Intestinal involvement in tuberculosis is rare, but when it occurs, the ileocaecal area is most often affected.1 The incidence of tuberculosis is increasing, however, as a result of HIV, chronic renal disease, immunosuppressive therapy and immigration.1,2 It is the great imitator, and is a diagnostic challenge.1
We present the case of a 67-year-old Spanish woman with a history of hypothyroidism and chronic constipation, who had been admitted for abdominal pain three times in the previous 2 months. She reported a 5-day history of postprandial abdominal pain, vomiting and constipation. The patient was afebrile, with unquantified weight loss.
On examination, her abdomen was slightly distended, tympanitic, with generalised pain, no signs of peritoneal irritation, no masses or organomegaly and diminished bowel sounds.
In the complementary examinations, blood tests were normal, while an abdominal X-ray showed dilatation of small bowel loops, with air-fluid levels. Abdominal scan revealed dilatation of the terminal jejunum and ileum with caecal wall thickening, and a change in calibre at the level of the terminal ileum, with small lymphadenopathies in the adjacent fat and root of the mesentery. Colonoscopy showed an oedematous and deformed ileocaecal valve with minute fibrinous ulcers, and erythematous mucosa and small aphthoid lesions in the last few centimetres of the terminal ileum, from which biopsies were taken.
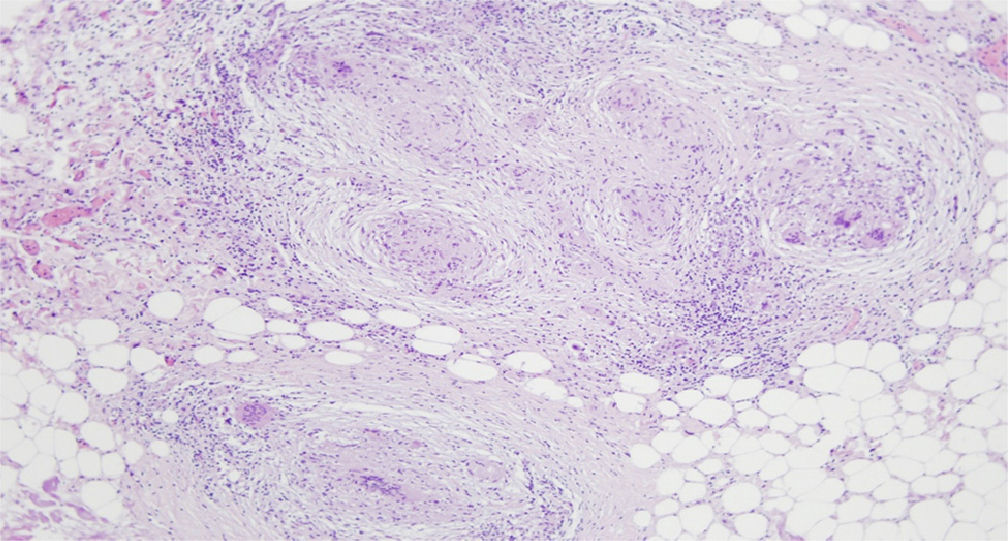
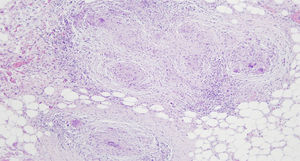
Due to the patient's clinical deterioration, an exploratory laparotomy was performed, which found multiple peritoneal implants with a miliary appearance, with segmental thickening of the ileum (Fig. 1). The histological result of the ileal biopsies was chronic necrotising granulomatous ileitis, and peritoneal implants and mesenteric lymphadenopathy of necrotising granulomas with caseous necrosis (Fig. 2). Ziehl–Neelsen staining and culture were negative, and a polymerase chain reaction (PCR) test was positive for M. tuberculosis. The Mantoux test was positive, even though the patient had been BCG vaccinated in childhood, but the interferon-gamma release assay was also positive, suggesting latent tuberculosis. Chest X-ray was normal and the HIV and hepatotropic virus studies were negative.
The patient started tuberculostatic treatment with quadruple therapy, with gradual improvement.
Diagnosing intestinal tuberculosis in a immunocompetent patient such as ours is challenging, and even more so when there is no evidence of lung disease. The lungs are involved in only 20% of cases of intestinal tuberculosis.1 Peritoneal tuberculosis accounts for between 1%-3% of all cases of tuberculous disease.3
In our case, the disease commenced with sub-occlusive symptoms; these should be considered in the differential diagnosis of chronic abdominal pain with ileocolic lesions and suspected on the basis of endoscopic findings. Colonoscopy gives access to the colonic and ileal mucosa, facilitating the histological study with the finding of necrotising granulomas, while microbiology, using different techniques such as staining, culture and PCR, provides diagnostic confirmation. Ziehl–Neelsen staining is positive in 35–60% of cases.4 Biopsy culture takes between 3 and 8 weeks, and the result is often negative.5 PCR assay of biopsy samples, which has a sensitivity of 86% and a specificity of 95–100%,6 is considered the most reliable test, as proved to be the case in our patient.
The differential diagnosis was made with Crohn disease, intestinal adenocarcinoma, lymphoma, enteritis due to Yersinia, amoebiasis, histoplasmosis, acute appendicitis and sarcoidosis.7
Please cite this article as: Sancho L, Pinto P, García F, González PI, Barrio J, Alcaide N, et al. Tuberculosis intestinal y peritoneal en paciente no inmunodeprimido. Gastroenterol Hepatol. 2016;39:645–646.