Intussusception (I) is caused by the telescoping or invagination of a generally proximal portion of intestine (intususceptum) into the adjacent, more distal portion of the intestinal lumen (intususcipiens). The concomitant displacement of the mesentery of the telescoped portion can cause, in addition to the obstruction of transit, vascular compromise, which can lead to intestinal ischaemia. Ileocolic I is uncommon in adults (5%), in whom it is an infrequent cause of mechanical obstruction (1–5%).1
We present the case of a 20-year-old man who was treated in the Emergency Department for a 1-day history of rectal bleeding and abdominal pain in the right flank. Examination revealed a distended and tympanic abdomen, with pain and guarding on palpation in the right lilac fossa. Notable in the blood tests were leukocytes of 15,640×109/l with neutrophilia, and the abdominal X-ray showed dilated loops of small bowel with the absence of gas distally. The subsequently performed abdominal ultrasound and computed tomography (CT) showed ileocolic II secondary to a lipoma of the ileocaecal valve which was causing intestinal obstruction (Fig. 1A and B), and therefore emergency surgery was indicated. An exploratory laparoscopy was performed, during which the intussusception was localised. Following unsuccessful reduction manoeuvres, a right colectomy with extracorporeal end-to-side mechanical anastomosis was carried out (Fig. 1C and D). The patient had no postoperative complications and was discharged 7 days after the procedure. The histopathology study showed ileocolic intussusception with ileal transmural ischaemia secondary to Meckel's diverticulum (MD).
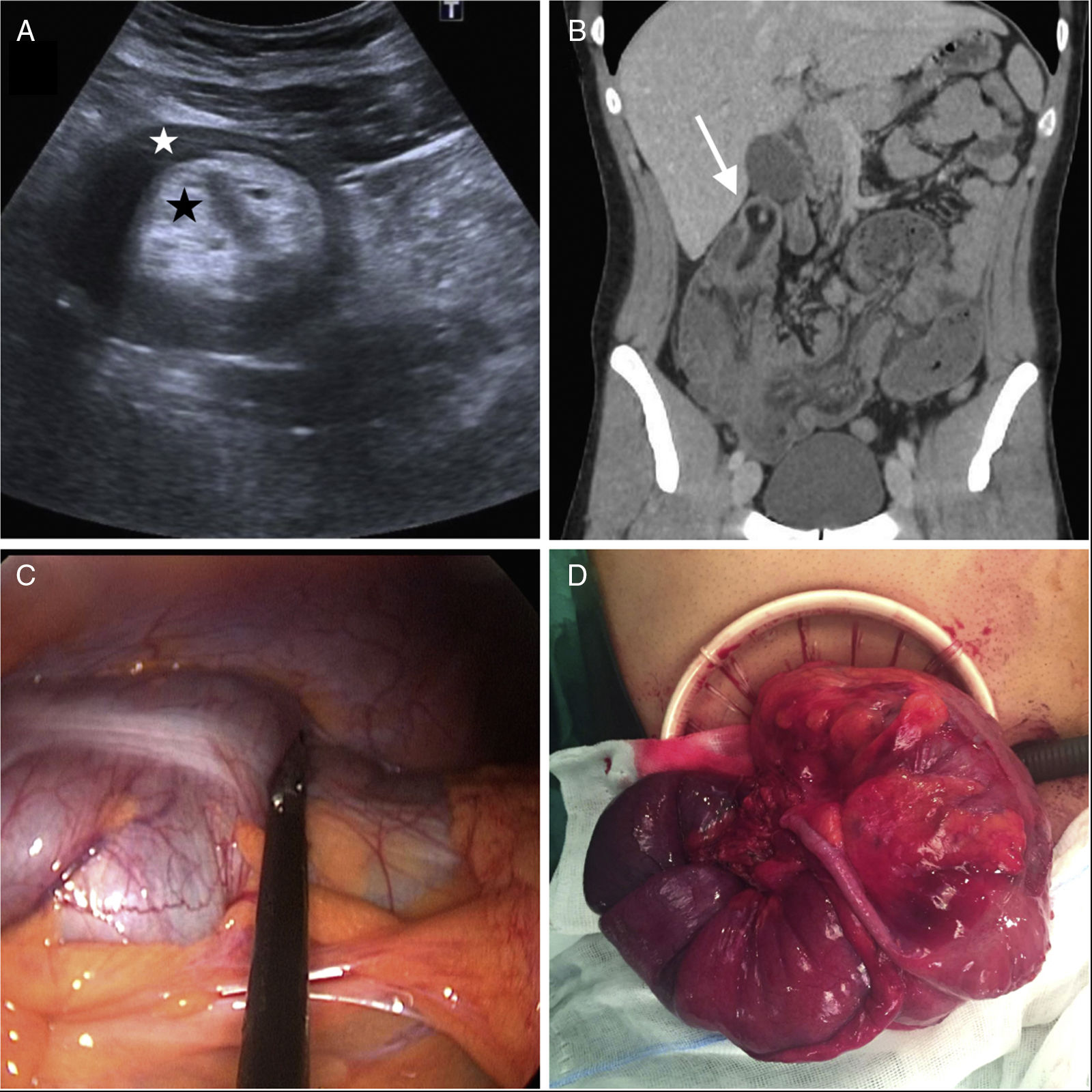
(A) Ultrasound target sign on a transverse section: hypoechogenic (white star) and hyperechogenic (black star) concentric bands. (B) Coronal CT section: hypodense tumour measuring 43mm at the apex of the intussusception consistent with lipoma of the ileocaecal valve (white arrow). (C) Image of the laparoscopic surgery of the ileocolic intussusception. (D) Extracorporeal image of the ileocolic intussusception.
