The main aim of this study was to analyze differences in inhibition and cognitive flexibility, taking into account some variables that may influence results (non verbal reasoning, depression, anxiety, intolerance of uncertainty, comorbidity, medication consumption).
MethodThe participants were 95 adults aged 17-61 years old (M=33.48, SD=11.13), primary (most severe) Generalized Anxiety Disorder or Obsessive-Compulsive Disorder and a healthy control group. Neuropsychological neasures were completed using computerized Wisconsin Card Sorting Test, Stroop Color Word Test and Go/NoGo Task.
ResultsClinical groups presented worse results in cognitive flexibility to the control group. The obsessive-compulsive group showed worse scores in flexibility than the generalized anxiety group, once non-verbal reasoning and tolerance to uncertainty were controlled. Comorbidity and medication use did not affect results in the obsessive compulsive group but did however influence the generalized anxiety group.
ConclusionsCognitive flexibility could be included treatment in the treatment of obsessive-compulsive disorder and generalized anxiety disorder.
El objetivo de este estudio fue analizar las diferencias en flexibilidad cognitiva e inhibición de respuestas teniendo en cuenta algunas variables que pueden influir en los resultados (razonamiento no verbal, depresión, ansiedad, intolerancia a la incertidumbre, comorbilidad, consumo de fármacos).
MétodoLos participantes fueron 95 adultos de edades comprendidas entre 17-61 años (M=33,48; DT=11,13), diagnosticados de Trastorno obsesivo-compulsivo, Trastorno de ansiedad generalizada y un grupo de control sano. Las variables neuropsicológicas fueron evaluadas con el Test de Clasificación de Tarjetas de Wisconsin, Test Stroop de Colores y Palabras y Tareas Go/NoGo.
ResultadosLos grupos clínicos presentaron peores resultados en flexibilidad cognitiva frente al grupo control. El grupo obsesivo-compulsivo alcanzó peores puntuaciones en flexibilidad que el grupo con ansiedad generalizada, una vez controlado el razonamiento no verbal y la tolerancia a la incertidumbre. La comorbilidad y el consumo de fármacos no afectaron a los resultados en el grupo obsesivo-compulsivo. Sin embargo, ambas variables influyeron en el grupo con ansiedad generalizada.
ConclusionesLa flexibilidad cognitiva podría ser incluida en los paquetes de tratamiento del Trastorno obsesivo-compulsivo y del Trastorno de ansiedad generalizada.
Obsessive-compulsive disorder (OCD) and generalized anxiety disorder (GAD) are categorized in different chapters of the Diagnostic and Statistical Manual of Mental Disorders (DSM-5, American Psychiatric Association APA, 2013). However, high comorbidity rates and phenomenological overlap may indicate common underlying processes (Peris et al., 2017, Taboas, Ojserkis, & McKay, 2015). Although the diagnostic criteria of both disorders are clear, clinical manifestations in real practice often complicate diagnosis as they can be comorbid, share risk factors and respond to similar pharmacological and psychological treatments. This has led some researchers to analyze cognitive processes and underlying common mechanisms.
Executive function (EF) and the relationship between its different subdomains either as independent entities, or as part of a whole, has been the subject of debate. EF could be described as a set of high level control mechanisms whose main purpose is regulation of cognition, behavior and emotions to meet individual goals and objectives (Miyake & Friedman, 2012). Some authors consider working memory, cognitive flexibility (CF) and inhibitory control as the main mechanisms responsible for executive control (Diamond, 2013). Inhibition refers to mental processes responsible for intentional and voluntary control or the ability to prevent interference of non-pertinent information in the face of responses or patterns of responses underway and to suppress previously relevant information which is not currently useful (Carlson & Wang, 2007). The most frequently used test for assessing this EF is the Wisconsin Card Sorting Test (WCST). Perseverative errors are the main signs of frontal dysfunction, although number of categories obtained has often been used as an equivalent indicator (Teubner-Rhodes, Vaden, Dubno, & Eckert, 2017). Response inhibition (RI) is not considered a unitary function, since it includes RI at the motor (or behavioral) level and the control of interference or cognitive inhibition. Some tests are the Stroop Test and the Go/NoGo tasks. Cognitive inflexibility appears an important feature of OCD (Kim et al., 2019).
Study results on the role of CF and RI in neurocognitive tasks have shown discrepancies. Some research has found that OCD patients have performance problems in CF tasks (Dittrich & Johansen, 2013), while others report that they work similarly to healthy controls (Moritz et al., 2002). Research on inhibitory executive function in OCD patients has obtained inconsistent results, as occurred with CF. Some studies have reported a worse performance for errors of commission in OCD in a Go/NoGo (motor inhibition) task, though there were no differences in errors of omission and reaction time (Abramovitch, Giving, Schweiger, & Hermesh, 2011). Other studies have found differences in both errors of commission and reaction time (Abramovitch, Giving, Hermesh, & Schweiger, 2012) while Kurt, Yildirim, & Topçuoğlu (2017) found no differentiation.
