To compare the effectiveness of two Cognitive-Behavioral Therapy (CBT) interventions—an individual and a group intervention—in Social Anxiety Disorder therapy. We compared the two treatment groups against a waitlist condition in a randomized clinical trial with 86 young adults. The individual CBT intervention was Trial-Based Cognitive Therapy (TBCT) developed by De-Oliveira, a novel technique in which the therapist engages the patient in a simulated judicial trial with the goal of identifying and changing core dysfunctional beliefs. The group intervention consisted of exposition therapy based on the Hofmann and Otto protocol (Group CBT) to restructure negative and dysfunctional cognitions regarding social situations. Both interventions reduced psychiatric symptoms from pre- to post-test and primary social anxiety and depression symptoms relative to waitlist controls. The interventions were recently introduced in Brazil, and this is the first randomized control trial to compare TBCT and this Group CBT, which were effective in assessing changes in social anxiety symptoms as well as co-occurring psychiatric symptoms.
Comparar la efectividad de dos intervenciones de Terapia Cognitivo-Conductual (TCC)-intervención individual y grupal- en tratamiento del Trastorno de ansiedad social. Comparamos los dos grupos de tratamiento con una condición de lista de espera en un ensayo clínico aleatorizado con 86 adultos jóvenes. La intervención individual de TCC fue la Terapia Cognitiva Basada en Ensayos (TCBE) desarrollada por De-Oliveira, una técnica novedosa en la cual el terapeuta involucra al paciente en un juicio judicial simulado con el objetivo de identificar y cambiar las creencias disfuncionales centrales. La intervención grupal consistió en terapia de exposición basada en el protocolo Hofmann y Otto (TCC grupal) para reestructurar cogniciones negativas y disfuncionales con respecto a situaciones sociales. Ambas intervenciones redujeron los síntomas psiquiátricos antes y después de la prueba y los síntomas de ansiedad y depresión social primarios en relación con los controles de la lista de espera. Las intervenciones se introdujeron recientemente en Brasil, y este es el primer ensayo de control aleatorizado para comparar TCBE y TCC grupal, que fueron efectivos para los cambios en los síntomas de ansiedad social y los síntomas psiquiátricos concurrentes.
Social Anxiety Disorder (SAD), also known as social phobia, is the most recurrent condition amongst anxiety disorders. In the United States, SAD is the fourth most common mental health condition, affecting more than 12.1% of the population (Kessler et al., 2005; Stein et al., 2017). Similarly high prevalence is observed also in Brazil, outranking every other mental condition (Andrade et al., 2012). Baptista et al. (2012) observed a prevalence of 11.6% in a wide sample of college students in the state of São Paulo. High prevalence notwithstanding, SAD is still an underdiagnosed and frequently untreated condition (Crippa, 2009). For instance, in a study by Baptista et al. (2012), only 1% of those diagnosed with SAD during the study had a previous SAD diagnosis. Research indicates that individuals with SAD usually hide, refraining from seeking either medical or psychological help for fear of a negative evaluation of their condition (Culpepper, 2006).
SAD can be characterized as a persistent, acute fear of either social or performance situations. Social situations are perceived as threatening due to the possibility of a negative assessment of the individual, and are thus either confronted with great discomfort or avoided altogether (American Psychiatric Association APA, 2013). Such social situations include making acquaintances, speaking and eating in public, and meeting persons of authority (American Psychiatric Association APA 2013; Ebrahimi, Pallesen, Kenter, & Nordgreen, 2019). SAD is chronic and significantly affects quality of life, harming one’s occupational functionality and social life (De-Oliveira et al., 2012; Dixon, Tull, Lee, Kimbrel, & Gratz, 2017; Gómez-Ortiz et al., 2019; Olivares-Olivares, Ortiz-González, & Olivares, 2019).
SAD frequently presents itself along with associated comorbidities, the most common of which being depression (Caetano et al., 2018; Garcia-Lopez, Bonilla, & Muela-Martinez, 2016; Klemanski, Curtiss, McLaughlin, & Nolen-Hoeksema, 2017; Langer et al., 2019; Nordahl, Nordahl, Vogel, & Wells, 2018). For instance, Katzelnick et al. (2001) observed some type of psychiatric comorbidity in roughly half of their sampled SAD patients, and Wong, Morrison, Heimberg, Goldin, and Gross (2014) observed depressive symptoms in almost 35% of SAD patients. Such comorbidities have been shown to worsen current conditions and prognosis, as well as to complicate treatment (Curtiss, Andrews, Davis, Smits, & Hofmann, 2017; Thompson, Boden, & Gotlib, 2017; Wersebe et al., 2018).
