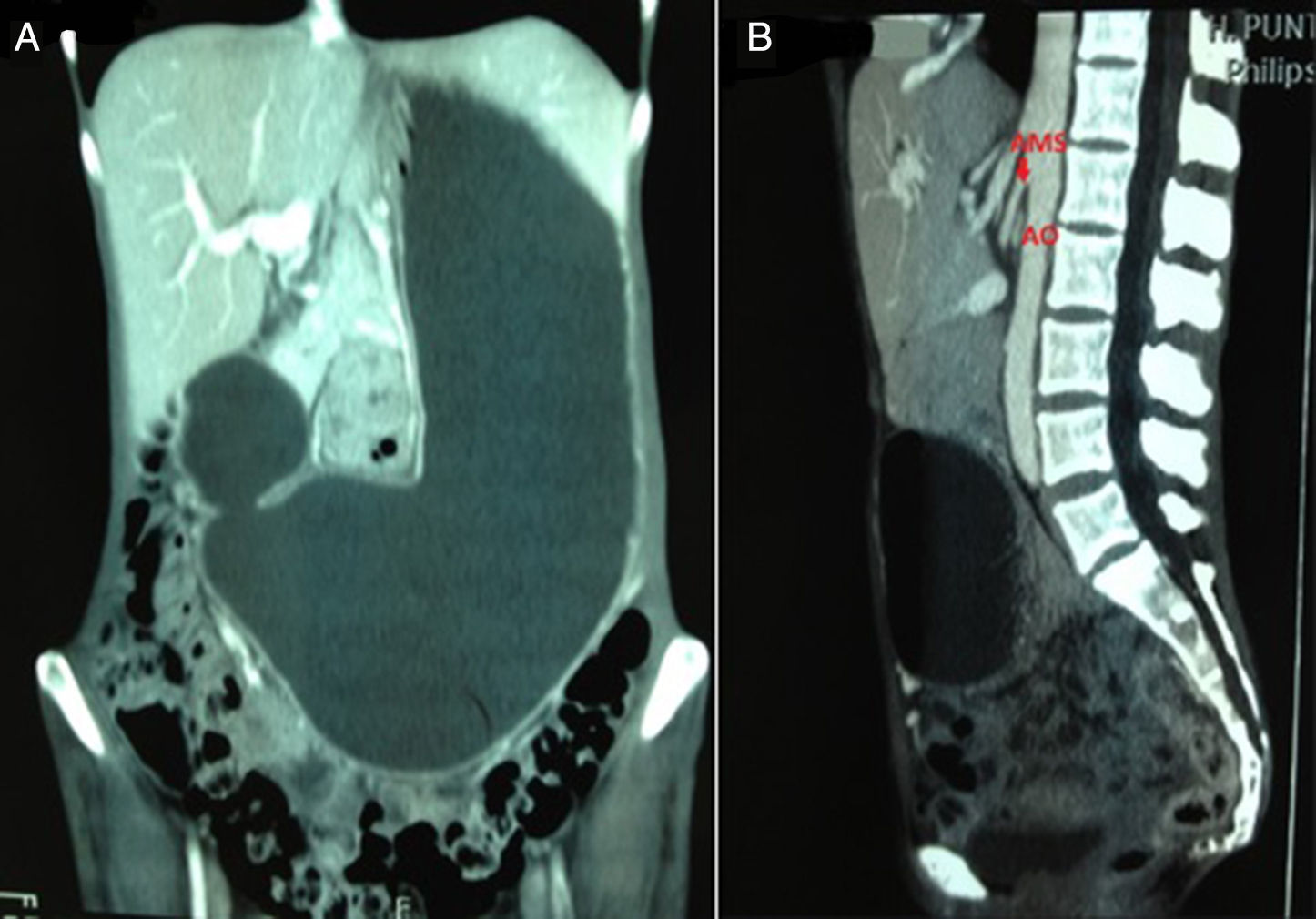
We present the case of a 43-year-old woman with a history of neurofibromatosis who came in for symptoms of abdominal pain, 15kg of weight loss, abdominal distension and vomiting of several months evolution. The physical examination found cachexia and diffuse abdominal distension. The computed tomography (CT) revealed massive gastric distension with obstruction of the third part of the duodenum (Fig. 1A), related to decreased space between the aortic and superior mesenteric arteries, with the aortomesenteric angle being less than 25° (Fig. 1B), data very suggestive of superior mesenteric artery syndrome (SMAS). A nasogastric tube was inserted, presenting a large volume of output. The gastroscopy reported oesophagitis and a stomach with abundant contents that, upon aspiration, showed very bloody mucous related to gastric stasis. Conservative treatment with enteral and parenteral nutritional supplements was started, as well as placement of the patient in left lateral recumbent position, without improvement. Therefore, a gastrojejunostomy was performed. After surgery, the patient progressed well, ceased vomiting and gained 7kg in the first 4 months and 12kg in the first year.
