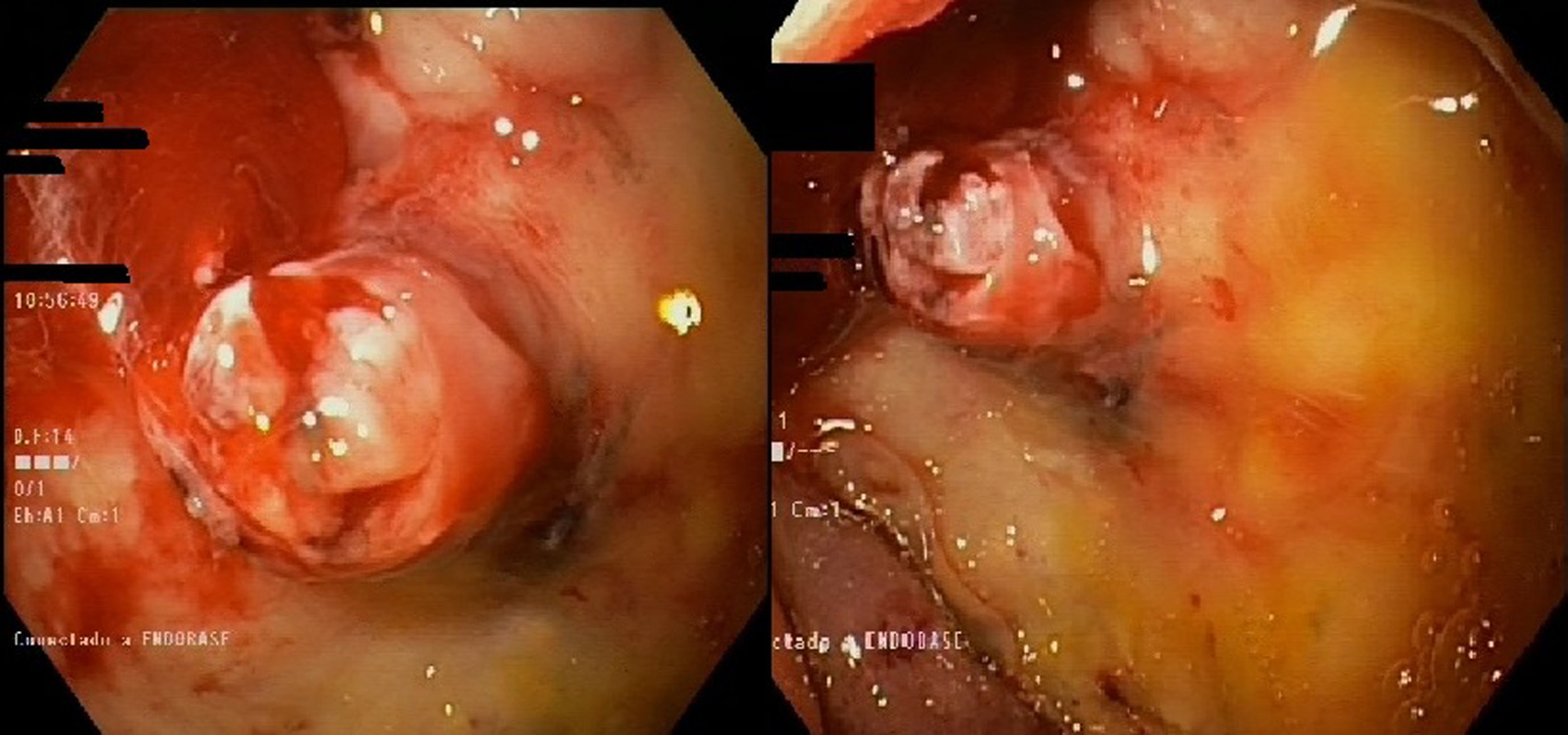
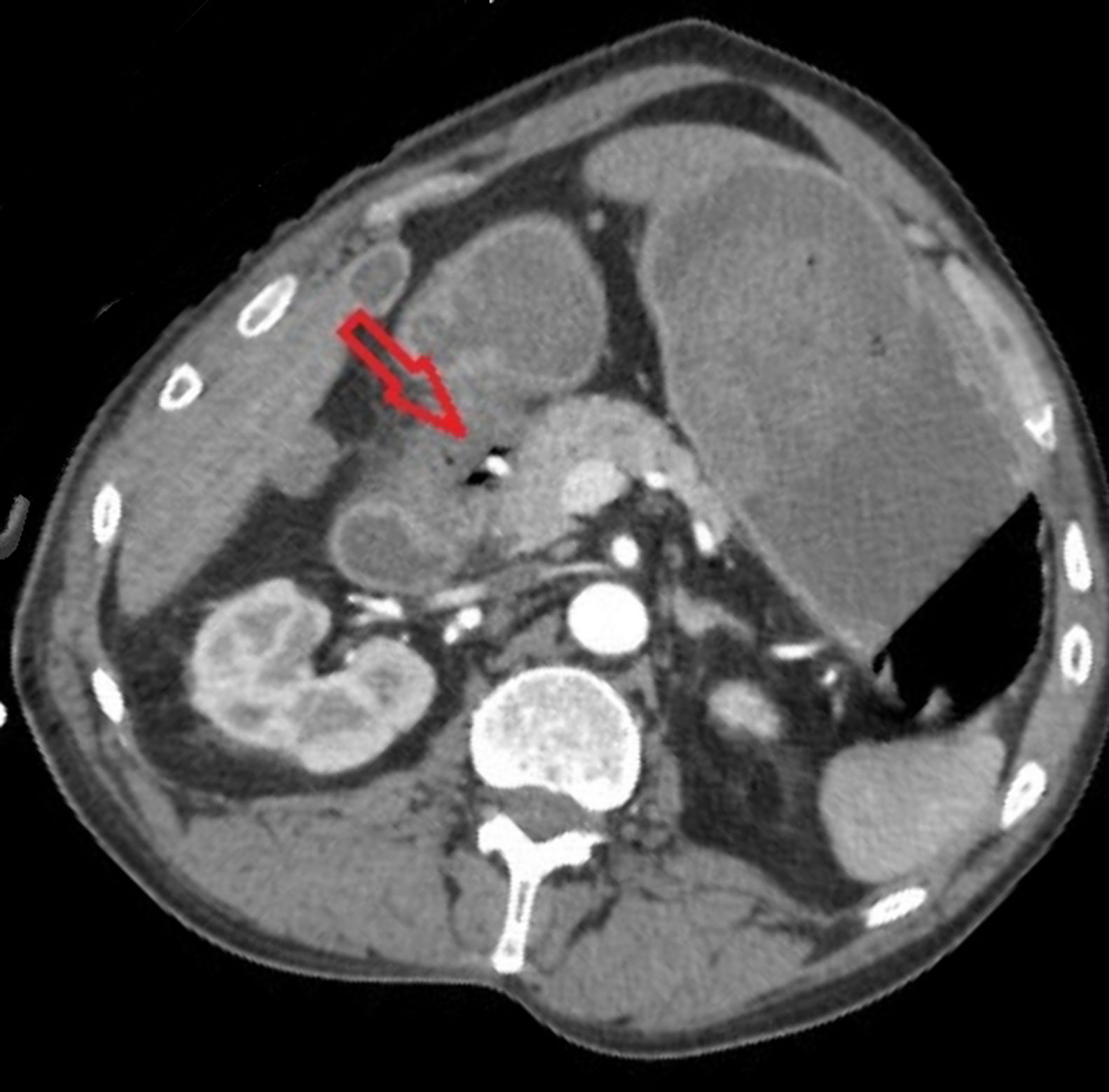
A 49-year-old man with a history of chronic alcoholism, post-traumatic subarachnoid haemorrhage and upper gastrointestinal bleeding eight years previously. He visited the A&E department with overt gastrointestinal bleeding in the form of melaena and later haematemesis and rectal bleeding. Once the patient was stabilised, an urgent gastroscopy was performed (incomplete due to abundant blood residue). The examination was repeated 12h later, showing a large duodenal ulcer actively oozing blood and a visible vessel (Fig. 1), which was sclerosed with adrenaline and Aethoxysklerol. A CT angiogram was then performed (Fig. 2), showing a pseudoaneurysmal dilation of the gastroduodenal artery in a possible duodenal ulcer bed which was treated by embolisation.
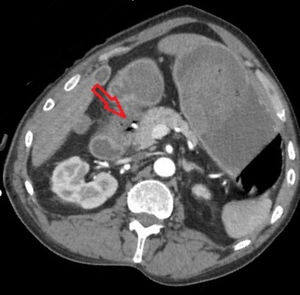
After absconding from hospital, the patient was readmitted five days later in haemorrhagic shock. A repeat CT angiogram was performed, which ruled out active bleeding, and two further gastroscopies, showing a Forrest IIc duodenal ulcer that was treated with sclerosing agent. Given the persistence of his anaemia, he was finally operated on.
Gastroduodenal artery pseudoaneurysms usually present with haematemesis and/or melaena which appear after chronic inflammation, sometimes associated with chronic pancreatitis.1 Endoscopic visualisation is rare and a computed tomography (CT) scan is generally required for diagnosis. A multidisciplinary approach is required2, which includes embolisation3 as the first line of treatment and surgery if that fails.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Ruiz Belmonter LM, et al. Pseudoaneurisma de arteria gastroduodenal. Gastroenterol Hepatol. 2021;44:306–307.