Several studies point out that Cognitive-Behavioral Therapy (CBT) has proved effective in treating SAD and should therefore be the first treatment option (Barkowski et al., 2016; Cuijpers et al., 2016; Mayo-Wilson et al., 2014; Scaini, Belotti, Ogliari, & Battaglia, 2016). In addition to reducing social anxiety symptoms, CBT has been shown to reduce depression symptoms, change neurobiological systems such as decreasing activity in the autonomic nervous systems, and improve cognitive information processing (e.g., Alden, Buhr, Robichaud, Trew, & Plasencia, 2018). CBT offers two main intervention techniques: group and individual (e.g., Olivares-Olivares, Olivares, Macià, Macià, & Montesinos, 2016). The former is the most common approach to SAD (Antón, Olivares, & Amorós-Boix, 2012) and presents consistent efficacy indicators in both the short and long term (Fogarty, Hevey, & McCarthy, 2019; Hofmann & Otto, 2008). Group intervention is effective due to the continuous exposure to a social situation inherent in being part of a group (Burlingame et al., 2016; Principe, Vincelli, & Capoderose, 2019).
The goal of group CBT is to restructure negative and dysfunctional cognitions regarding social situations. To accomplish this, therapy is delivered in cognitive restructuring sessions, self-guided exposition sessions, and in vivo exposure sessions. A realistic assessment of the experienced situations, along with changes in thoughts, emotions, and behaviors, produce a shift in the patient’s basic dysfunctional beliefs, thus leading to a lasting improvement. This treatment has been typically conducted in group settings (e.g., Hofmann, 2007).
CBT offers several individual approaches for social phobia as well. Trial-Based Cognitive Therapy (TBCT), or simply “the Trial,” is a novel individual intervention developed by the Brazilian psychiatrist Irismar Reis De-Oliveira at Universidade Federal da Bahia, in Brazil. The technique is based on the novel The Trial, by Franz Kafka, in which the main character, Josef K., is prosecuted, arrested and ultimately executed for a crime never revealed either to him or to the reader (De-Oliveira, 2011).
TBCT’s main technique is analogous to a court trial in which the therapist engages the patient in a simulated judicial trial with the goal of identifying and changing core dysfunctional beliefs. The trial is a structured technique, useful in eliciting patient’s dysfunctional negative core beliefs and developing positive, more realistic ones (De-Oliveira, 2007, 2011). The Trial incorporates other CBT techniques such as downward arrow, empirical evidence examination, Defense Attorney technique, and cognitive restructuring, but the therapist uses legal, rather than psychological, jargon.
Research has shown TBCT to effectively reduce a range of psychological symptoms compared to conventional CBT techniques (Caetano & De-Oliveira, 2018; De-Oliveira et al., 2012; Powell et al., 2013). De-Oliveira (2008) observed lower activation of dysfunctional negative core beliefs and associated emotions in 30 patients with different psychiatric disorders after a single therapeutic session employing the Trial. A second study with a similar methodological design by De-Oliveira et al. (2012) showed lower adherence to dysfunctional negative core beliefs and associated emotions in 166 patients with diverse psychiatric diagnoses after using the Trial. In addition, the therapy shows no difference in clinical results when the Trial was performed by therapists of different experience levels with the technique, as confirmed by a recent randomized clinical trial with 39 outpatients with various diagnoses (Delavechia, Velasquez, Duran, Matsumoto, & De-Oliveira, 2016).
TBCT’s focus on cognitive restructuring through the deployment of experiential techniques that mobilize significant emotional responses in patients make the approach a useful tool in SAD therapy, given the literature’s emphasis in cognitive restructuring to the alleviation of social anxiety present in SAD (Olivares-Olivares et al., 2019). Nonetheless, the novelty necessitates further research for a full comparison of this intervention to well-established techniques within CBT.