Abramovitz, Abramowitz, and Mittelman (2013) reported that results found in RI showed a lesser overall effect size than expected, perhaps due to the different sensitivity of tests used in these studies (Go/Nogo errors of commission and Stroop interference). The same occurred with the CF results, with different tests used in studies, indicating the importance of the influence of tools on results and highlighting important limitations in primary studies.
Other meta-analyzes (Shin, Lee, Kim, & Kwon, 2014; Snyder, Kaiser, Warren, & Heller, 2015) pointed out that effect sizes were medium and medium-low in RI while medium in CF. They also reported that depression could influence results if measured as a continuous variable. Other influential variables were age and medication consumption. Abramovitch, McCormack, Brunner, Johnson, and Wofford (2018) found that the worst performance of OCD patients in neuropsychological tests was linked to symptomatic severity approaching a mean effect size in CF tasks.
CF has also been studied in anxiety and related disorders and difficulties have been found (Park & Moghaddam, 2017). As for GAD, RI deficits have been found compared to healthy controls, obtaining a significantly worse performance in the Stroop but not in Go/NoGo. Performance is related to the severity of symptoms for an inhibition task -Stroop- but not- Go/NoGo (Hallion, Tolin, Assaf, Goethe, & Diefenbach, 2017). By contrast, Leonard, and Abramovitch (2018) found no statistically significant differences between GAD patients and a control group. However, Kim et al. (2019) found OCD and GAD groups had worse performance in CF compared to the control group, being more impaired in GAD patients. These differences were eliminated when severity and medication was controlled
On the other hand, cognitive models assign a central role to dysfunctional beliefs and intrusive thoughts in maintaining mental disorders (Pascual-Vera et al., 2019; Rosa-Alcázar et al., 2019). Dugas, Gagnon, Ladouceur, and Freeston (1998) reported that intolerance of uncertainty could be a variable of cognitive vulnerability in the excessive and uncontrollable worries of GAD. Intolerance of uncertainty has been related to GAD and OCD, finding links between OCD severity and uncertainty (LaPosa, Collimore, Hawley, & Rector, 2015).
The different meta-analyzes highlight certain limitations. In particular, they reported that some studies had used self-report measures rather than clinical interviews; most comparison groups versus OCD patients were non-clinical (healthy) groups; anxiety and depression had not been controlled with validated quantitative measures; some variables could influence results -duration of disorder, comorbidity, use of medication, age and sex. The age of the participants and the duration of the disorder were moderating variables of the results in some studies, although in others no significant relationship was found (Abramowitz, Abramovitz, & Mittelman, 2013; Kim et al., 2019; Shin et al., 2014, Snyder et al., 2015).
Aims were as follows: (1) to analyze RI and CF differences among patients with OCD, GAD and a healthy control group; (2) to study if CF and RI performance can be influenced by nonverbal reasoning and intolerance of uncertainty; (3) to verify if duration of disorder and anxiety and depression levels influence results; (4) to analyze if there are differences in executive function within each clinical group due to comorbidity and medication use; and (5) to assess relationship between CF and IR and obsessive and worry responses.
