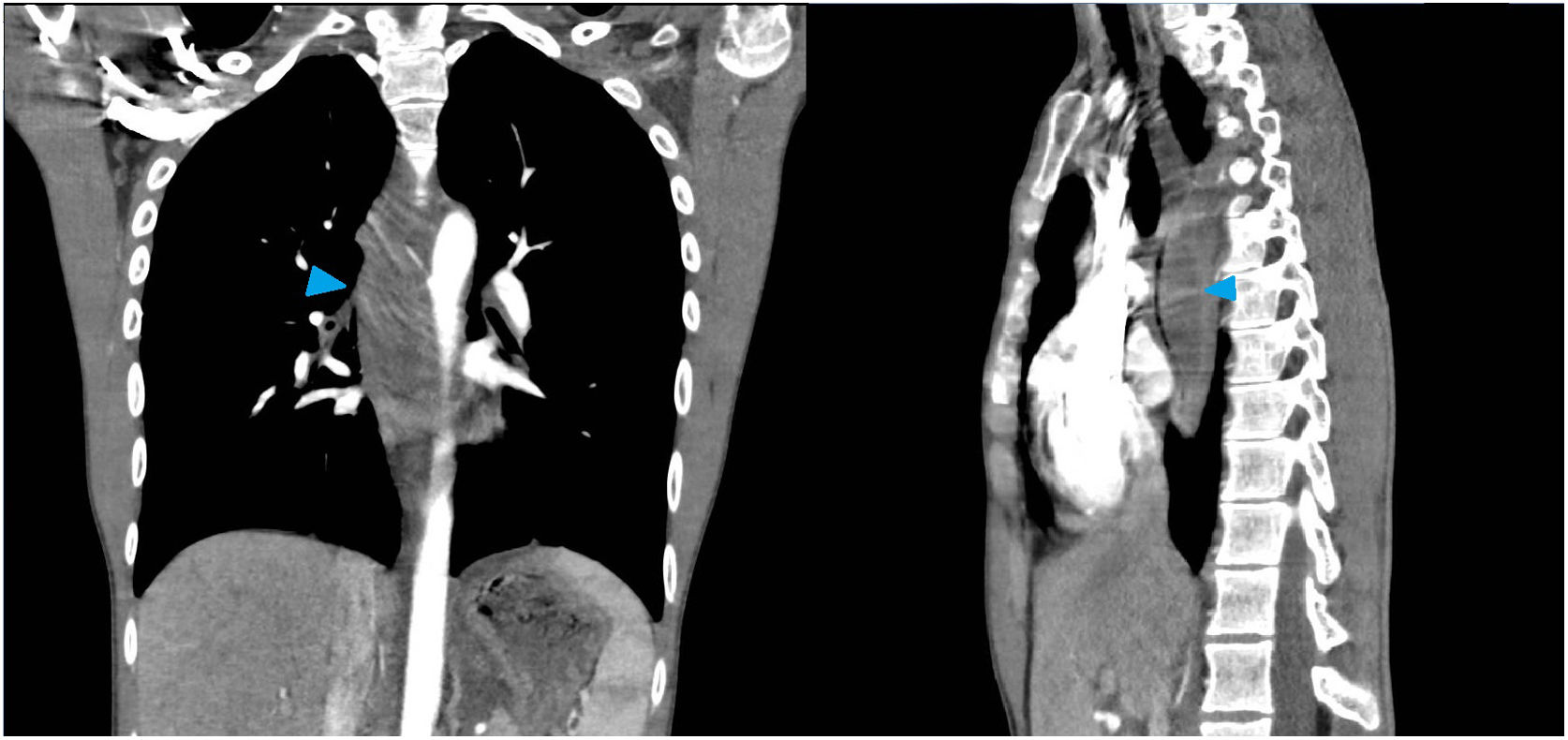
We present the case of a 21-year-old man with no prior history of note and no toxic habits who went in for epigastric pain, retrosternal chest pain, dysphagia and fever which had started three days beforehand. Laboratory testing revealed leukocytosis 16.41×103/μl (85 % neutrophils) and C-reactive protein 116mg/l. Given the clinical suspicion of pulmonary thromboembolism, this testing was complemented with an CT angiography scan, which showed an oesophageal duplication cyst complicated by superinfection and inflammatory changes suggestive of mediastinitis (Fig. 1).
CT angiography scan of the chest which revealed a prevertebral fusiform structure from T5 to T9, with an approximate size of 27×30×100mm, causing a mass effect on the oesophagus, compressing it and subjecting it to anterior and lateral displacement towards the right side, with an increase in the density of the mediastinal fat — all suggestive of a complicated oesophageal duplication cyst with superinfection and/or microperforation and associated mediastinitis.
