Portal pneumatosis or the presence of gas in the portal venous system is a rare radiological finding that can appear in the context of intestinal ischaemia and necrosis, constituting a very poor prognosis in this type of patient. Nevertheless, it may also be associated with less serious processes or conditions and therefore with a better prognosis.1
We present the case of a 62-year-old woman with a history of secondary biliary cirrhosis who underwent a liver transplantation less than one year ago, having developed significant post-sinusoidal portal hypertension with ascites in the postoperative period due to anastomotic stenosis between the cava and the liver graft, as well as occlusive condition of adherent origin conservatively resolved. Having presented progressive disorientation, dyspnoea and abdominal pain preceded by an episode of diarrhoea self-limited without pathological products in the preceding days, she was treated at home when her relatives detected a low level of consciousness. When evaluated by the emergency personnel, the patient presented a Glasgow score 3, reactive anisocoria with unilateral mydriasis and arterial hypotension with marked hypoperfusion. An abdominal exploration detected the presence of a very distended abdomen without abdominal guarding or signs of peritonitis. Orotracheal intubation was carried out in her home and high doses of vasoactive drugs were administered during the hospital transfer. Blood tests and complete cerebral and thoraco-abdomino-pelvic CT scans were subsequently performed.
The analyses showed worsening of renal function, severe hyponatraemia and hyperkalaemia, severe thrombocytopenia, mixed acidosis of metabolic predominance and coagulopathy.
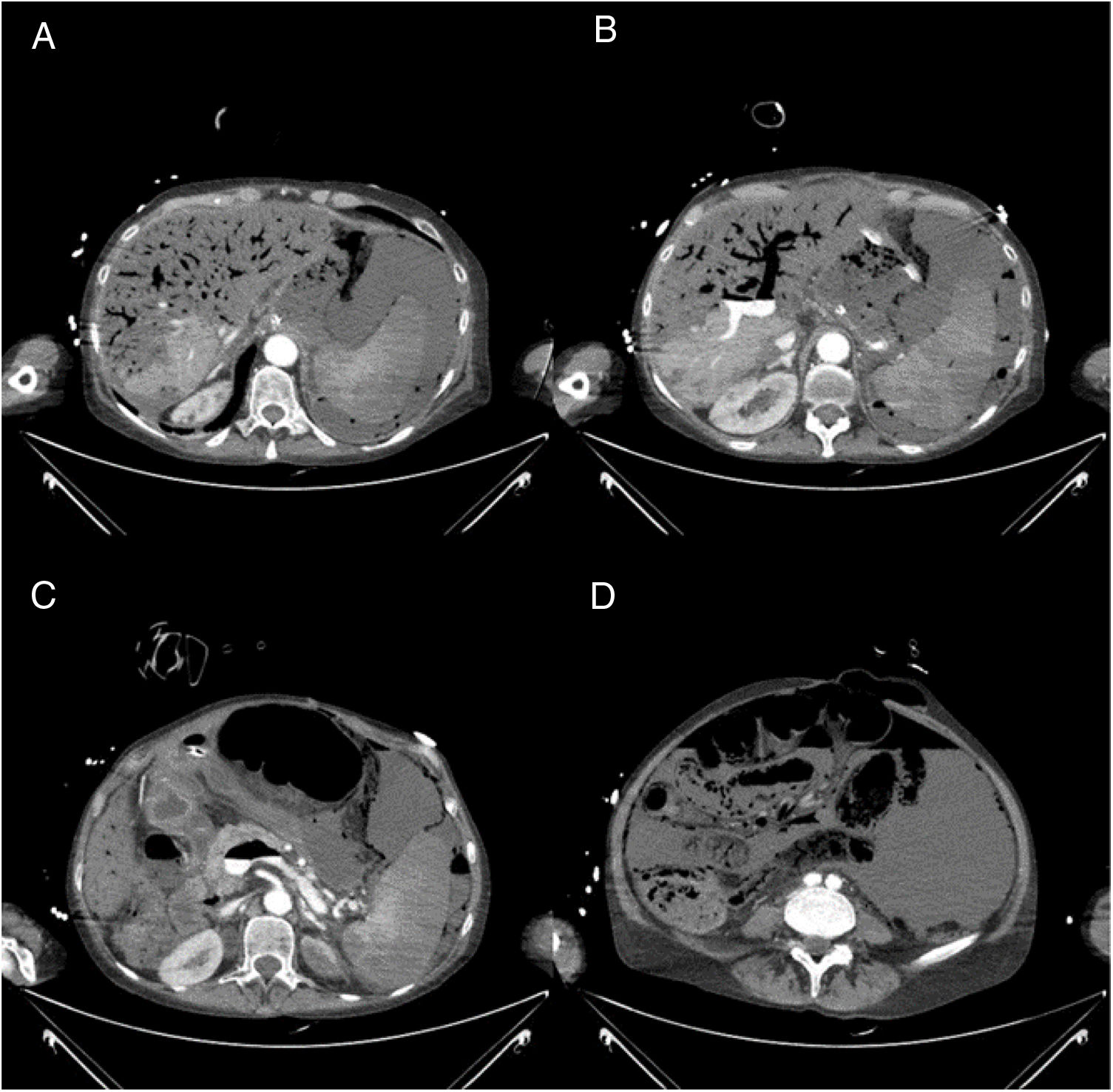
