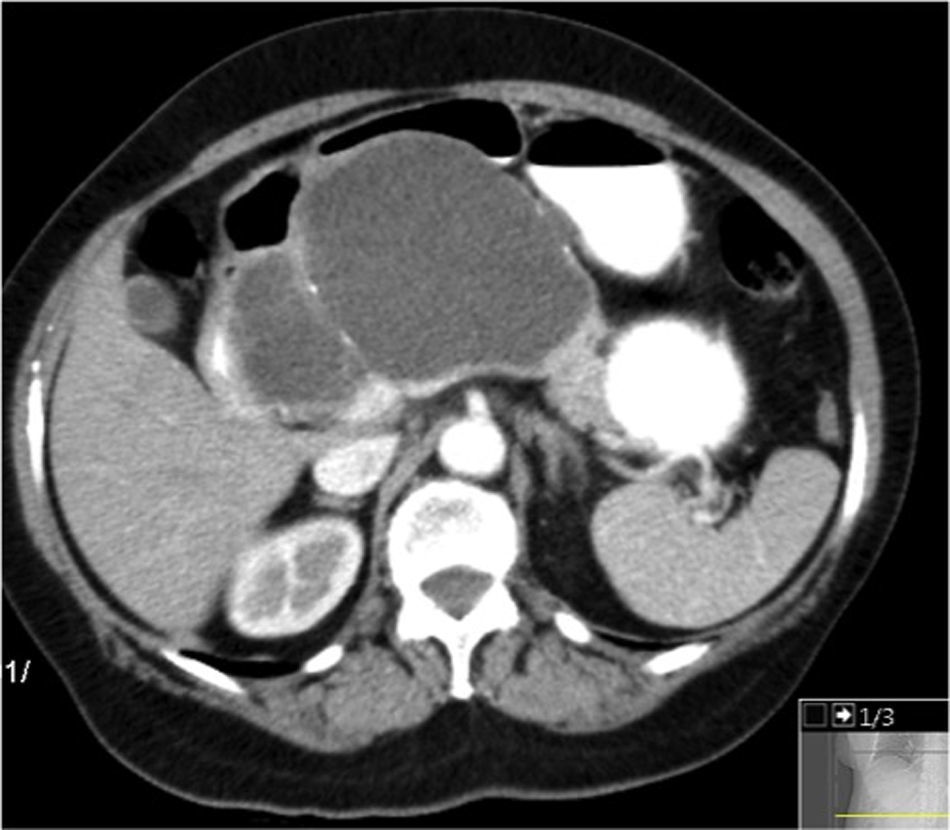
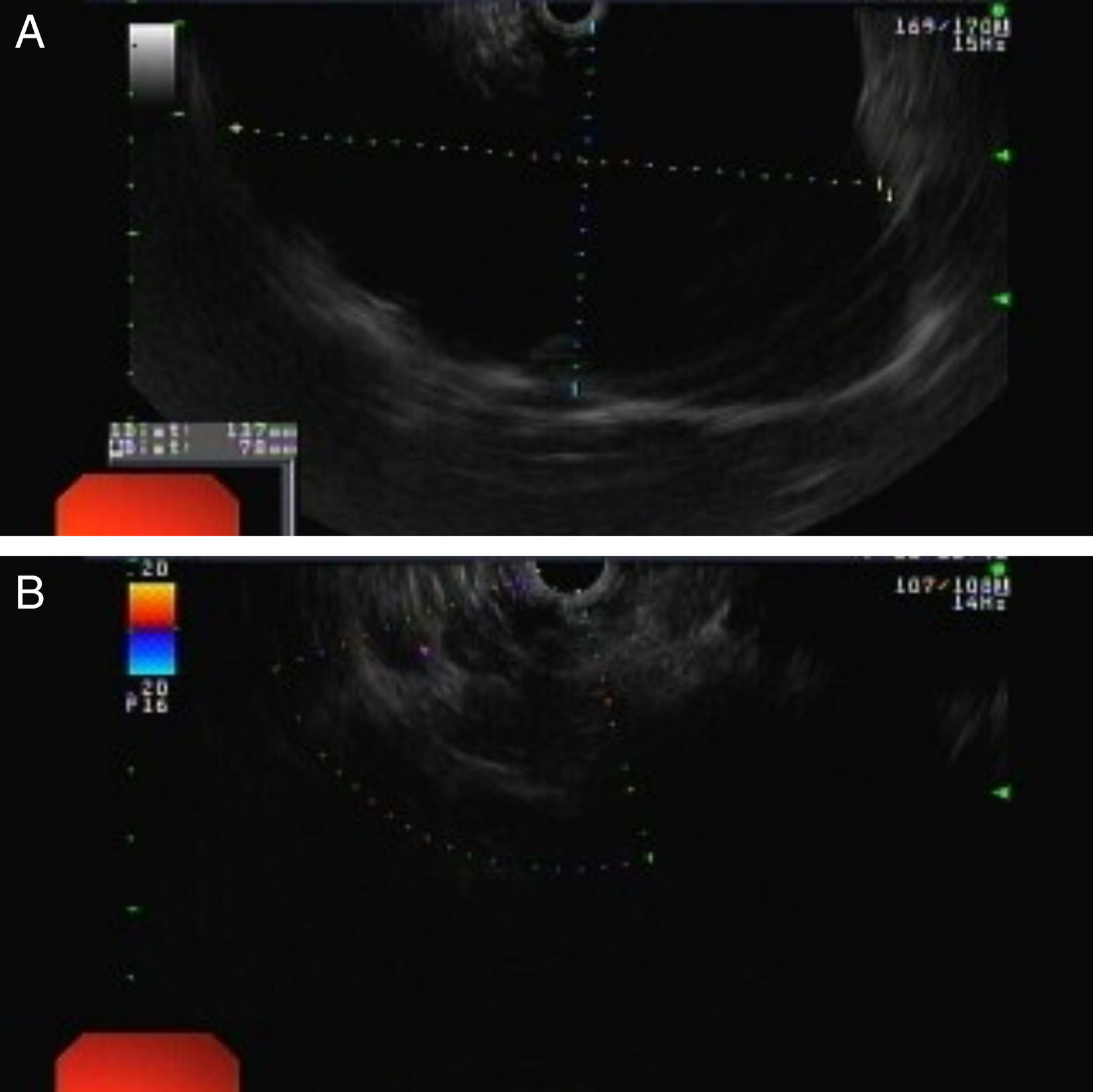
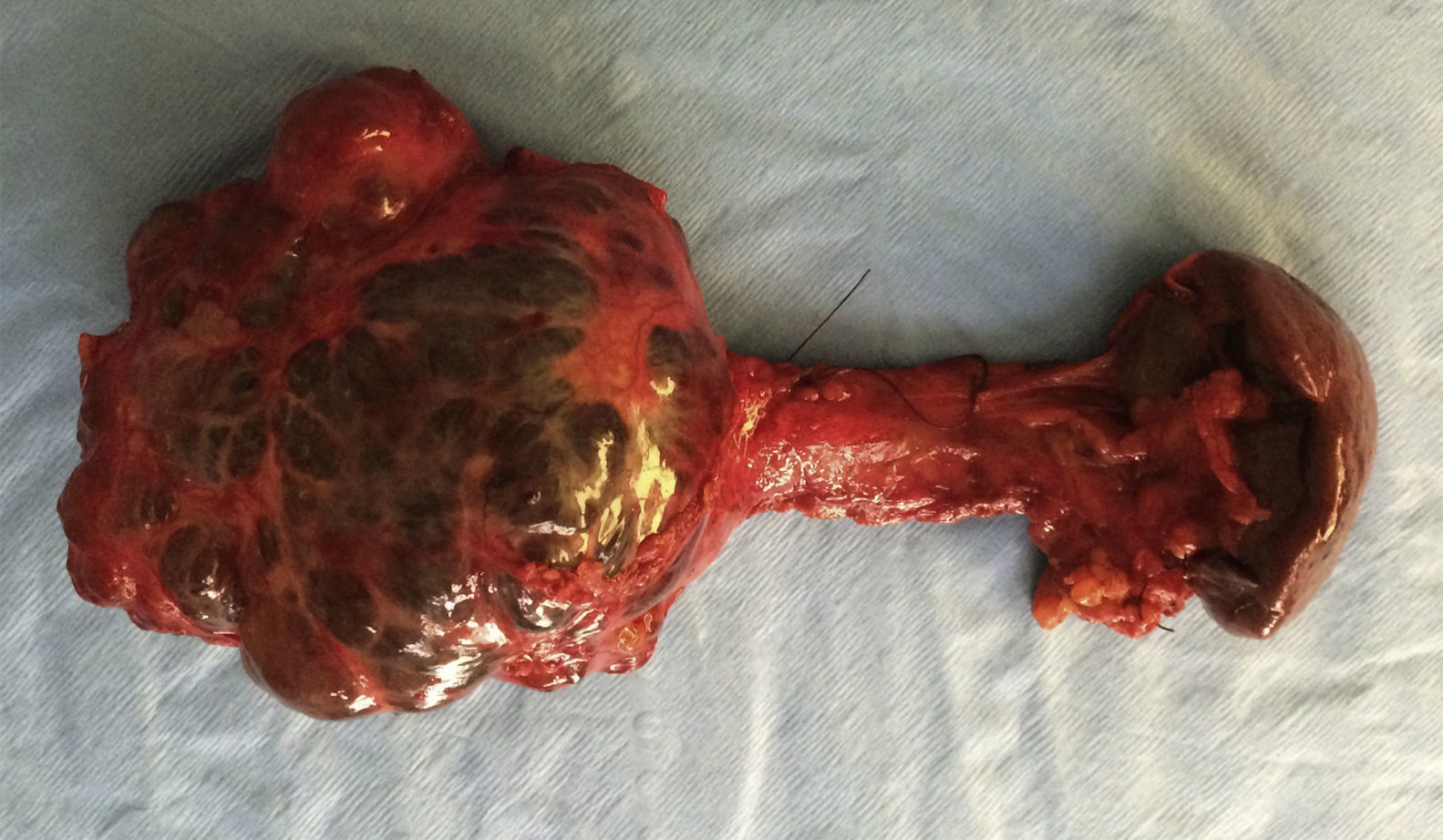
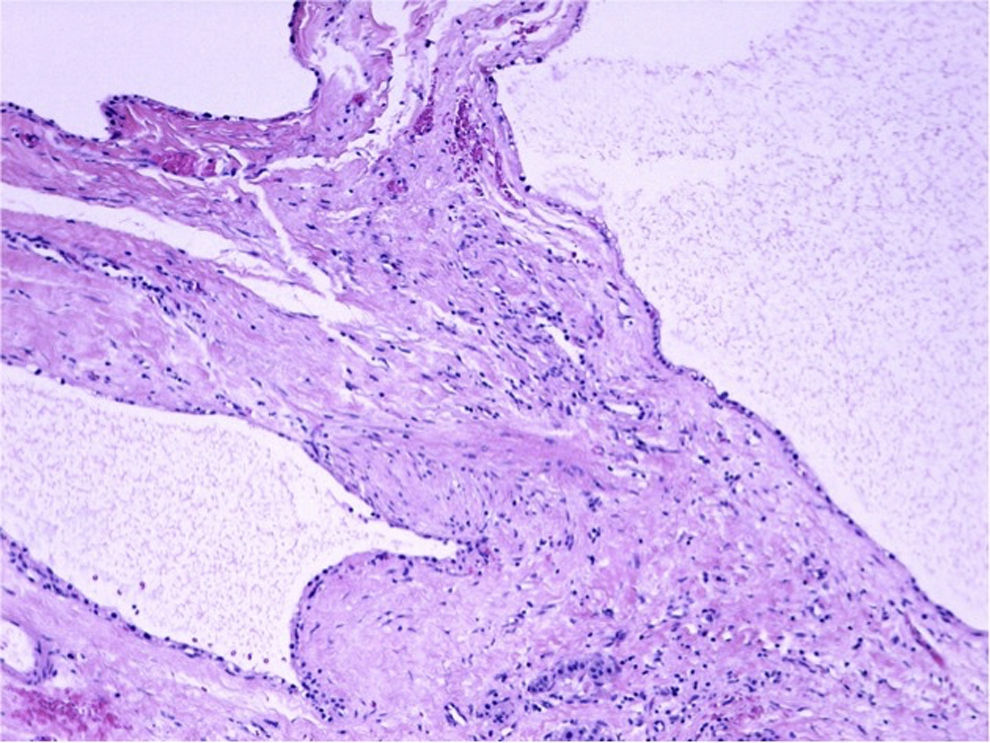
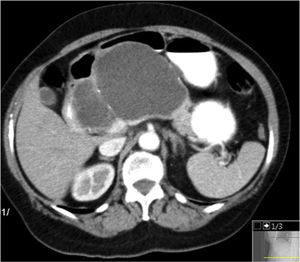
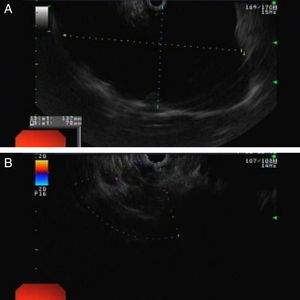
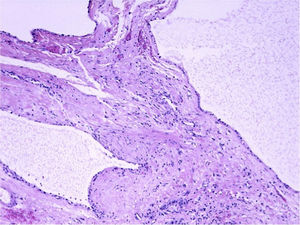
A 74-year-old woman was referred for further evaluation of a large pancreatic cystic lesion. She presented with abdominal discomfort, without weight loss, anorexia or history of pancreatitis or abdominal trauma. Physical examination revealed a large epigastric mass. A contrast-enhanced computed tomography (CT) showed a huge, well-defined, multiloculated cyst of 12cm in