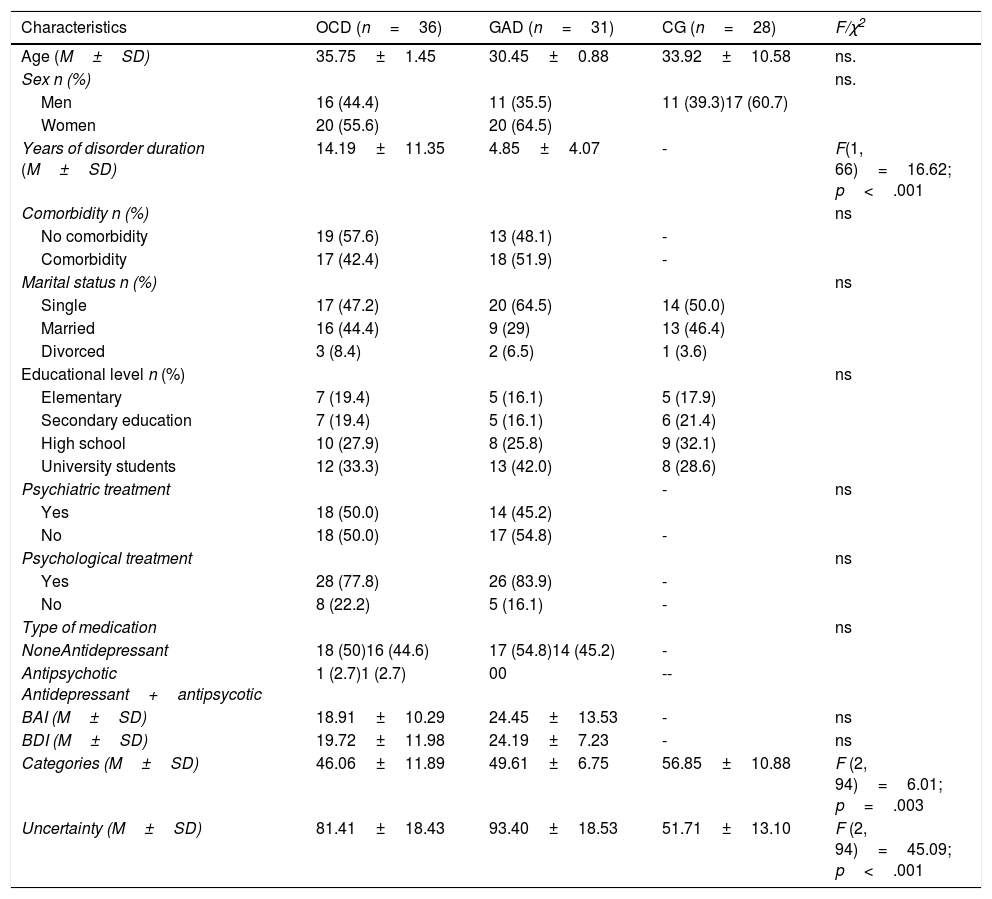
MethodParticipantsParticipants were 95 adults aged between 17-61 years (M=33.48, SD=11.13), diagnosed with OCD and GAD (American Psychiatric Association APA, 2013) and a healthy control group. Women comprised 60% of the sample. Inclusion criteria were as follows: (a) OCD participants were required to obtain ≥ 16 scores in Y-BOCS (Goodman et al., 1989); (b) GAD participants had to reach ≥ 56 in the Penn State Worry Questionnaire (PSWQ; Meyer, Miller, Metzger, & Borkovec, 1990); and (c) the control group (CG) could not present any current psychopathological disorder or have suffered throughout their lives from OCD or GAD or other disorders such as Personality Disorder, Schizophrenia Spectrum Disorder and other Psychotic Disorders, Bipolar Disorder, Nervosa Anorexia or Bulimia. They could not have a family history with any disorder which was the object of this research. Exclusion criteria of clinical groups were: (a) to suffer comorbidity with Bipolar Disorder, Schizophrenic Spectrum Disorders and other Psychotic Disorders, Personality Disorders, Anorexia, Bulimia, disorders related to substance and addictive dependence and Neurocognitive Disorders; and (b) be under 17 and over 65 years of age. Sample characteristics are presented in Table 1.
Sample measures.
| Characteristics | OCD (n=36) | GAD (n=31) | CG (n=28) | F/χ2 |
|---|---|---|---|---|
| Age (M±SD) | 35.75±1.45 | 30.45±0.88 | 33.92±10.58 | ns. |
| Sex n (%) | ns. | |||
| Men | 16 (44.4) | 11 (35.5) | 11 (39.3)17 (60.7) | |
| Women | 20 (55.6) | 20 (64.5) | ||
| Years of disorder duration (M±SD) | 14.19±11.35 | 4.85±4.07 | - | F(1, 66)=16.62; p<.001 |
| Comorbidity n (%) | ns | |||
| No comorbidity | 19 (57.6) | 13 (48.1) | - | |
| Comorbidity | 17 (42.4) | 18 (51.9) | - | |
| Marital status n (%) | ns | |||
| Single | 17 (47.2) | 20 (64.5) | 14 (50.0) | |
| Married | 16 (44.4) | 9 (29) | 13 (46.4) | |
| Divorced | 3 (8.4) | 2 (6.5) | 1 (3.6) | |
| Educational level n (%) | ns | |||
| Elementary | 7 (19.4) | 5 (16.1) | 5 (17.9) | |
| Secondary education | 7 (19.4) | 5 (16.1) | 6 (21.4) | |
| High school | 10 (27.9) | 8 (25.8) | 9 (32.1) | |
| University students | 12 (33.3) | 13 (42.0) | 8 (28.6) | |
| Psychiatric treatment | - | ns | ||
| Yes | 18 (50.0) | 14 (45.2) | ||
| No | 18 (50.0) | 17 (54.8) | - | |
| Psychological treatment | ns | |||
| Yes | 28 (77.8) | 26 (83.9) | - | |
| No | 8 (22.2) | 5 (16.1) | - | |
| Type of medication | ns | |||
| NoneAntidepressant | 18 (50)16 (44.6) | 17 (54.8)14 (45.2) | - | |
| Antipsychotic Antidepressant+antipsycotic | 1 (2.7)1 (2.7) | 00 | -- | |
| BAI (M±SD) | 18.91±10.29 | 24.45±13.53 | - | ns |
| BDI (M±SD) | 19.72±11.98 | 24.19±7.23 | - | ns |
| Categories (M±SD) | 46.06±11.89 | 49.61±6.75 | 56.85±10.88 | F (2, 94)=6.01; p=.003 |
| Uncertainty (M±SD) | 81.41±18.43 | 93.40±18.53 | 51.71±13.10 | F (2, 94)=45.09; p<.001 |
Note. n=number; SD: Standard deviation; ns: Not significant.