The literature suggests that both group interventions, such as those using Hofmann and Otto’s (2008) protocol, and individual interventions, such as those using TBCT, are effective in the treatment of SAD symptoms. However, it is yet to be shown which technique is more effective in reducing both SAD symptoms and comorbid symptoms (especially depression symptoms), which would be useful in therapy choice, mainly considering public health policies.
The goal of this study was to compare the effectiveness of two CBT interventions: an individual intervention using TBCT and a group intervention consisting of exposure therapy based on the Hofmann and Otto (2008) protocol (Group CBT). Both interventions were recently introduced in Brazil, and this is the first randomized control trial to compare TBCT and this Group CBT, and assess changes in social anxiety symptoms as well as co-occurring psychiatric symptoms.
MethodDesignThe current randomized clinical trial compares the benefits of two cognitive behavioral interventions and a waitlist control group for individuals with SAD using a pre- and post-test design. The two distinct interventions were the individual TBCT (a novel intervention within the cognitive behavioral therapy) and Group CBT (based on behavioral exposure).
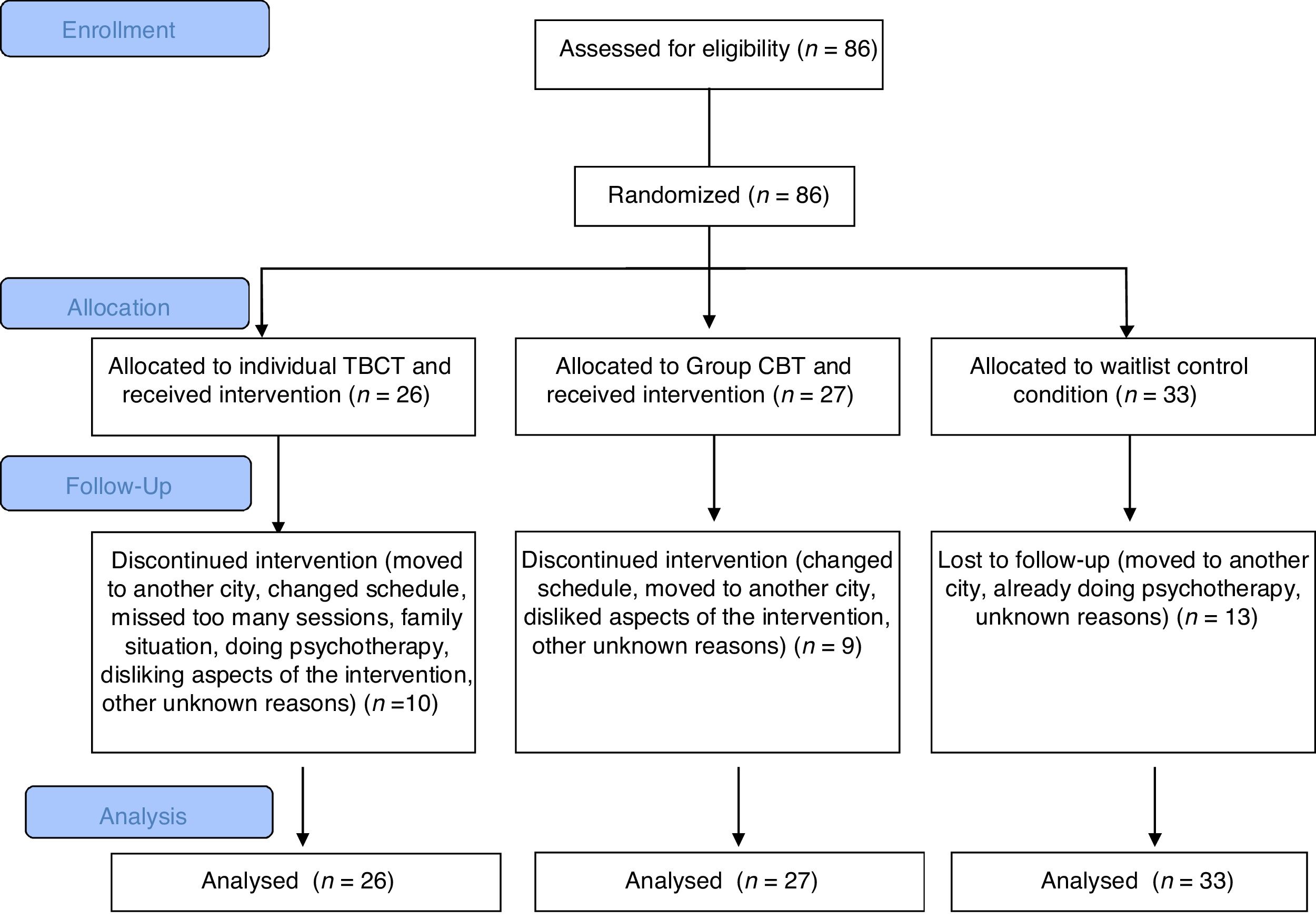
ParticipantsParticipants included 86 young adults (66 female, 46%) diagnosed with SAD, 26 of which were initially allocated to the TBCT intervention, 27 to the Group CBT intervention, and 33 to a waitlist controls (Figure 1). All subjects received the primary diagnosis of SAD based on SCID results, compliant to DSM-IV TR (American Psychiatric Association APA, 2000). Moreover, all subjects who received the interventions or were waitlisted received SPIN scores equal to or above 19, indicating the occurrence of symptoms compatible with the SAD diagnosis (Osório, Crippa, & Loureiro, 2009). Possible comorbidities where identified using Patient Health Questionnaire PHQ-9 and Self-Reporting Questionnaire, 20-item SQR-20. Exclusion criteria were the presence of psychotic symptoms, severe cognitive impairment, and primary diagnostic of a disorder other than SAD.
The attrition rate was 35% (30 subjects), due to changes in their schedule (6%), moving to a different city (5%), missing too many sessions (2%), disliking aspects of the intervention (2%) regarding (a) random assignment to TBCT and (b) not feeling confortable in Group CBT, already doing psychotherapy (1%), family situation (1%), or unknown reasons (13%).
