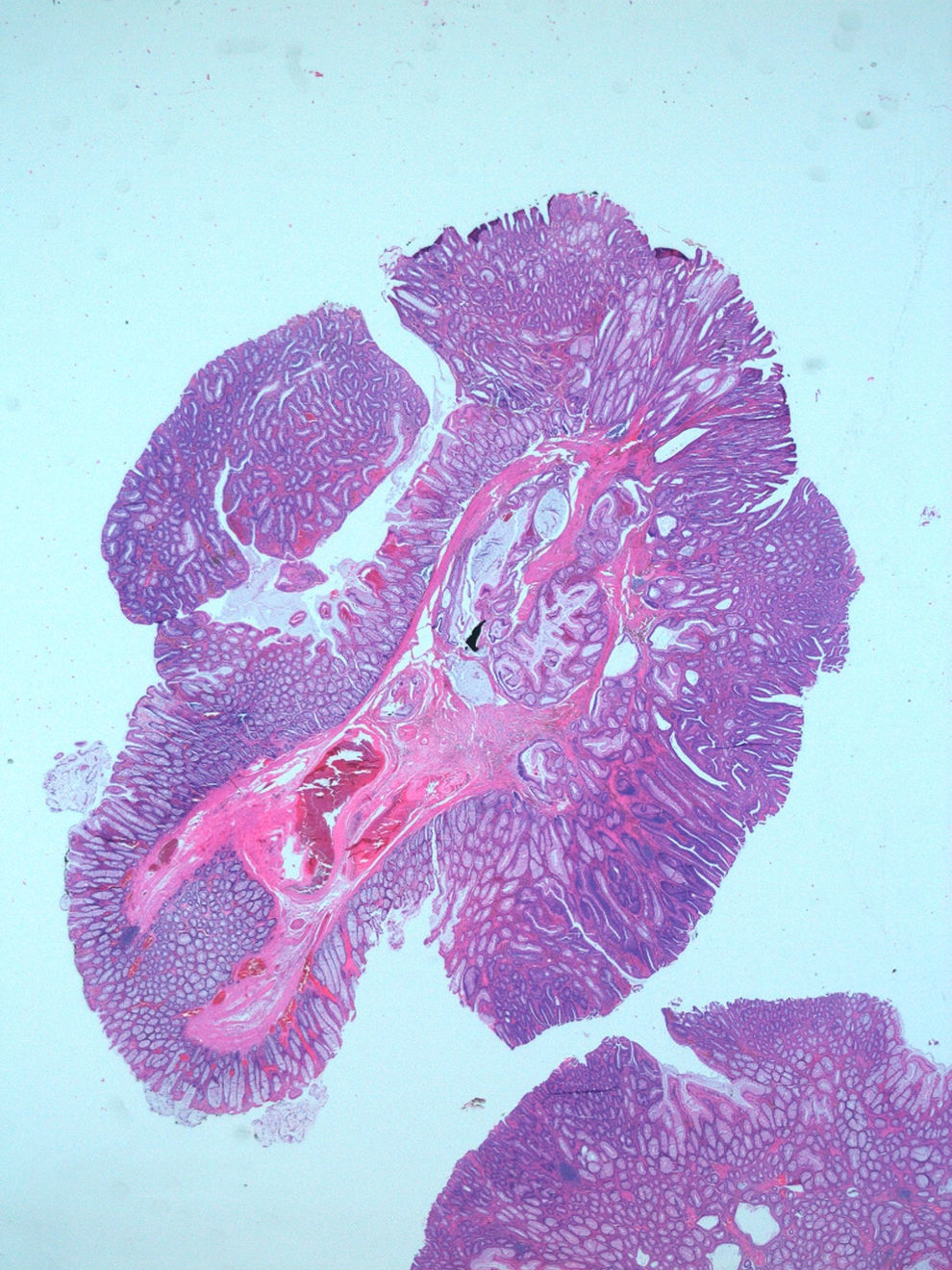
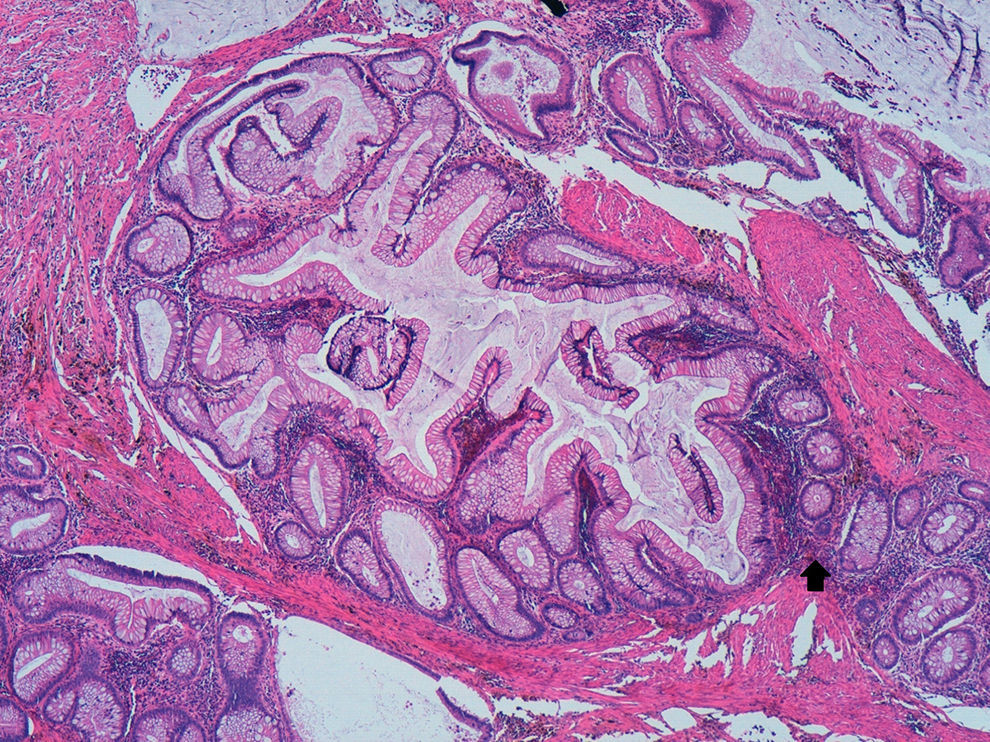
A 69 year-old man was referred to our department for polypectomy after a previous colonoscopy for colorectal cancer screening revealed three pedunculated polyps in the colon. The subsequent colonoscopy confirmed the presence of one polyp with 10mm in the transverse colon, and two in the sigmoid, about 15mm each; conventional snare polypectomy was performed, without complications. The microscopic evaluation of the transverse polyp revealed a tubule-villous adenoma with low-grade dysplasia. The evaluation of both sigmoid polyps was identical revealing aggregates of dilated and slightly irregular glands in the submucosa, in connection with the overlying mucosa (Fig. 1). These submucosal “misplaced” glands were located in stroma with chronic inflammatory infiltrate, hemosiderin deposit and fibrous reaction. Only mild cytological atypia was observed in some of the “misplaced” glands (Fig. 2). A diagnosis of adenomas with pseudoinvasion was made.
Inflammatory infiltrate, hemosiderin deposit and fibrosis in association with the “misplaced” glands. Only mild cytological atypia was observed in some of them. A “breakpoint” (arrow) in muscularis mucosae through which the “misplaced” part grew down was also identified (HE, 100×).
The term pseudoinvasion was first introduced in 1973.1 It represents the prolapse of benign adenomatous glands into its stalk, simulating carcinoma.1,2 Most pseudoinvasion in an adenomatous polyp is diagnosed pathologically after endoscopic polypectomy of colonic adenomas, especially pedunculated polyps in the sigmoid colon.1,3 It may occur secondary to tissue damage from repeated twisting of the stalk, ischemia or prior biopsy causing protrusion of glands through weak regions of the muscularis mucosae.1,4,5 Taking into account its pathogenesis, the term misplaced epithelium was proposed instead of pseudoinvasion.3
The recognition of pseudoinvasion in adenomatous polyps and its distinction from invasive cancer may be difficult and has considerable importance in follow-up.1,4 In fact, the behavior, significance and therapy of this entity are simply that of the adenoma in which it occurs.2
