Wilson's disease (WD) is a hereditary disorder caused by mutations of the ATP7B gene in chromosome 13, in which the defective biliary excretion of copper causes it to accumulate primarily in the liver and brain.1 We present the case of a female patient with acute liver failure (ALF) due to WD.
This case concerns a 15-year-old female patient with no personal or family history of interest on treatment with oral contraceptives for some months prior, with slightly increased liver enzyme levels at baseline (ALT 89IU/l, GGT 80IU/l). She occasionally took non-steroidal anti-inflammatory drugs and received erythromycin on the days prior to her presenting complaint due to accidental trauma, with the development of haematoma that required drainage and the incidental finding of coagulopathy (INR 1.65), for which she was admitted to her hospital.
Clinically asymptomatic with no neurological or behavioural abnormalities (good academic record), she presented three normal haematopoietic series: INR 1.71; albumin 3mg/dl; total bilirubin (TBIL) 1.84mg/dl (direct bilirubin 1.22mg/dl); AST 112IU/l; ALT 219IU/l; GGT 351IU/l and polyclonal hypergammaglobulinaemia. Studies on hepatotropic viruses, autoimmunity, immunoglobulins, coeliac disease and thyroid hormones were normal. Serum copper was 36mcg/dl (normal 80–155mcg/dl) and ceruloplasmin 2.97ng/dl (normal 25–63ng/dl). The patient had no Kayser–Fleischer rings and the abdominal ultrasound revealed no pathological findings.
Progressive deterioration of liver function was observed at two weeks with a negative Coombs test for haemolytic anaemia, thrombocytopenia; INR 2.94; albumin 2.6mg/dl; TBIL 8.35mg/dl; ascites and splenomegaly. The patient was referred to our Liver Transplant Unit for observation and management. Upon admission, she underwent: 24-hour urine copper test of 805mcg/dl (normal up to 60mcg/dl) and a positive D-penicillamine challenge test.
Her liver function further deteriorated in the subsequent 48h: INR 3.11; TBIL 25.3mg/dl (432μmol/l); leukocytes 10.2×109/l; albumin 26g/l; AST 110IU/l, preserved renal function, MELD score of 30 points and WD prognostic index of 13 points. In light of these findings, she was admitted to the ICU and added to the emergency liver transplant list.
At 24h, her renal function deteriorated (serum creatinine: 1.30; MDRD-6: 55ml/min/1.73m2) and an orthotopic liver transplantation was performed without any complications. Upon examination of the liver explant, cirrhosis and 2457ng/g of copper (normal range 10–40ng/g) in the liver tissue were observed. The subsequent genetic study identified homozygosity of mutations c.1285+5G>7 and c.3451c>T in the ATP7B gene.
The diagnosis of WD is complicated and can often be delayed owing to the broad clinical variability of this disease. WD should be considered when treating any young patient with acute hepatitis. Symptoms may resolve spontaneously or, in a minority of cases, may give rise to rapid deterioration and ALF, particularly in young women (female/male ratio: 4:1).2
WD accounts for 6–12% of all patients with ALF who are referred for emergency liver transplantation.3 Although most patients already have cirrhosis of the liver, the clinical manifestation is acute and very rapidly deteriorates to liver and kidney failure. Without treatment, the mortality rate is almost 95%. In ALF due to WD, pharmacological treatment is rarely effective, primarily because of how long it takes to eliminate the copper accumulated in the body: liver transplantation is the only curative treatment option in such cases.4
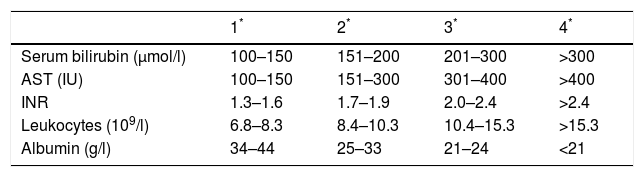
In our case, the diagnosis of WD was relatively certain given the patient's history, despite a lack of biopsy or genetic testing. Deciding when to perform the liver transplantation was the most complicated aspect of the treatment given the lack of published studies in this regard. The largest series was published by Dhawan et al.,4 who developed a prognostic index based on five analytical parameters, with a score of more than 11 points representing a high likelihood of death without a liver transplant (Table 1).5
Our patient scored 13 points when she was added to the liver transplant list. In our opinion, the drafting of simple criteria to define when emergency transplantation is indicated is essential. Dhawan's score may be very useful in such cases.
Finally, we feel that a liver disease study should be conducted if transaminase levels are elevated. This should include an assessment of plasma and urine copper levels and ceruloplasmin at baseline.
Please cite this article as: Estrada León I, Guiberteau Sánchez A, Vinagre Rodríguez G, Blanco Fernández G, Pérez Civantos D, Gaspar Blázquez MJ, et al. Trasplante hepático urgente por fallo hepático agudo por enfermedad de Wilson. Gastroenterol Hepatol. 2019;42:392–393.