InstrumentsTherapeutic Interventions. TBCT was provided in weekly, 90 minutes-long sessions by one of the researchers, a trained clinical psychologist, using a protocol created by the developer of TBCT, Dr. Irismar Reis De-Oliveira. Group CBT was provided in weekly, 120 minute-long sessions by trained clinical psychologist with the support of another therapist. Each group consisted of six participants and the protocol developed by Hofmann and Otto (2008).
Structured Clinical Interview for DSM-4-Clinician (SCID-CV) and Research (SCID-RV) Versions. The Brazilian version (Del-Ben et al., 2001) of the Research (RV) and Clinical (CV) versions of SCID were used for assessing and diagnosing Axis I Disorders pursuant to DSM-IV-TR (American Psychiatric Association APA, 2000). SCID-RV’s Module F (Anxiety Disorders) was used to confirm SAD symptoms and assess the diagnostic criteria for SAD as set by DSM-IV-TR. SCID-CV’s Modules A (Mood Episodes), B (Psychotic and Associated Symptoms), E (Substance Use Disorders) and F (Anxiety Disorders) were used to diagnose SAD and to assess the presence of other disorders to control for comorbidities.
Social Phobia Inventory (SPIN). The Brazilian version (Osório, Crippa et al., 2009; Cronbach’s alpha=.90) of SPIN (Connor et al., 2000) was used for assessing fear, avoidance, and physiological symptoms associated with SAD. The 17 items were rated on a 5-point scale indicating severity of each symptom over the past week from not at all (0) to extremely (5).
Beck Anxiety Inventory (BAI). The Brazilian version (Cunha, 2001; Cronbach’s alpha=.76) of BAI (Beck, Epstein, Brown, & Steer, 1988) was used for measuring typical anxiety symptoms in the previous week. The 21 items were measured on a 4-point Likert scale ranging from less (0) to more (3) severe symptoms.
Fear of Negative Evaluation Scale (FNE). The Brazilian version (Silva & Nardi, 2009) of the FNE (Watson & Friend, 1969) was used to assess fear of negative evaluation of social situations, a core characteristic of SAD. Participants were asked to indicate if each of the 30 situations presented were true (1) or false (0) for them, and responses were summed.
Social Avoidance and Distress Scale (SADS). The Brazilian version (Levitan, Nascimento, Freire, Mezzasalma, & Nardi, 2008) of SADS (Watson & Friend, 1969) was used to measure symptoms of avoidance of social events and social discomfort. Participants were asked to indicate if each of the 28 situations presented were true (1) or false (0).
