Gastrocolic fistulas can have numerous aetiologies, both benign and malignant. Benign entities include peptic ulcers, acute or chronic pancreatitis, and Crohn's disease. In western countries, the most common malignant aetiology is colon adenocarcinoma, while in eastern countries it is gastric adenocarcinoma. The incidence of a malignant fistula is very low: they appear in only 0.3%–0.4% of patients undergoing surgery for a digestive neoplasm.1
The most common clinical manifestations are feculent vomiting, abdominal pain, diarrhoea and weight loss.2
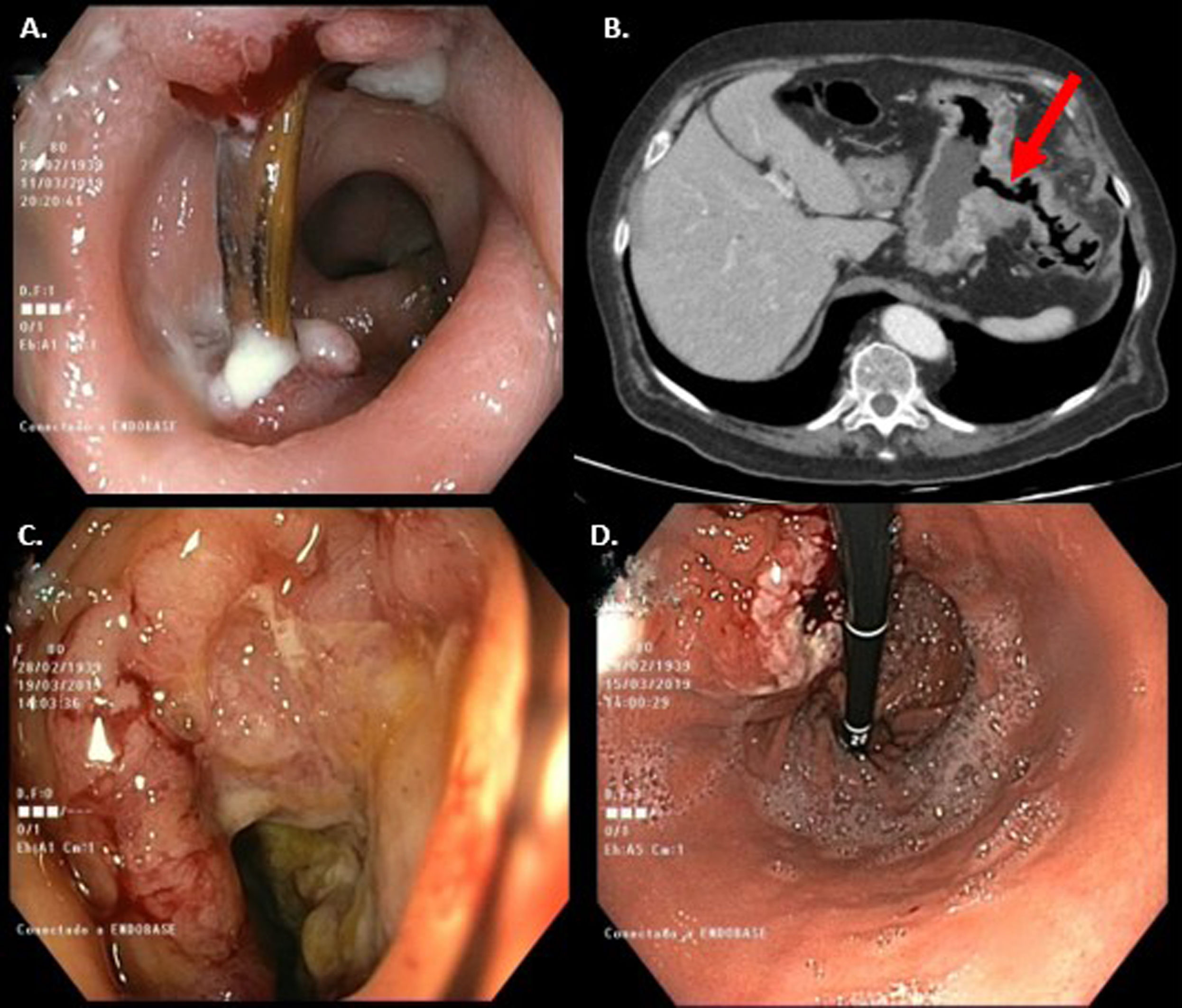
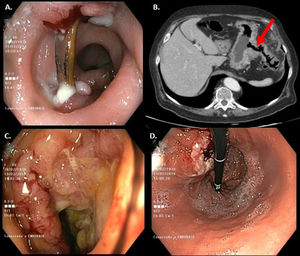
We present the case of an 80-year-old patient with a history of a cholecystectomy and a hiatal hernia operated by a posterior Toupet-type fundoplication. The patient presented for an outpatient colonoscopy for a microcytic anaemia study, in which, 25 cm from the anal verge, an elongated foreign body embedded at both ends (bone fragment) was observed, with the surrounding mucosa oedematous and erythematous (Fig. 1A). It was extracted in a second stage, 24 h later, using a foreign body forceps, and an abdominal computed tomography (CT) scan was performed showing a 45 × 38-mm mass in contact with the greater curvature of the stomach and splenic flexure of the colon that suggested communication between the lumen of both structures (Fig. 1B). Clinically, the patient reported postprandial dyspepsia and anorexia, with a weight loss of 3 kg in 6 months.