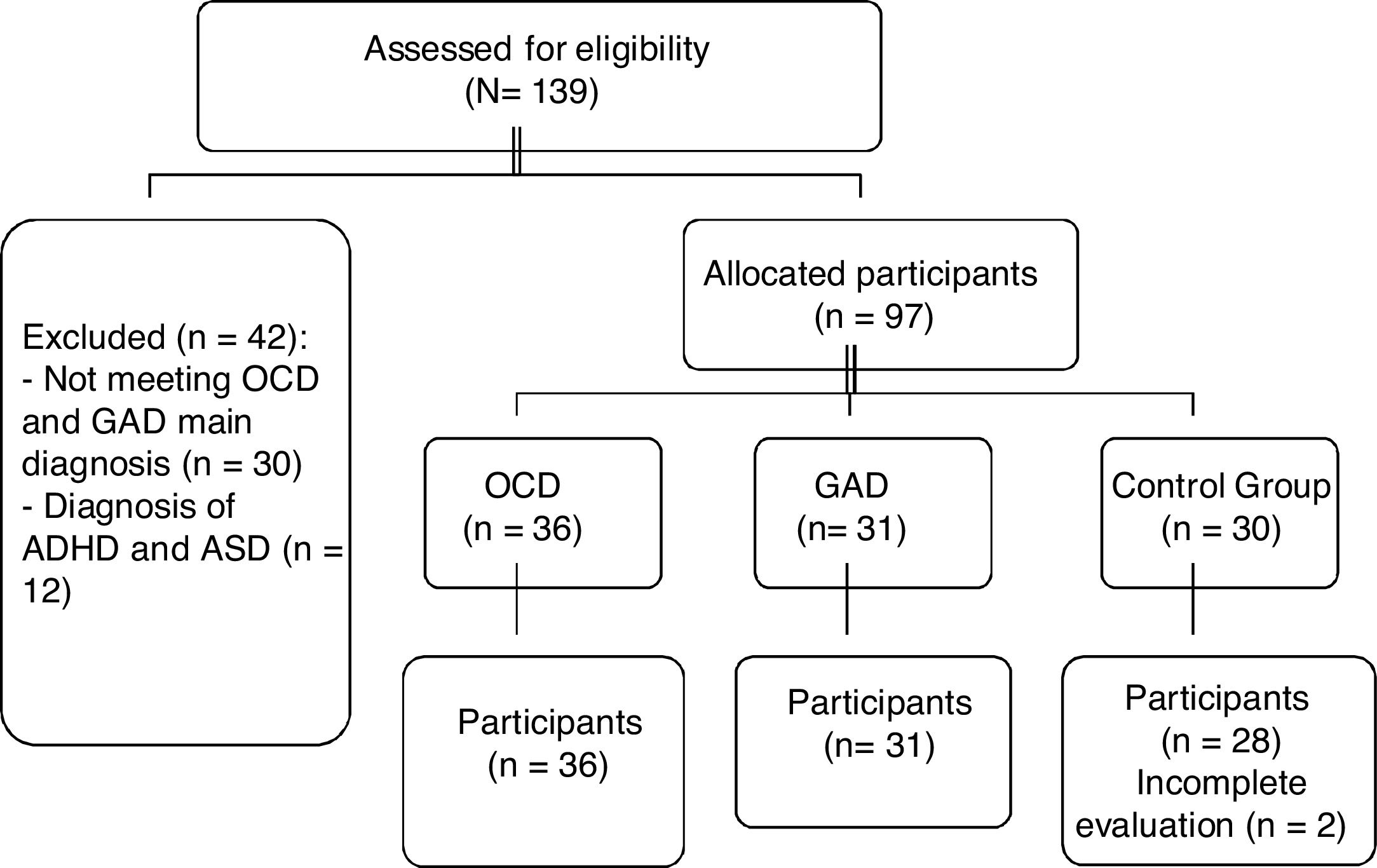
The study met ethical standards of the Declaration of Helsinki and has been approved by the Ethics Committee of the University of Murcia (Spain). All families provided written informed consent. The sample was recruited from two contexts: clinical and community. Once clinical groups were formed, the non-clinical group was recruited in order to be equal in age, sex and educational level through advertisements from the Applied Psychology Service of the University of Murcia. The procedure was as follows: (a) contact various mental health centers / hospitals / public and private clinics in the Regions of Murcia (n=7) and Castilla-La Mancha (n=5), Spain, from January 2017 to December 2018; (b) individual diagnostic interview, based on the DSM-5, by three clinical psychologists; and (c) assessment was in two 60-minute sessions by four clinical psychologists with more than 10 years of experience in these disorders who had been trained by fifth author for two sessions of one hour each. The test presentation order was the same for all participants. Participation was voluntary and free. Two patients in the control group withdrew as they did not wish to continue being assessed. Recruitment is shown in Figure 1.