Patient Health Questionnaire (PHQ-9). The Brazilian version (Osório, Mendes, Crippa, & Loureiro 2009; Cronbach’s alpha=.85) of the PHQ-9 (Kroenke, Spitzer, & Williams, 2001) based on DSM-IV Major Depression diagnosis was used for screening major depressive episodes in the previous two weeks. The 9 items were measured on a 4-point Likert scale ranging from not at all (0) to nearly every day (3).
Beck Depression Inventory (BDI-II). The Brazilian version (Cunha, 2001; Cronbach’s alpha=.81) of BDI (Beck, Ward, Mendelson, Mock, & Erbaugh, 1961) was used to measure the severity of symptoms of depression. The 21 items were measured on a 4-point Likert scale ranging from less (0) to more (3) severe symptoms.
Self-Reporting Questionnaire, 20-item (SRQ-20). The Brazilian version (Mari & Williams, 1986; Cronbach’s alpha=.80) of SRQ-20 (Harding et al., 1980) was used to detect common mental health problems (i.e., physical and emotional symptoms). Participants were asked to indicate yes (1) or no (0) for each of the 20 question.
ProcedureAll procedures were authorized by the Institutional Review Board of University of São Paulo’s School of Philosophy, Sciences and Literature at Ribeirão Preto. Volunteers were contacted and informed about the study’s procedures. Subjects were recruited through clinical services, the internet, television, and local media. This sample included subjects who demonstrated the ability to read, write, understand, and sign the informed consent form.
The initial assessment comprised a diagnostic interview as well as the battery of self-report instruments previously detailed. If SCID-RV’s F Module confirmed SAD, the aforementioned SCID-CV Modules were utilized to identify Axis I comorbidities. An external advisor then randomly assigned volunteers with diagnosis of SAD into one of the three conditions (i.e., TBCT, Group CBT, or waitlist). Those waitlisted were offered the therapy after the study was over. Volunteers whose diagnosis did not confirm SAD were excluded from the study and referred to appropriate care according to the presenting problem. Both TBCT and Group CBT were provided over 16 therapy sessions. After 16 weeks, participants from all three conditions answered the same questionnaires from baseline.
Data analysisGroup characteristics were compared at pre-test using Univariate Analyses of Variance (ANOVAs) to compare continuous variables and Chi-Square to compare categorical variables. A mixed ANOVA was performed for time of testing (pre- vs. post-test) to evaluate the benefits of the interventions (between group effects). An alpha of .05 was used for all analyses, and p-values were submitted to Bonferroni correction using IBM SPSS Statistics (version 21). Intent-to-treat analysis were used to account for possible effects of drop out participation (McCoy, 2017).
To examine between-group differences across the conditions, a latent change score approach to test temporal change and time-sequential associations was adopted using the R package Lavaan (Grimm, Zhang, Hamagami, & Mazzocco, 2013; Rosseel, 2012). Comparisons between conditions were evaluated for both symptoms of social anxiety and depression, using the SPIN and BDI-II. Consistent with the procedures by Coman et al. (2013), a latent change model was specified such that the mean of the latent variable represents the difference between the pre-treatment (T1) and post-treatment means (T2). The T2 variable was regressed on both the latent change variable and the T1 variable, and both pathways were fixed to 1. Initially, the pathway from T1 to the latent change score was fixed to 0, which indicates stability in changes. If this assumption was not upheld, as indicated by poor model fit, then a covariance parameter between T1 and the latent change score was permitted. The variance of the latent change score was fixed to 1, and the intercept of the T2 was fixed to 0. Between-group differences were examined by specifying a conditional latent change score model, in which dummy coded treatment variables predicted the latent change score. Full-information maximum likelihood was used as the estimator.