Intussusception (I) was first described by Barbette (1674) and later named as such by Hunter (1789). Intussusceptions (I) are classified according to location and may be ileoileal, enterocolic (ileocolic if the head of the intussusception is in the ileum and ileocaecal if the head of the intussusception is situated in the caecum or in the valve itself), and colocolic.2 In contrast to the paediatric population, in adults, 70–90% of cases are secondary to an intraluminal lesion which acts as the head of the intussusception.3 Around 20–50% of these are malignant in origin, ranging in frequency according to localisation (70% in colocolic cases compared to 31% in ileal cases).4 The presence of MD as a cause of ileocolic intussusception in adults is uncommon,5 since, as this type is localised 60–80cm from the ileocaecal valve, they require a very extensive intususceptum segment in order to occur. MD is the most common congenital malformation of the gastrointestinal tract (1–4%), but associated complications occur in only 16% of carriers. The most common is gastrointestinal bleeding, which usually occurs in children. The characteristic clinical triad of II in children (abdominal pain, palpable mass and rectal bleeding) occurs less frequently in adults,6 who for the most part first present with subacute/chronic clinical signs and symptoms of abdominal pain and/or symptoms of intestinal obstruction. Other possible, but less common complications of MD are diverticulitis, torsion or perforation.7 Abdominal ultrasound can provide a diagnosis in 60% of cases of I,5 identifying the characteristic target sign on transverse section and the pseudokidney sign viewed on longitudinal section (multiple thin, concentric, hypoechoic and echogenic bands).3 CT is the diagnostic test of choice3 as it enables the intussusception to be localised and its aetiology to be established. Moreover, it is useful for the detection of associated complications, such as intestinal ischaemia or perforation.