Endoscopic and radiological images of the foreign body and gastrocolic fistula A) Image of the foreign body embedded in the sigmoid colon. B) CT: fistulous path (arrow) between the gastric corpus and the left colon. C) Splenic flexure with ulcerated mucosa and impassable stenosis. D) Raised lesion with depressed centre suggestive of the gastric portion of the gastrocolic fistula.
The study was completed with a gastroscopy in which a 3−4 cm lesion with a depressed central area and raised margins with an inflammatory appearance, suggestive of a fistula (Fig. 1C) was observed in the gastric corpus, with an endoscopic ultrasound in which a solid 40 mm × 40 mm mass was observed that encompassed the gastric wall and communicated with the colon. A further colonoscopy revealed a mucosa with multiple ulcerations and an impassable stenosis at the splenic flexure (Fig. 1D).
The biopsies were consistent with a moderately differentiated adenocarcinoma of gastric origin (CDX2 and CK20 positive immunohistochemical study, with weakly positive CK7).
Therefore, the patient synchronously presented a foreign body lodged in the sigmoid colon and a malignant gastrocolic fistula.
The detection of foreign bodies in the colon is rare, since they are usually expelled spontaneously once they have reached it. Diagnosis is usually related to the appearance of a complication, such as intestinal perforation or digestive bleeding.3
Moreover, the detection of gastrocolic fistulas is exceptional. These, as occurred in our patient, usually communicate the greater curvature of the stomach with the distal half of the transverse colon, since at this point both organs are only separated by the greater omentum.2
There are 2 hypotheses to account for the formation of fistulas between the upper and lower digestive systems. The tumour can invade the adjacent organ through the greater omentum or cause, secondary to an ulcer, an intense peritoneal inflammatory reaction that produces adherence and subsequent fistulisation between both organs.1
Diagnostic methods include abdominal CT scan, gastroscopy, colonoscopy or a barium meal, which is the most sensitive procedure (up to 90%). Gastroscopy and colonoscopy are important, since they allow direct visualisation of the fistula and the taking of biopsies, although small fistulas may go unnoticed.4
Treatment is usually surgical, individualised in each patient based on tumour staging and comorbidities, although if possible an en bloc resection of the affected area with combined adjuvant chemotherapy is performed in some cases. The data available on the long-term post-surgical survival of these patients are scant.4
In our patient, an en bloc resection was indicated. However, during surgery, the tumour's unresectability was confirmed, since it infiltrated the root of the mesenteric vessels, whereupon the decision to perform palliative surgery, consisting of a feeding jejunostomy and a colostomy in the ascending colon, was taken. The patient died three months later.
In conclusion, malignant gastrocolic fistulas are infrequent. Diagnosis requires computed tomography, colonoscopy and gastroscopy, and treatment, when possible, consists of en bloc resection of the affected area.
Please cite this article as: Alfaro E, Laredo V, Cañamares P, Abad D, Hijos G, García Mateo S, et al. Hallazgo sincrónico de un cuerpo extraño en colon y una fístula gastrocólica de etiología maligna. Gastroenterol Hepatol. 2021;44:658–659.