greatest dimension arising from the pancreatic body, with multiple wall calcifications, without typical imaging features of a particular pancreatic cystic neoplasm (Fig. 1). Endoscopic ultrasound (EUS) showed a multilocular cyst with a larger cyst (120mm×70mm) and a peripheral microcystic component (Fig. 2). EUS-guided fine-needle aspiration of 7mL of serous cystic fluid was performed from the largest cyst under prophylactic IV antibiotics. The sample had no malignant or mucus-producing cells and CEA (<2.5ng/mL) and amylase (41U/L) were within the reference values, making a serous cystadenoma the most likely diagnosis. Due to persistent epigastric discomfort, a distal pancreatectomy and splenectomy was performed (Fig. 3). Macroscopic examination of the resected specimen showed a combination of large cysts with several small cysts. On microscopy, the cysts were lined with a single layer of cuboidal epithelial cells with clear cytoplasm, PAS positive (Fig. 4). Histopathological examination confirmed the diagnosis of a pancreatic serous oligocystic adenoma.
Serous oligocystic adenoma (SOA) is a rare benign pancreatic tumor which represent an atypical macroscopic morphologic variant of serous cystadenomas (SCA).1 SOAs are characterized by a limited number of cysts with a diameter of >2cm and share imaging features overlapping those of mucinous cystic neoplasm (MCN) and branch-duct intraductal papillary mucinous neoplasm (BD-IPMN), thus frequently making the radiologic diagnosis difficult.2 Endoscopic ultrasound and cyst fluid aspiration have a role in distinguishing mucinous and serous lesions.3 Management is determined by the presence of symptoms. Giant serous cystadenomas are also rare; this term usually refers to a multicystic tumor larger than 10cm in diameter in comparison with a described mean tumor diameter of 5cm.4
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflicts of interestThe authors have no conflicts of interest to declare.