No intracranial abnormalities were detected on the brain CT. The thoraco-abdominal CT revealed left basal alveolar consolidation consistent with bronchoaspiration, pneumatosis intestinalis, abundant free peritoneal fluid, pneumoperitoneum and portal, splenic and mesenteric venous pneumatosis with hepatic and splenic hypoattenuation, all suggestive of intestinal ischaemia with associated visceral perforation and hepatic and splenic ischaemia (Fig. 1).
Abdominal CT findings. (A) Presence of intense portal pneumatosis with hypoattenuation of the liver and spleen parenchyma suggestive of ischaemia, as well as abundant free abdominal fluid. (B) Visualisation of hydro-air level in the portal venous system. (C) The hydro-air level is observed in the spleno-mesenteric axis. (D) Intense pneumatosis of the intestinal wall and pneumoperitoneum, suggestive of mesenteric ischaemia and intestinal perforation.
Despite the measures taken in the Intensive Care Unit, the patient rapidly progressed to multi-organ failure, dying a few hours after admission.
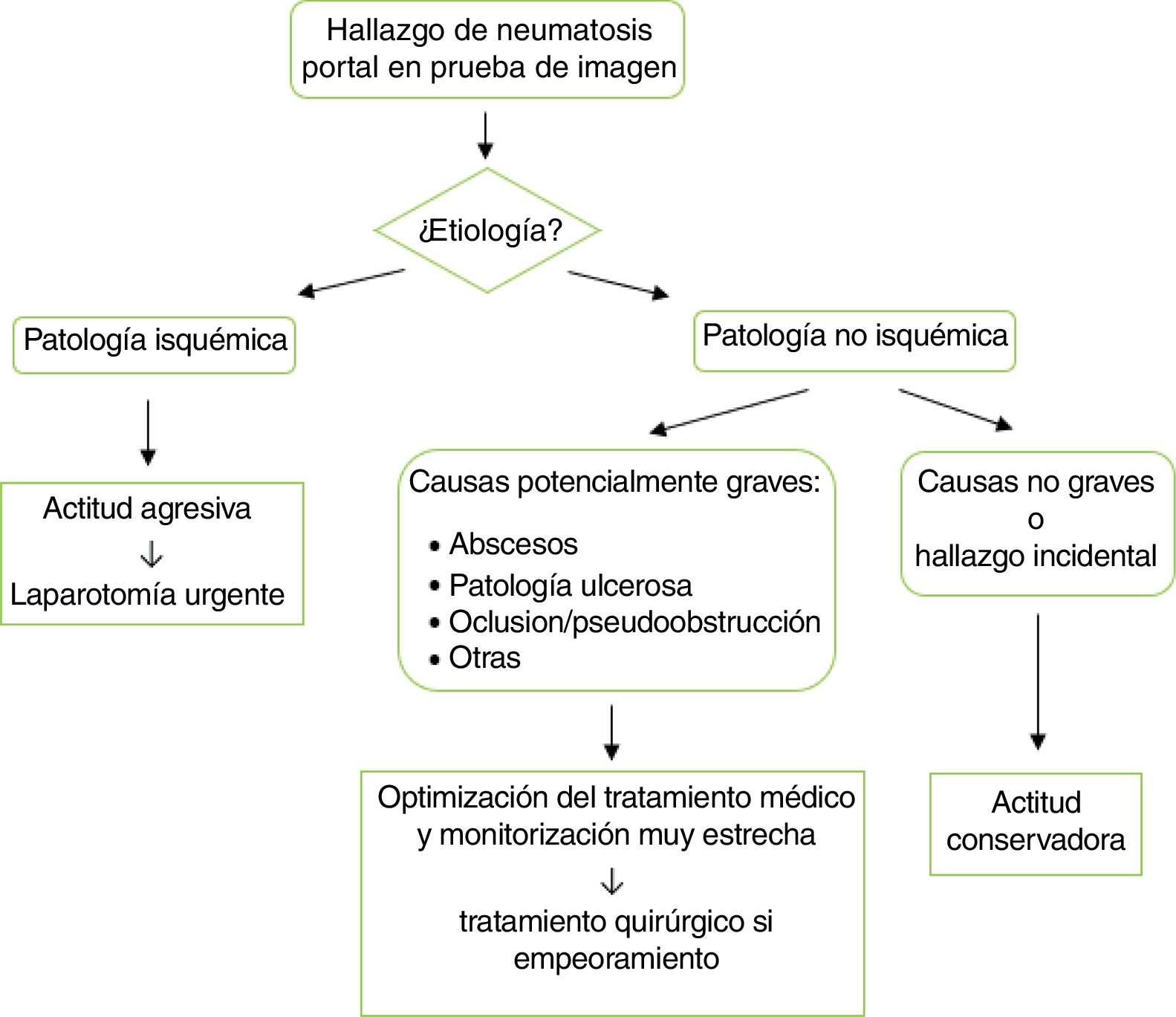
The finding of hepatic portal venous gas has been classically related to a fatal prognosis, with an associated mortality rate of up to 75%,2 since in most cases this radiological sign appeared in the context of pathologies with high morbidity and mortality, with mesenteric ischaemia being particularly noteworthy.2 However, at present the development and wide usage of CT for the diagnosis and study of various pathologies in routine clinical practice has made it possible to demonstrate this radiological finding more frequently, related to other less serious or non-ischaemic conditions, currently associated with an overall mortality of 39%. Among the many non-ischaemic pathologies in which this radiological sign has been described, the most notable are inflammatory bowel disease (8% of the total, and