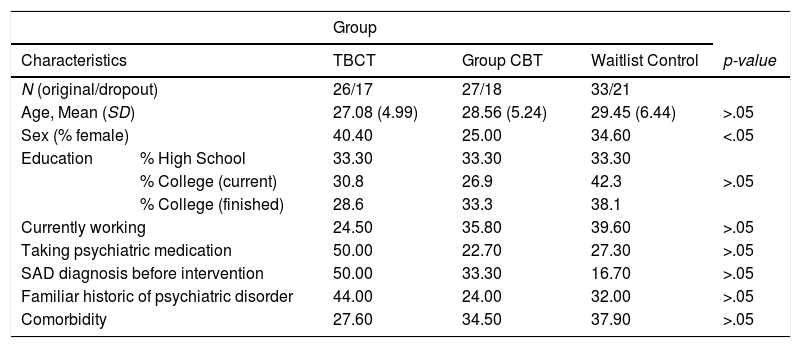
ResultsAll participant characteristics are presented in Table 1. Overall, all three groups were equivalent at baseline. The only group difference was the percent female assigned to TBCT, which was bigger than that assigned to Group CBT. When added sex as a covariate in further analyses, sex was not a significant predictor of performance and all interactions remained significant. Thus, results are presented without further consideration of possible effects of sex.
Comparison of participants’ characteristics by group.
| Group | |||||
|---|---|---|---|---|---|
| Characteristics | TBCT | Group CBT | Waitlist Control | p-value | |
| N (original/dropout) | 26/17 | 27/18 | 33/21 | ||
| Age, Mean (SD) | 27.08 (4.99) | 28.56 (5.24) | 29.45 (6.44) | >.05 | |
| Sex (% female) | 40.40 | 25.00 | 34.60 | <.05 | |
| Education | % High School | 33.30 | 33.30 | 33.30 | >.05 |
| % College (current) | 30.8 | 26.9 | 42.3 | ||
| % College (finished) | 28.6 | 33.3 | 38.1 | ||
| Currently working | 24.50 | 35.80 | 39.60 | >.05 | |
| Taking psychiatric medication | 50.00 | 22.70 | 27.30 | >.05 | |
| SAD diagnosis before intervention | 50.00 | 33.30 | 16.70 | >.05 | |
| Familiar historic of psychiatric disorder | 44.00 | 24.00 | 32.00 | >.05 | |
| Comorbidity | 27.60 | 34.50 | 37.90 | >.05 | |
Note. All analyses were performed for the full sample. TBCT: Trial-Based Cognitive Therapy; Group CBT: Group Cognitive-Behavioral Therapy; WL: Waitlist control; SD: Standard Deviation; SAD: Social Anxiety Disorder.
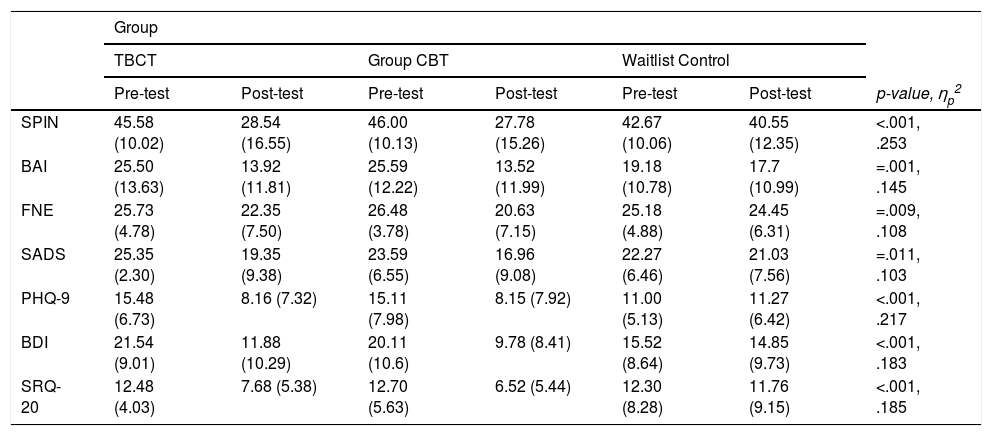
Overall, results indicated that participants improved during posttest in both TBCT and Group CBT when compared to pretest in all measures (Table 2). Effect sizes were more robust for changes in responses to SPIN and PHQ-9 and most changes in symptoms showed a reduction of scores by half in all scales, except FNE and SADS (which in turn had the smaller effect sizes, although changes were sill significant). The waitlist condition was not associated with significant differences. Results remained the same when only participants who completed the interventions were analyzed.