Note. OCD: Obsessive Compulsive Disorder; GAD: Generalized Ansiety Disorde. ADHA: Attention deficit hyperactivity disorder; ASD: Autism spectrum disorder.
MeasuresClinical MeasuresProtocol socio-demographic variables.
Yale Brown Obsessive Compulsive Scale (Y-BOCS; Goodman et al., 1989). Comprising 10 items assessing severity of OCD. It has two subscales, Obsessions (range=0-20) and Compulsions (range=0-20) and a Total score (range=0-40). The scale has a high internal consistency (α=.87-.90), and good convergent validity (r=.74-.47). A total average greater than or equal to 16 is considered of clinical significance. Cronbach's alpha in this study was .87.
Penn State Worry Questionnaire (PSWQ; Meyer et al., 1990). Sixteen item self-report scale assessing the general tendency to worry especially present in Generalized Anxiety Disorder. The cut-off point for the detection of Generalized Anxiety Disorder is 56. It has been shown to have good psychometric properties, the correlation with other measures of anxiety being satisfactory, for example, the SAI-R, with a correlation of .76. Cronbach's alpha was high (α=.96).
Beck-II Depression Inventory (BDI; Beck, Steer and Brown, Sanz, & Valverde, 2011). Twenty and one item Self-report scale to measure depression severity. The internal consistency coefficient ranged between 0.87 and .89. Cronbach's alpha in this study was .91.
Beck Anxiety Inventory (BAI; Beck & Steer, 1996). Twenty and one item self-report scale to measure degree of anxiety. The internal consistency coefficients varied between .85 and .93. Cronbach's alpha was .92.
Intolerance of Uncertainty Scale (IUS; Freeston, Rhéaume, Letarte, Dugas, & Ladouceur, 1994). Comprising 27 items with five types of response (1: not at all characteristic of me, 5: entirely characteristic of me) which evaluates the tendency to react negatively on an emotional, cognitive and behavioral level to uncertain situations and events. The internal consistency coefficient was .91 and the test-restest reliability .78. Cronbach's alpha in this study was .94.
Neuropsychological measuresWisconsin Card Sorting Test (WCST; Heaton, Chelune, Talley, Kay, & Curtiss, 2001). Assess CF or attentional change using a set of cards. The most important measures are: Number of categories completed, Perseverative responses, Total errors, Perseverative errors and Non-perseverative errors. The T-score is used taking into account age and educational level. The psychometric properties of the WCST have been widely researched and it is a valid and reliable instrument, oscillating reliability coefficients between .39 and .72.
Stroop Color and Word Test (Golden, 1999). Assesses the ability to inhibit the automatic tendency to respond verbally and, therefore, control response to conflicting stimuli (words, colors, words / colors and interference). The test-retest reliability was .85, .81, .69
Go/No-go Task. Evaluates motor RI. It involves two stimuli (arrows of different colors and positions), one requiring a response (Go), and one requiring no response (NoGo). It has presented good convergent validity (r=.87).
Reynolds Intellectual Screening Test (RIST; Reynolds, Kamphaus, Fernández, & Pinto, 2009). It has its origin in the RIAS scales comprising two of its subtests: Guess (verbal subtest) and Categories (nonverbal subtest). In this study, only categories that measure nonverbal abstract reasoning were used. It maintains, like the RIAS, high test-retest reliability, .84.
Data analysisFirstly, Chi-square and one-factor ANOVA were used to examine potential group differences in clinical and demographic (age/gender) variables at pretreatment. Subsequently, multivariate analysis and post-hoc comparisons (Tukey or Games-Howel) of CF and RI were carried out. An analysis of covariance was performed when there were significant differences between groups in some variables considered influential in their performance. Independent samples Tests (Kruskal Wallis H test) were performed within each clinical group, taking into account the presence/absence of comorbidity and medication use. The Pearson correlation was used to analyze the relationship between variables. Cohen's ds (standardized mean differences) were calculated to estimate the magnitude of between-groups differences, 0.2 low, 0.5 medium, and 0.8 high. All participants were included in analyzes. SPSS Statistic 22.00 was used for statistical analysis.
