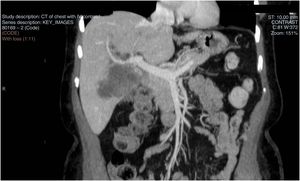
This was a 67-year-old woman with hypothyroidism and dyslipidaemia who was admitted with a two-day history of symptomatic jaundice. She reported repeated symptoms of biliary colic over the previous four months, as well as anorexia and weight loss. She did not have pyrexia and there was no other relevant history. Abdominal ultrasound showed dilatation of the intrahepatic bile duct, gallbladder with cholelithiasis and adjacent poorly defined predominantly echogenic pseudonodular liver mass suggestive of hepatic phlegmon. Investigations were completed with a CT of the abdomen (Fig. 1), which showed a solid mass in liver segments IV and V, 6×8×6.2cm in size, showing no plane of separation with the upper part of the gallbladder and causing amputation of the bile duct at the level of the common hepatic duct, suggestive of cholangiocarcinoma with liver and gallbladder invasion infiltrating the origin of the right hepatic artery and portal vein. There was no radiological evidence of liver disease. Liver MRI and MR cholangiogram showed a solid mass enveloping the upper two thirds of the gallbladder, liver segments IV and V, the proximal bile duct, the common hepatic duct and the bifurcation, with moderately high heterogeneous signal in T2 and low in T1, restriction in diffusion sequences and late heterogeneous peripheral uptake in the dynamic study, compatible with probable biliary carcinoma. Blood tests showed elevation of cholestasis parameters and marker Ca 19.9 of 193.5U/ml, with normal CA 125, CEA and alpha-fetoprotein markers. Ultrasound-guided biopsy revealed poorly differentiated epithelial neoplasia with morphological and immunohistochemical findings consistent with pure squamous cell carcinoma, showing intense immunoexpression for p40, weak positivity for Gata 3, CK19 and focal for CK7, negative result for CK20, TTF1 and OCHE5, p53 positive in 90% and Ki 67 in around 15-20%. Further investigations included oesophagogastroduodenoscopy and gynaecological and ENT screening, which ruled out the tumour being of metastatic origin. CT scanning of neck/chest and abdomen/pelvis for spread of the cancer was negative. The patient was discussed at the multidisciplinary oncology committee; surgical intervention was ruled out as it was considered unresectable due to vascular invasion, and it was decided to opt for right transparietohepatic and left external-internal drainage. The drainage was effective, achieving normalisation of bilirubin levels, but it was complicated by bile leak and infected biloma. The patient made poor progress and did not respond well to the treatment. She died three months later as a consequence of biliary sepsis.
Cholangiocarcinoma is the most common cancer of the bile duct, with an annual incidence of less than six cases/100,000 people. Worldwide, there has been a general decrease in the incidence of extrahepatic cholangiocarcinoma and an increase in intrahepatic cases. The mortality rate is high due to its aggressive nature, the usually late diagnosis and the fact that it is refractory to treatment.1
The majority of biliary tract tumours are adenocarcinomas. Squamous cell carcinomas in the biliary tract are extremely rare, the incidence being less than 1.4%.2 The pathogenesis of this type of cancer is unknown, although some have suggested a relationship with chronic biliary inflammation, congenital biliary cysts, biliary lithiasis and clonorchiasis.3,4 The possible origins of squamous cell carcinomas include the transformation of adenocarcinomas, the derivation of a metaplastic squamous epithelium, a squamous ectopic epithelium or undifferentiated basal cells.5
Given the low incidence of cholangiocarcinomas containing squamous cells, the diagnostic, prognostic and therapeutic implications have not been fully established and are based on the cases reported in the literature.3–5 Prognosis is poor due to the aggressive nature of the cancer; progression is rapid, with invasion of the liver parenchyma and metastatic spread, and survival time is short.3,4 We do not have standardised treatment strategies. Surgical resection is recommended as the only curative treatment available, with or without chemotherapy.3 Whether it is resectable or not depends on the biliary spread of the tumour, invasion of the portal vein and the hepatic artery and metastatic involvement.5 Radiotherapy seems to be ineffective, and the recommended chemotherapy is based on platinum regimens, such as gemcitabine plus oxaliplatin or cisplatin, similar to that used in adenocarcinomas. One case of good response to treatment with S-1 and cisplatin has been reported.3
Please cite this article as: Delgado Maroto A, Barrientos Delgado A, Lázaro Sáez M, Hallouch Toutouh S, Práxedes González E. Carcinoma primario de células escamosas del conducto hepático común: a propósito de un caso. Gastroenterol Hepatol. 2019;42:436–437.