Means (and standard deviations) of clinical scores during pre- and post-test by intervention.
| Group | |||||||
|---|---|---|---|---|---|---|---|
| TBCT | Group CBT | Waitlist Control | |||||
| Pre-test | Post-test | Pre-test | Post-test | Pre-test | Post-test | p-value, ηp2 | |
| SPIN | 45.58 (10.02) | 28.54 (16.55) | 46.00 (10.13) | 27.78 (15.26) | 42.67 (10.06) | 40.55 (12.35) | <.001, .253 |
| BAI | 25.50 (13.63) | 13.92 (11.81) | 25.59 (12.22) | 13.52 (11.99) | 19.18 (10.78) | 17.7 (10.99) | =.001, .145 |
| FNE | 25.73 (4.78) | 22.35 (7.50) | 26.48 (3.78) | 20.63 (7.15) | 25.18 (4.88) | 24.45 (6.31) | =.009, .108 |
| SADS | 25.35 (2.30) | 19.35 (9.38) | 23.59 (6.55) | 16.96 (9.08) | 22.27 (6.46) | 21.03 (7.56) | =.011, .103 |
| PHQ-9 | 15.48 (6.73) | 8.16 (7.32) | 15.11 (7.98) | 8.15 (7.92) | 11.00 (5.13) | 11.27 (6.42) | <.001, .217 |
| BDI | 21.54 (9.01) | 11.88 (10.29) | 20.11 (10.6) | 9.78 (8.41) | 15.52 (8.64) | 14.85 (9.73) | <.001, .183 |
| SRQ-20 | 12.48 (4.03) | 7.68 (5.38) | 12.70 (5.63) | 6.52 (5.44) | 12.30 (8.28) | 11.76 (9.15) | <.001, .185 |
Note. TBCT: Trial-Based Cognitive Therapy; Group CBT: Group Cognitive-Behavioral Therapy; WL: Waitlist control; ηp2=Partial Eta Squared; SPIN: Social Phobia Inventory; BAI: Beck Anxiety Inventory; FNE: Fear of Negative Evaluation Scale; SADS: Social Avoidance And Distress Scale; PHQ-9: Patient Health Questionnaire; BDI: Beck Depression Inventory; SRQ-20: 20-items Self-Reporting Questionnaire.
Results of the latent change score analyses are presented in Table 3. The original conditional latent change score model for social anxiety symptoms, in which the regression parameter from pre-treatment symptoms to the latent change score was fixed to 0, exhibited worse model fit than the model permitting a covariance parameter between these variables (χ2Δ=7.58, df=1, p<.01). Freely estimating this covariance parameter relaxes the assumption that change across time must be stable. The new model evidenced adequate model good fit with a non-significant chi-square statistic (χ2 = 3.18, p = .20), as well as good fit indices (i.e., CFI=.97; TLI=.94; and RMSEA=.10). The regression coefficients representing the contrasts between the active treatments and waitlist both significantly predicted the latent change score (TBCT vs. WL, γ = −21.19, p < .01; Group CBT vs. WL, γ = −22.34, p < .01). This suggests that, on average, individuals in the TBCT and Group CBT conditions experienced significantly greater reductions in social anxiety symptoms relative to waitlist control. The comparison between TBCT and Group CBT did not reveal a significant difference (γ=1.15 p > .05).
Conditional latent change score model.
| Social Anxiety Symptoms | Depression Symptoms | |
|---|---|---|
| αPre-Sx | 45.14**(1.24) | 18.77**(1.46) |
| φPreSx*LCS | −31.23*(14.28) | −63.69**(18.49) |
| φPreSx*PreSx | 87.81**(13.12) | 96.34**(17.04) |
| φLCS*LCS | 106.48**(24.08) | 95.70**(21.79) |
| λTBCTvsCBT | 1.15 (3.64) | 0.76 (2.35) |
| λCBTvsWL | −22.34**(3.09) | −11.14**(2.27) |
| λTBCTvsWL | −21.19**(3.19) | −10.38**(2.44) |
Note. LCS: Latent change score; TBCT:Trial-Based Cognitive Therapy; CBT: Group Cognitive-Behavioral Therapy; WL: Waitlist control; αPre-Sx: intercept of pre-treatment social anxiety (or depression); φPreSx*LCS: covariance between pre-treatment depression and latent change score; φPreSx*PreSx: variance of pre-treatment social anxiety (or depression); φLCS*LCS: variance of latent change score; λExp: unstandardized path coefficient from experimental condition to the latent change score. * p < .05; **p < .01.