The diagnostic criteria of pseudoinvasion in adenomatous polyps include1,2: nests of adenomatous epithelium in the submucosa and/or stalk, usually circumscribed by lamina propria and muscularis mucosae, frequently with chronic inflammation and granulation tissue; absence of infiltrative pattern and desmoplastic stromal response; common demonstrable continuity with overlying adenoma through a gap in the muscularis mucosae; bland cytology and architecture with frequent cystic dilation of the glands; signs of recent hemorrhage or hemosiderin deposition; typical localization in the sigmoid colon. Additionally, no morphological aspects of neoplastic epithelium (as desmoplasia, frank atypia or pleomorphism) should be seen.1,3
Immunohistochemical studies can be an additional help in the distinction between pseudoinvasion and invasive carcinoma.2,3 Entrapped nests show strong, continuous staining of surrounding basement membrane with collagen type IV, while invasive carcinoma shows only weak, discontinuous staining. E-cadherin stains cell membranes of normal and adenomatous epithelium strongly, with markedly decreased intensity in carcinoma. p53 usually exhibits scattered nuclear staining in adenomas, and extensive in carcinomas.
Similar features of mucosal entrapment have also been reported in hyperplastic polyps.5 When pronounced, these may cause diagnostic confusion with other lesions such as adenomas with pseudoinvasion or even well-differentiated adenocarcinomas.
Benign lesions associated with mucosal prolapse, that may mimic invasive adenocarcinoma of colon, are relatively rare and may be unknown by some endoscopists. Since their recognition may prevent unnecessary aggressive treatments, it is important for clinicians to be aware of their existence and recognize their histopathologic characteristics.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that no patient data appear in this article.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflicts of interestThe authors have no conflicts of interest to declare.