ResultsEquivalence of groups in pretestGroups were equivalent in sex (p=.750), age (p=.170), marital status (p=.210) and educational level (p=.860). They presented differences in the Categories variable (p=.003) and Intolerance of Uncertainty (p=.000). Clinical groups only found significant differences in Duration of disorder variable (p=.000). See Table 1
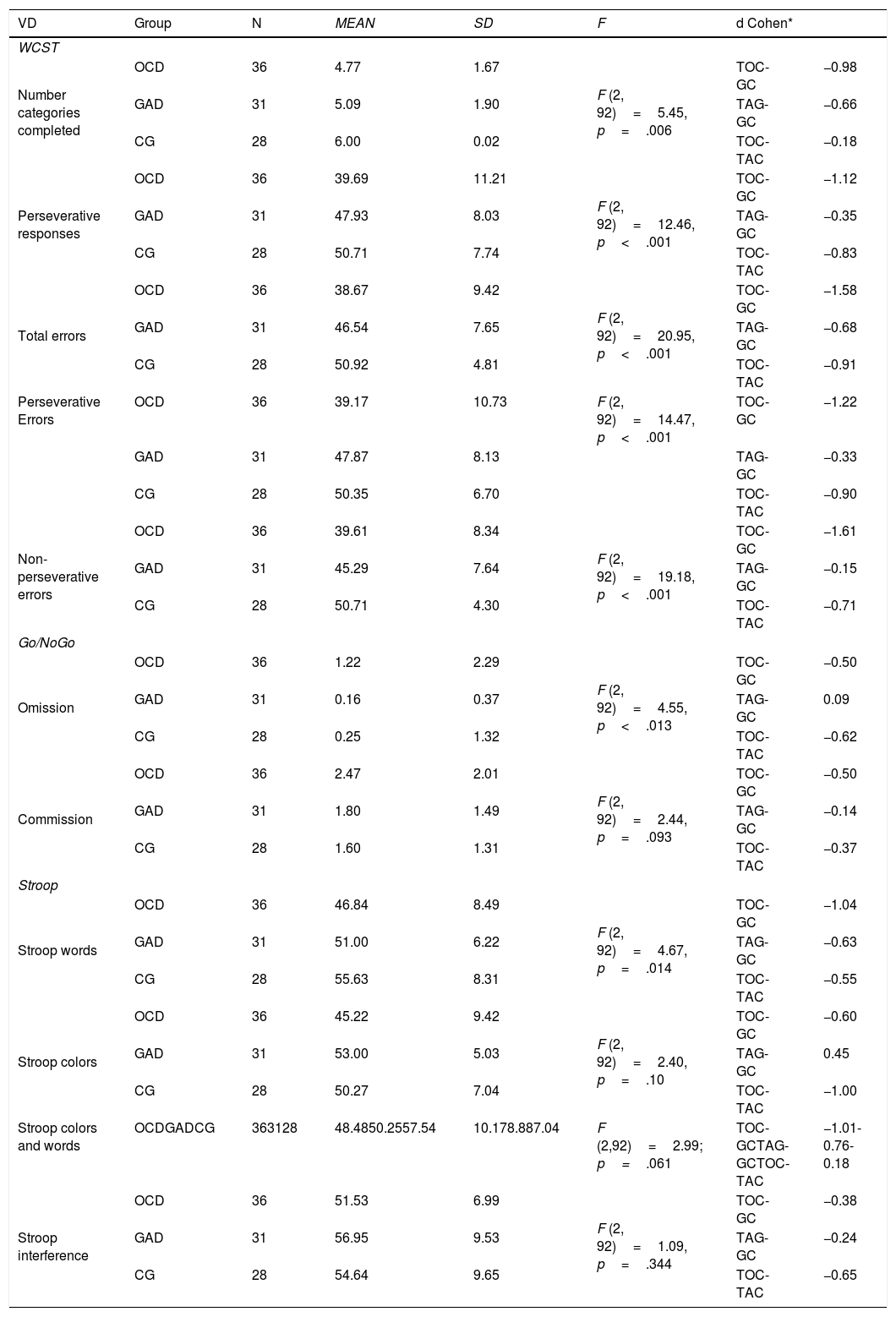
A Comparison with clinical groups and CG in CF and motor and cognitive inhibitionTable 2 shows the results of a multivariate analysis (MANOVA) on all variables. Comparison between the OCD and CG group obtained statistically significant differences in the following variables: Number of categories (p=.005), Perseverative responses (p<.001), Number of errors (p<.001), Perseverative errors (p<.001), Non-perseverative errors (p<.001), Errors of omission (p=.047) and Stroop words (p=.014), with the CG obtaining the best scores. The ES of measures evaluated with Wisconsin and Stroop words were high, compared to the average magnitude of Errors of omission.