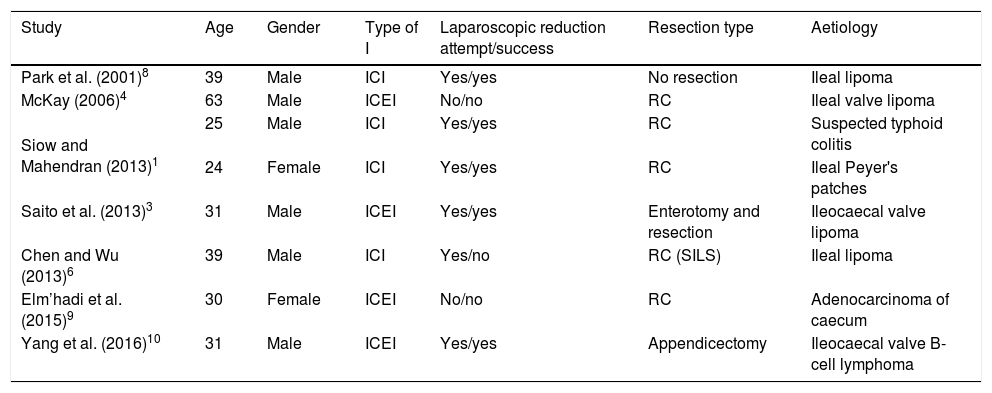
Surgery is the treatment of choice for enterocolic II in adults and consists of the resection, with or without prior reduction, of the involved segment.1 Reduction avoids the resection of long segments of intestine but can lead to delayed perforations or in tumour dissemination on account of the manoeuvres performed.2 Consequently, it is only indicated after malignancy is ruled out and tissue viability can be confirmed. If these two requirements are not met, or in the case of technical inability, the treatment of choice is en bloc resection. Emergency surgery should be considered in view of signs and symptoms of intestinal occlusion, clinical deterioration of the patient and when intestinal ischaemia or perforation is suspected. Alternatively, surgery can be postponed so that a colonoscopy can be performed5 and an appropriate surgical strategy suggested which facilitates a subsequent laparoscopic approach. However, in spite of its advantages, the use of laparoscopy in enterocolic II intussusception in adults is practically anecdotal, with 8 cases described in the current literature (Table 1). In the majority of these cases, laparoscopic reduction prior to resection was performed successfully, and right colectomy with extracorporeal anastomosis was the technique most used. None of the cases required conversion to open surgery, and the postoperative course was good in all cases.
Enterocolic intussusceptions treated by laparoscopy.
| Study | Age | Gender | Type of I | Laparoscopic reduction attempt/success | Resection type | Aetiology |
|---|---|---|---|---|---|---|
| Park et al. (2001)8 | 39 | Male | ICI | Yes/yes | No resection | Ileal lipoma |
| McKay (2006)4 | 63 | Male | ICEI | No/no | RC | Ileal valve lipoma |
| Siow and Mahendran (2013)1 | 25 | Male | ICI | Yes/yes | RC | Suspected typhoid colitis |
| 24 | Female | ICI | Yes/yes | RC | Ileal Peyer's patches | |
| Saito et al. (2013)3 | 31 | Male | ICEI | Yes/yes | Enterotomy and resection | Ileocaecal valve lipoma |
| Chen and Wu (2013)6 | 39 | Male | ICI | Yes/no | RC (SILS) | Ileal lipoma |
| Elm’hadi et al. (2015)9 | 30 | Female | ICEI | No/no | RC | Adenocarcinoma of caecum |
| Yang et al. (2016)10 | 31 | Male | ICEI | Yes/yes | Appendicectomy | Ileocaecal valve B-cell lymphoma |
RC: right colectomy; ICI: ileocolic intussusception; ICEI: ileocaecal intussusception; SILS: single-incision laparoscopic surgery.
In our opinion, given that a laparoscopic approach makes it possible to achieve a complete exploration of the peritoneal cavity, which confirms the diagnosis and rules out associated complications as well as enabling the patient to achieve early postoperative recovery,3 it should be considered as a first therapeutic option in enterocolic II in adults, provided that it is possible based on patient characteristics and the extent of intestinal dilatation.
Please cite this article as: Payá Llorente C, Martínez Pérez A, Bernal Sprekelsen JC, Sebastián Tomás JC, Armañanzas Villena E. Cirugía laparoscópica en el tratamiento de la invaginación entero-cólica en el adulto: a propósito de un caso y revisión de la literatura. Gastroenterol Hepatol. 2018;41:255–257.