Belching may be defined as audible or silent oral expulsion of boluses of gas from the upper gastrointestinal tract.1–3 It is a normal phenomenon in most individuals, but may represent a medical problem if it is excessive or hard to control.
Physiologically, belching relieves the accumulation of gas inside the stomach. The air accumulated in the stomach is expelled towards the oesophagus, due to spontaneous relaxation of the lower oesophageal sphincter (LOS), which allows the air to pass into the oesophagus. There, it stimulates secondary relaxation of the upper oesophageal sphincter (UOS), thereby allowing the air to pass into the mouth.1,3 In supragastric belching, air is swallowed and belched immediately without reaching the stomach, or originating from it. There are 2 reported mechanisms by which it may occur1–3:
- −
“Air suction”. This is the more common mechanism. In it, the diaphragm generates increased negative intrathoracic pressure, which, together with a relaxation of the UOS, causes the air to pass towards the oesophagus and be expelled immediately, resulting in a belch.
- −
An increased pressure in the pharynx together with a decreased pressure in the oesophagus. This is due to contractions of the base of the tongue, which cause a contraction of the pharynx without a simultaneous contraction of the oesophagus.
It has been suggested that supragastric belching may be due to an involuntary response to different feelings of discomfort for the patient (abdominal distension/bloating), which end up becoming uncontrolled. It has been demonstrated that it does not occur during sleep and that the patient belches less if distracted. Consequently, supragastric belching may be a learned behaviour.1,2 Other studies have postulated that a certain amount of supragastric belching may be considered normal, and that excessive supragastric belching is usually associated with gastro-oesophageal reflux disease (GORD) and sometimes associated with oesophageal hypomotility.4
Supragastric belching has been demonstrated in patients with GORD or rumination syndrome, and should be distinguished from aerophagia, in which the gas swallowed goes to the stomach.1,2 It may be accompanied by a feeling of reflux and pyrosis, especially with fluids.1