MANOVA and EF of the variables of Wisconsin, Go / NoGo and Stroop.
| VD | Group | N | MEAN | SD | F | d Cohen* | |
|---|---|---|---|---|---|---|---|
| WCST | |||||||
| Number categories completed | OCD | 36 | 4.77 | 1.67 | F (2, 92)=5.45, p=.006 | TOC-GC | −0.98 |
| GAD | 31 | 5.09 | 1.90 | TAG-GC | −0.66 | ||
| CG | 28 | 6.00 | 0.02 | TOC-TAC | −0.18 | ||
| Perseverative responses | OCD | 36 | 39.69 | 11.21 | F (2, 92)=12.46, p<.001 | TOC-GC | −1.12 |
| GAD | 31 | 47.93 | 8.03 | TAG-GC | −0.35 | ||
| CG | 28 | 50.71 | 7.74 | TOC-TAC | −0.83 | ||
| Total errors | OCD | 36 | 38.67 | 9.42 | F (2, 92)=20.95, p<.001 | TOC-GC | −1.58 |
| GAD | 31 | 46.54 | 7.65 | TAG-GC | −0.68 | ||
| CG | 28 | 50.92 | 4.81 | TOC-TAC | −0.91 | ||
| Perseverative Errors | OCD | 36 | 39.17 | 10.73 | F (2, 92)=14.47, p<.001 | TOC-GC | −1.22 |
| GAD | 31 | 47.87 | 8.13 | TAG-GC | −0.33 | ||
| CG | 28 | 50.35 | 6.70 | TOC-TAC | −0.90 | ||
| Non-perseverative errors | OCD | 36 | 39.61 | 8.34 | F (2, 92)=19.18, p<.001 | TOC-GC | −1.61 |
| GAD | 31 | 45.29 | 7.64 | TAG-GC | −0.15 | ||
| CG | 28 | 50.71 | 4.30 | TOC-TAC | −0.71 | ||
| Go/NoGo | |||||||
| Omission | OCD | 36 | 1.22 | 2.29 | F (2, 92)=4.55, p<.013 | TOC-GC | −0.50 |
| GAD | 31 | 0.16 | 0.37 | TAG-GC | 0.09 | ||
| CG | 28 | 0.25 | 1.32 | TOC-TAC | −0.62 | ||
| Commission | OCD | 36 | 2.47 | 2.01 | F (2, 92)=2.44, p=.093 | TOC-GC | −0.50 |
| GAD | 31 | 1.80 | 1.49 | TAG-GC | −0.14 | ||
| CG | 28 | 1.60 | 1.31 | TOC-TAC | −0.37 | ||
| Stroop | |||||||
| Stroop words | OCD | 36 | 46.84 | 8.49 | F (2, 92)=4.67, p=.014 | TOC-GC | −1.04 |
| GAD | 31 | 51.00 | 6.22 | TAG-GC | −0.63 | ||
| CG | 28 | 55.63 | 8.31 | TOC-TAC | −0.55 | ||
| Stroop colors | OCD | 36 | 45.22 | 9.42 | F (2, 92)=2.40, p=.10 | TOC-GC | −0.60 |
| GAD | 31 | 53.00 | 5.03 | TAG-GC | 0.45 | ||
| CG | 28 | 50.27 | 7.04 | TOC-TAC | −1.00 | ||
| Stroop colors and words | OCDGADCG | 363128 | 48.4850.2557.54 | 10.178.887.04 | F (2,92)=2.99; p=.061 | TOC-GCTAG-GCTOC-TAC | −1.01-0.76-0.18 |
| Stroop interference | OCD | 36 | 51.53 | 6.99 | F (2, 92)=1.09, p=.344 | TOC-GC | −0.38 |
| GAD | 31 | 56.95 | 9.53 | TAG-GC | −0.24 | ||
| CG | 28 | 54.64 | 9.65 | TOC-TAC | −0.65 | ||
Note. OCD: obsesive-compulsive disorder; GAD: Generalized anxiety disorder; CG: Control group. ES: Effect size.
Comparison between GAD and CG only reached significant differences in variables: Number of categories completed (p=.034), Number of errors (p=.028), Non perseverative errors (p=.012), with better CG results. ES were medium and low. Comparisons between OCD and GAD clinical groups reached statistical significance in the following variables: Perseverative responses (p=.001), Number of errors (p<.001), Perseverative errors (p<.001), Non-perseverative errors (p=.005) and Errors of omission (p=.022), reaching the highest ES in Total errors and perseverative errors.