SMAS was described by Rokitansky in 18611 and named by Wilkie in 1927, being known since then as Wilkie's Syndrome.2 Its frequency is very low, with an incidence of 0.2% found across 6000 radiological studies.1 Its incidence is higher in adolescent girls and young adults, although it can occur at any age.3
It originates from duodenal compression caused by the superior mesenteric artery (SMA) and the abdominal aorta (AO). In normal anatomy, the third part of the duodenum passes anterior to the AO and then the SMA at the level of the third lumbar vertebra. These three structures, along with the left renal vein, are surrounded by pads of mesenteric fat and lymph nodes. In patients with SMAS, the aortomesenteric angle is less than 25° (normal value: 38°–65°), and the distance between the two arteries is less than 8mm (normal value: 10–28mm).3–5 On occasions, this syndrome is also associated with compression of the left renal vein, causing what is called nutcracker syndrome (haematuria and severe proteinuria).3
The common trigger for this disease is weight loss for various reasons, which can be classified as3,6: consumptive syndromes (AIDS, cancer, widespread burns, endocrine diseases, intestinal malabsorption); eating disorders (anorexia nervosa); major operations (including bariatric surgery); severe traumas (head, multiple traumas) and spinal diseases (deformities).6,7
Patients may complain of reflux, with the endoscopic study revealing oesophagitis and/or retention gastritis, early postprandial abdominal distension, vomiting bile, nausea and hyporexia. They may report major weight loss recently or improvement of symptoms when lying on the left side or when bringing the knees close to the chest, since these postures alleviate the tension between the AO and SMA. The analytical findings are nonspecific, although there may be hydroelectric changes consistent with the severity of the symptoms.6,8
The differential diagnosis of SMAS includes other causes of acute abdominal pain such as intestinal obstructions of other origins, mesenteric ischaemia and gastro-oesophageal reflux disease. It is difficult to distinguish these symptoms from other types of intestinal obstruction since the presentation and laboratory data are identical. Another origin of intestinal obstruction may be considered where there is a history of neoplasm, radiotherapy, inflammatory bowel disease or prior abdominal surgeries.
The diagnosis is established via imaging techniques. Duodenal obstruction due to abrupt stenosis of the third part with proximal duodenal and gastric cavity distension can be identified in a barium test. SMAS is definitively diagnosed via direct visualisation on CT, magnetic resonance, ultrasound or conventional angiogram of the decreased aortomesenteric angle based on the previously-described parameters.6,8
The treatment for SMAS is generally conservative via replenishing electrolytes, and parenteral, enteral or combined diet.8 Placing the patient in left lateral recumbent position to facilitate gastric emptying is also recommended. Psychological support is important in certain cases, such as those motivated by anorexia nervosa. Acute episodes tend to respond to conservative treatment, but in chronic cases, surgical treatment is often needed. Surgery would be indicated after the failure of conservative management, in chronic cases with progressive weight loss and duodenal dilation, as in this case, and in patients who develop complicated ulcers secondary to biliary stasis and reflux.6,8
The proposed surgical interventions for treatment include: liberation of the ligament of Treitz (Strong procedure), gastrojejunostomy and duodenojejunostomy. The Strong procedure maintains the integrity of the gastrointestinal tract, but it has a failure rate of 25%. Gastrojejunostomy allows for gastrointestinal decompression but does not alleviate duodenal compression. Therefore, gastrointestinal symptoms may persist and lead to the onset of blind loop syndrome or recurrent peptic ulcers. Duodenojejunostomy is the procedure of choice, with a success rate exceeding 90%. Gastroparesis after surgical correction is a common problem related to gastric and duodenal atony. Although there is little information about its medical management in the literature, treatment with prokinetics may be attempted.4,6,8,9
The rate of complications in relation to upper gastrointestinal tract obstruction is high, in particular aspiration pneumonia, gastric perforation and cardiovascular collapse. Therefore, the diffusion of the pathophysiology of this condition would allow for a higher rate of suspicion, leading to greater prevention, diagnosis and early treatment.4,6
Please cite this article as: Ruiz Padilla FJ, Mostazo Torres J, Vílchez Jaimez M. Gran distensión gástrica en relación con síndrome de la arteria mesentérica superior o síndrome de Wilkie. Gastroenterol Hepatol. 2017;40:581–583.