Likewise, the original conditional latent change score model for depression symptoms, in which the regression parameter from pre-treatment symptoms to the latent change score was fixed to 0, exhibited worse model fit than the model permitting a covariance parameter between these variables (χ2Δ=31.09, df =1, p < .01). Freely estimating this covariance parameter relaxes the assumption that change across time must be stable. The new model evidenced adequate model good fit with a non-significant chi-square statistic (χ2 = 3.19, p = .20), as well as good fit indices (i.e., CFI=.95; TLI=.87; and RMSEA=.10). The hypothesis for differential efficacy for depression outcome was supported for the comparison between the active treatments and waitlist (TBCT vs. WL, γ = −10.37, p < .01; Group CBT vs. WL, γ = −11.14, p < .01). This suggests that, on average, individuals in the TBCT and Group CBT conditions experienced significantly greater reductions in depression symptoms relative to waitlist control. The comparison between TBCT and Group CBT did not reveal a significant difference on depression (γ=.76, p > .05).
To determine whether baseline levels of BDI-II, FNE, or SADS moderated treatment outcome for the SPIN across all pairwise comparisons across the three groups, a number of models including interaction terms were pursued. After applying false-discovery rate corrections, results revealed that none of those measures moderated treatment outcome for social anxiety symptoms (p’s < .05).
DiscussionThis study aimed to evaluate the effect of two CBT interventions for social anxiety: individual TBCT, a new therapy within the field, and Group CBT, a group therapy based on exposure through high social costs and cognitive restructuring. This was the first randomized clinical trial that evaluated and compared TCBT (De-Oliveira, 2011) and the Group CBT treatment proposed by Hofmann and Otto (2008) in Brazil, while specifically investigating changes in symptoms of social anxiety, general anxiety, fear of negative evaluation, avoidance and social discomfort, depression, and symptoms of comorbid psychiatric disorders.
Overall, results appear to be in the same direction as those found in the literature regarding the high efficacy of CBT in the treatment of SAD, which is considered the gold standard (Barkowski et al., 2016; Cuijpers et al., 2016; Mayo-Wilson et al., 2014). In particular, individuals in both interventions showed greater reductions in both social anxiety and depression symptoms relative to waitlist controls as seen by latent change scores results. (Nevertheless, note that sample size was limited and results should be interpreted in light of the design; see Hackshaw, 2008, for more information.) Moreover, post-test comparisons to pre-test results showed that both interventions were able to reduce social anxiety symptoms evaluated by SPIN, the primary efficacy measure in of SAD in this study. There was a significant reduction in severity of general anxiety symptoms (as measured by the BAI) in both treatment groups, as well as a reduction in SAD symptoms of fear and avoidance of social situations as well as social discomfort (as measured by FNE and SADS). Concomitantly, the two interventions also led to a reduction in symptoms of depression in terms of frequency of major depressive episodes and severity of symptoms (as measured by PHQ-9 and BDI). Finally, both interventions showed a reduction of the probability of presence of mental health problems.
The results suggest that both treatments were equally effective in reducing different comorbidity symptoms in patients with SAD, even though the Group CBT involves a higher social cost than individual therapy sessions (Barkowski et al., 2016). This result is in line with existing literature that points out that any CBT intervention generates a reduction not only in social anxiety symptoms, but also in associated psychiatric symptoms (Cuijpers et al., 2016). Interventions that are effective in reducing not only social anxiety symptoms but also different associated comorbid symptoms, especially depressive ones, may be very useful in clinical practice given the high presence of comorbidities in the SAD condition (Wong et al., 2014). Overall, both treatments are viable options for those suffering from SAD. Because less therapist time is needed for a group intervention, Group CBT is more cost-effective than individual TCBT. On the other hand, it is easier to schedule patients for individual sessions than scheduling group sessions.
FundingThis work was support by grants from the São Paulo Research Foundation (FAPESP), São Paulo, SP, Brazil [grant numbers 2013/19981-1, 2013/19273-7, 2013/19263-1, 2013/19263-1].