We present the case of a 72-year-old woman, allergic to iodine contrast, with a history of type 2 diabetes mellitus, hypercholesterolaemia, goitre and hypothyroidism due to Hashimoto thyroiditis. She had been admitted on multiple occasions since 1997 for acute gastric dilatation secondary to pyloric stenosis, which was of unknown aetiology due to the patient's refusal to undergo diagnostic tests. She had severe ischaemic colitis, with secondary sigmoid perforation in 2006, requiring surgical resection and permanent colostomy in the left iliac fossa.
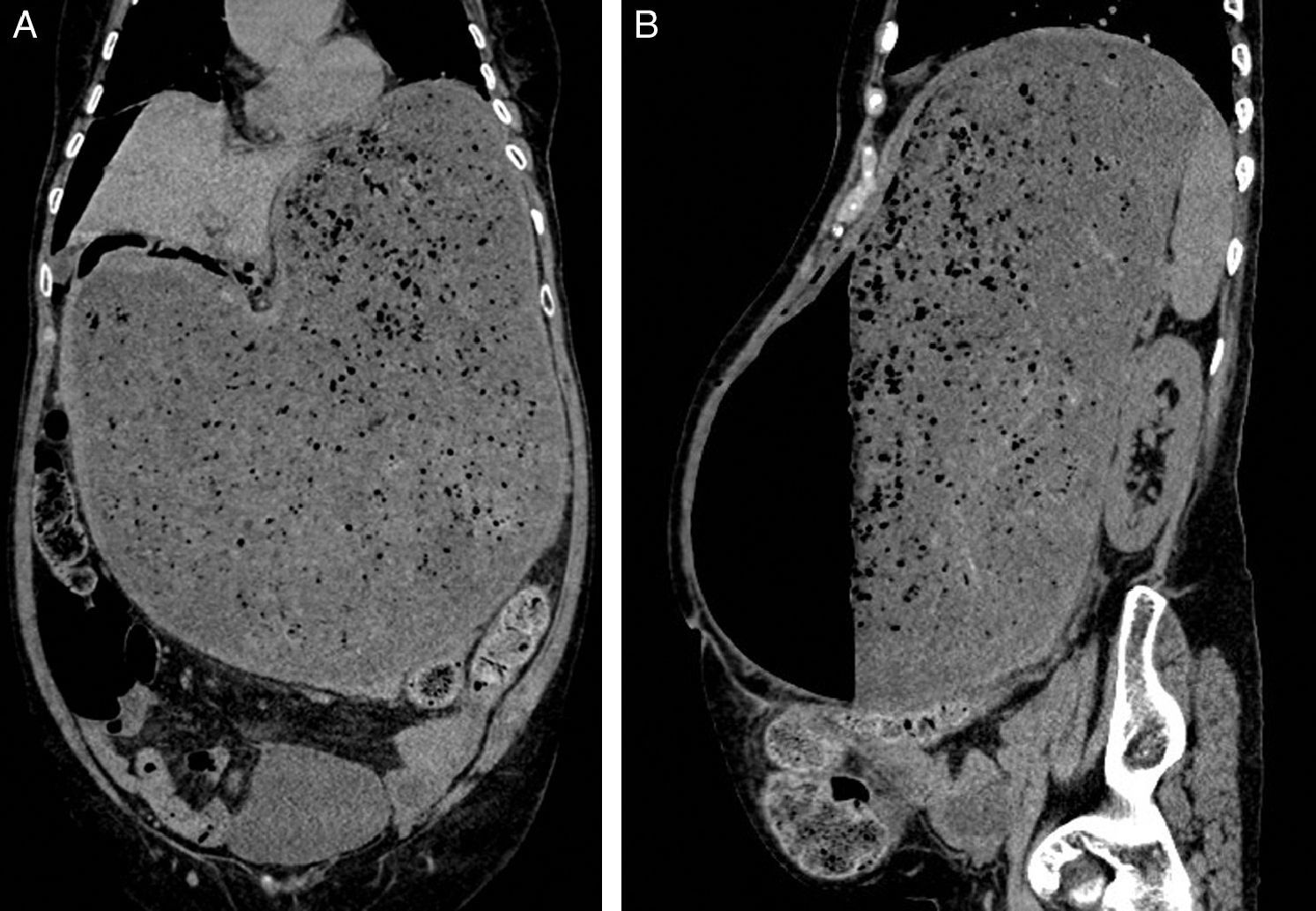
She was admitted to our department for sudden onset abdominal pain, accompanied by vomiting and absence of flatulence. On physical examination, she presented severe abdominal distension, tympanism and findings of peritoneal irritation. Blood tests found compensated metabolic acidosis, with normal full blood count, coagulation, C-reactive protein and basic biochemistry. Abdominal X-ray revealed severe gastric dilatation (Fig. 1), so an urgent abdominal computed tomography (CT) scan was requested (Fig. 2A and B), in which gastric distension secondary to complete pyloric stenosis and pneumoperitoneum was observed, with no clear perforation site.
Abdominal computed tomography images. (A) Coronal slice; (B) Sagittal slice: stomach very distended, containing food and air, with no passage of these to the duodenum observed, in relation to known pyloric stenosis. Pneumoperitoneum in upper abdomen and small amount of perigastric free fluid.