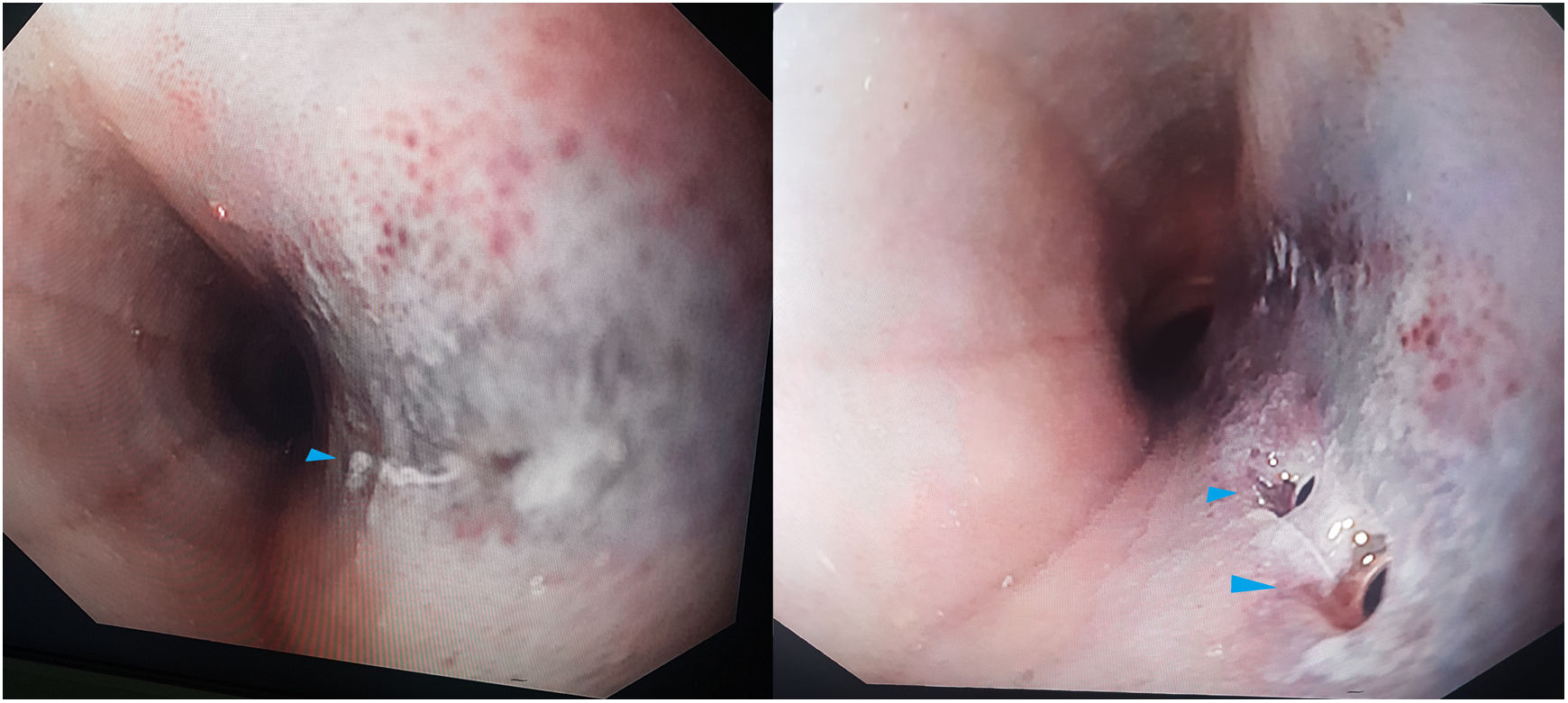
Given the unfavourable clinical course of the patient’s condition with increased pain, tachypnoea and tachycardia, it was decided to perform a thoracoscopy due to a suspicion of mediastinitis. No oesophageal cyst abnormalities or signs of frank mediastinitis were found; therefore, an intraoperative upper gastrointestinal endoscopy was performed which revealed two perforations with an ischaemic appearance in the oesophageal mucosa (Fig. 2) through which purulent cloudy fluid was spontaneously draining. Following confirmation of the absence of transmural perforation, they were biopsied and hydrostatically expanded to promote drainage. During admission, infectious-contagious disease, autoimmune disease, eosinophilic oesophagitis and malignancy were ruled out. The patient was discharged with outpatient monitoring after a follow-up endoscopy showed no significant findings.
Intramural oesophageal dissection constitutes laceration of the mucosa and submucosa layers with no transmural perforation of the oesophagus. Its aetiology remains unknown.1 On occasion, it may simulate other conditions such as a complicated oesophageal duplication cyst or oesophageal rupture.2 Initially, it is managed conservatively, but when this approach is insufficient, it is sometimes necessary to turn to endoscopic treatment3 or even surgical treatment.
Please cite this article as: Gómez Sánchez J, Alcaide Lucena M, Romera López AL, Mirón Pozo B. Perforación esofágica idiopática que simula quiste de duplicidad esofágico complicado. Gastroenterol Hepatol. 2019;42:634–635.