We present the case of a patient who was admitted to our hospital, transferred from another hospital where she was admitted due to signs and symptoms of continuous belching for the last 2 months which had been increasing. Her signs and symptoms started following an episode of uncontrollable vomiting for several days. It was sometimes accompanied by vomiting after eating and pyrosis. The situation limited the patient's daily activities, since she could not control the belching. She had undergone an oesophagogastroduodenal transit study; upper gastrointestinal endoscopy; and oesophageal, antral and duodenal biopsies. These were normal. Her laboratory testing with a complete blood count, thyroid profile, IgA, ATG, total IgA and iron metabolism was normal. She had received treatment with omeprazole, H2 antagonists, prokinetics, antacids, diazepam, haloperidol, clorazepate dipotassium and antiflatulents with no improvement.
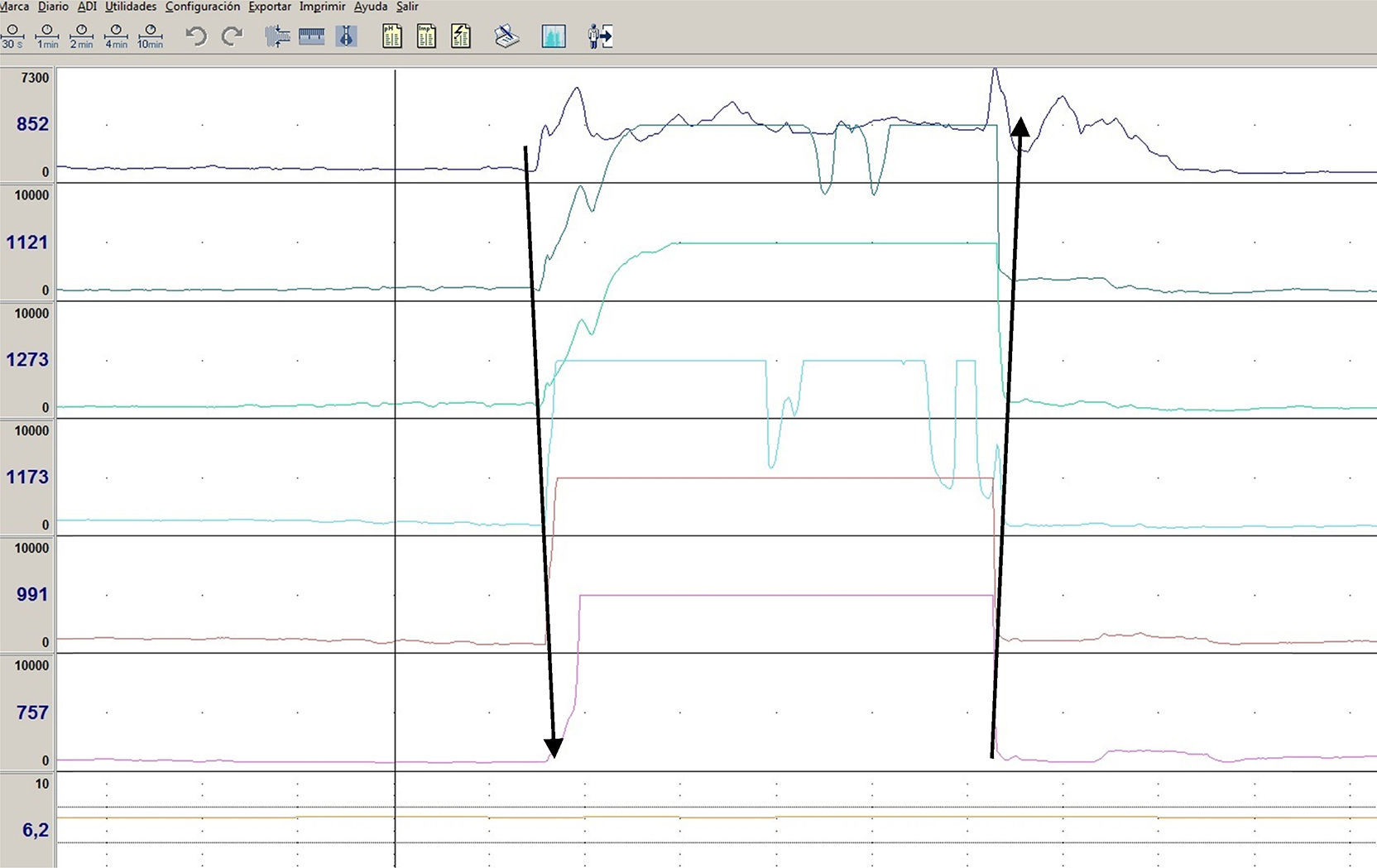
While she was admitted, the patient was found to have no belching while sleeping or speaking, and to belch less when distracted and more when stressed. She was examined using a head CT scan, a hydrogen breath test for lactose and fructose, gastric emptying scintigraphy, and impedancemetry. The results of the head CT scan, hydrogen breath tests, and scintigraphy were normal. Impedancemetry demonstrated supragastric belching (Fig. 1).
A diagnosis of supragastric belching should be suspected in patients with repetitive belching that ceases when they are speaking and decreases when they are distracted.1 It may be associated with pyrosis, abdominal or chest pain, dysphagia, or a feeling of distension.4 The leading test that enables diagnosis is impedancemetry, which has a typical pattern in which there is an increase in impedance that starts at the proximal channel and advances towards the most distal channel, followed by a return to baseline from the distal channel to the proximal channel.1,2
Treatment is based on different steps: (1) explaining the nature of the symptoms to the patient, (2) addressing it as a behaviour disorder using behaviour therapy and (3) ensuring that the patient has speech therapy in which he or she learns exercises to control the entry of air into the oesophagus.1,3,5 The use of medication is not recommended, with the exception of baclofen, which may be useful in selected cases.6 In our case, the patient was referred to the children's mental health and rehabilitation unit to address her existing behaviour disorder.
Please cite this article as: Salazar Quero JC, Moya Jiménez MJ, Rubio Murillo M, Roldán Pérez S, Rodríguez Martínez A, Valverde Fernández J. Eructos supragástricos. Una entidad a conocer. Gastroenterol Hepatol. 2017;40:396–397.