The patient underwent surgical treatment with total gastrectomy and bowel transit reconstruction by Roux-en-Y oesophagojejunostomy. We were unable to use the laparoscopic approach given the patient's severe gastric distension.
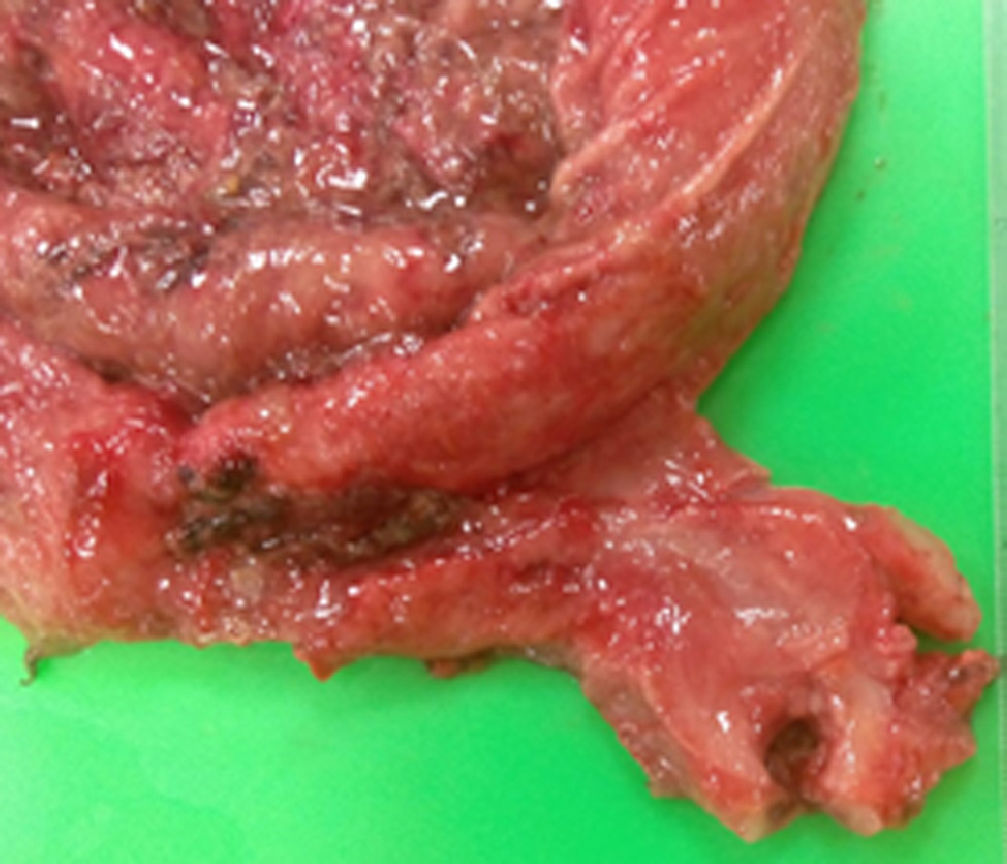
A stomach measuring 30cm at the longest axis was observed in the surgical specimen, with a thickened pylorus (Fig. 3); histopathology showed muscle fibres in bundles with an irregular arrangement and hypertrophy. No perforation site was found in the specimen, attributing the pneumoperitoneum to diffusion of air secondary to the severe gastric dilatation.
Hypertrophic pyloric stenosis in adults is a rare entity, with a wide range of symptoms (although it can be asymptomatic), producing dyspepsia, vomiting or even occlusive symptoms with pneumoperitoneum.1 Symptoms can appear between the ages of 14 and 85, with an average age of 50 years; it is more common in men, with an incidence of 3:1.2,3
The aetiology remains uncertain, but several hypotheses have been proposed, namely1,2,4:
- 1.
Primary causes: No apparent lesion identified:
- (a)
Neuromuscular incoordination due to changes in the Auerbach plexus or vagal hyperactivity.
- (b)
Protracted pylorospasm.
- (c)
Persistence of childhood stenosis. Most authors favour this theory, in which the disease remains latent and is reactivated by secondary factors such as inflammation, oedema, and spasm. Pyloric stenosis in adults and children presents similar anatomical and histopathological abnormalities, which supports this hypothesis.
- 2.
Secondary causes: Associated with gastric, pyloric or duodenal lesion, such as gastritis, peptic lesions or tumours.
Clinical symptoms are variable and rarely diagnostic, with predominantly abdominal pain, persistent vomiting, early satiety, anorexia, dyspepsia and weight loss.2,3 Diagnosis is mainly radiological (identifying a pyloric canal greater than 1cm) and endoscopic (where a narrow pylorus with smooth border is observed), although diagnostic confirmation is histological.
Asymptomatic patients or those with few symptoms do not require treatment, while patients with clinical evidence require surgery. Among the various surgical techniques used, pylorectomy with minimal gastrectomy seems to obtain better outcomes. Endoscopic treatment by means of pyloric dilation has also been described, but has a high rate of recurrence and should be used only in selected cases (patients with high surgical risk or who refuse surgery).2–4
Please cite this article as: Fernández Laso AB, Ganchegui Aguirre I, Campos Ruiz A, Urtasun Arlegui L, Gorroño Zamalloa I, Martinez Blazquez C, et al. Estenosis hipertrófica pilórica del adulto. Gastroenterol Hepatol. 2016;39:643–645.