possibly presenting in both ulcerative colitis and Crohn's disease), paralytic ileus, occlusion and intestinal pseudo-obstruction (12%), intraabdominal abscesses (11%), gastroduodenal ulcerative pathology (4%), intraperitoneal tumours (3%) and other conditions such as suppurative cholangitis, acute diverticulitis and graft-versus-host disease.3 It can also appear in the context of iatrogenesis, such as after laparoscopic procedures, endoscopic retrograde cholangiopancreatography, gastric dilations, liver transplants, radiofrequency tumour ablations, arterial catheterisations and after the administration of enemas. However, the existence of mesenteric ischaemia continues to be frequent (up to 43% of cases), still determining a high mortality rate (approximately 75%), which is why an aggressive attitude is recommended in these cases through an emergency laparotomy. If the prognosis is better, conservative treatment can be chosen, usually yielding good results.1,4 A treatment algorithm is proposed in these cases (Fig. 2).
The pathogenesis of portal pneumatosis could be accounted for by the bacterial production of gas in the context of an infectious process and/or by the absorption of intraluminal air in processes involving disruption of the mucosa or increased intraluminal pressure.1,4
In conclusion, in the event of a radiological finding of portal pneumatosis, treatment should be oriented according to the underlying disease, which will determine the prognosis of the patients.
Conflicts of interestThe authors declare that they have no conflicts of interest.
Please cite this article as: Abad D, Laredo V, Hijos G, Alfaro E, Cañamares P, García S, et al. Gas venoso portal hepático, un hallazgo radiológico potencialmente grave. Gastroenterol Hepatol. 2020. https://doi.org/10.1016/j.gastrohep.2020.02.018