CF and IR controlling Nonverbal Reasoning and Uncertainty ToleranceSince the Categories variable (Nonverbal Reasoning) and Uncertainty obtained statistically significant differences between groups, an analysis of covariance was carried out. These variables only influenced measures evaluated with the Wisconsin, F (5, 87)=6.24, p=.000. The OCD group still presented statistically significant differences to the CG in Number of completed categories (p=.002), Number of errors (p<.001), Perseverative responses (p<.001), Perseverative errors (p<.001) and Non-perseverative errors (p<.001), with CG scores being better. Comparison between GAD and CG only reached significant differences in the following variables: Number of categories completed (p<.001), Number of errors (p=.001), Perseverative responses (p=.045), Non perseverative errors (p<.001), CG results being better. Comparisons between OCD and GAD clinical groups reached statistical significance in the following variables: Number of errors (p=.019), Perseverative responses (p=.015) and Perseverative errors (p=.007), with the GAD group obtaining better scores.
Duration of disorder, anxiety and depression as covariates in clinical groupsAs duration of disorder was significantly different in the clinical groups, an analysis of covariance was carried out controlling its influence on neuropsychological variables. Only variables measured with the Wisconsin, F (5, 60)=5.50, p<.001, obtained significant differences. The following variables reached statistical significance: Number of errors (p=.014), Perseverative responses (p=.001) and Perseverative errors (p=.001), with the GAD group obtaining better scores. The anxiety and depression variables were excluded as covariates as they did not present significant differences between groups.
Intragroup comparisons based on comorbidity and medication useIn the OCD group, no significant differences were found regarding comorbidity or medication use (p>.05).tGAD participants suffering from other comorbid disorders presented significant differences in Number of errors (p=.034), Stroop words (p=.003) and Stroop interference (p=.049), with higher performance in patients who only presented GAD. Type of medication influenced variables: Number of categories completed (p=.017), Non-perseverative errors (p=.001), Errors of omission (p=.005), Errors of commission (p=.041) and Stroop colors (p=.002). Participants who did not take medication performed better.
Correlation between CF and Inhibition and Obsessions and WorryThe OCD group only presented significant relationships between scores in OCI-R and Errors of commission (r=-.45, p=.016) the higher the score in obsessions the smaller number of errors.tThe GAD group achieved significant correlations between the scores of the Penn State Worry Questionnaire and Stroop colors (r=-.54, p=.003) and those worries and interference (r=-.39, p=.042), with Worry a variable that negatively influenced results.
Discussion and conclusionsOur first aim was to analyze differences in response inhibition and CF among patients with OCD, GAD and a healthy CG. The most frequently used test for assessing CF is the WCST with Perseverative Errors and Number of categories completed being the main signs of dysfunction (Teubner-Rhodes et al., 2017). In this study, the OCD group presented lower scores in CF tasks, consistent with other studies (Dittrich & Johansen, 2013). This clinical group also reported more Errors of omission, perhaps reflecting problems of control or attention maintenance and fewer words read (Stroop words) indicating slow reading. ES achieved in CF were high, while medium in motor inhibition and low in cognitive inhibition, following the trend seen in other studies (Shin et al., 2014, Snyder et al., 2015, Yazdi Ravandy et al., 2018). The GAD Group presented differences to the CG in Number of completed categories, Number of errors, Non-perseverative errors, with medium and medium-low ES. Therefore, lower performance was reported in CF although their scores were not very low. Comparison between OCD and GAD groups indicated lower CF in the former, not consistent with the study by Kim et al. (2019) which reported lower CF in the GAD group; however, those results were influenced by comorbidity and medication use. Therefore, CF results could explain essential OCD symptomatology, repetitive thought pattern and great difficulty for change, leading to problems in facing situations.
Contrary to expectations, no differences were found between groups in Cognitive Inhibition (Stroop interference) and motor (Go/NoGo - Errors of commission), coinciding with the study by Leonard and Abramovitch (2018) and partially with research by Hallion et al. (2017). In the latter, good performance was obtained in the Go/NoGo task in GAD patients although they presented deficiencies in Cognitive Inhibition, related to anxiety severity, rather than diagnosis. These results could be in line with those of Carver, Johnson, and Timpano (2017), suggesting that psychopathology, emotional reactivity and availability of cognitive resources are factors that may influence cognitive functions, and to a lesser degree diagnostic entity. Another explanation might be compensatory processes in simpler tasks allowing normal performance despite substantial anomalies in underlying capacities. Brain imaging studies and observation of altered brain activity patterns in patients during task performance would enable identification of the key brain circuits involved.
Our second aim was to assess whether differences observed could be due to the Categories variable (Non-verbal reasoning) and Tolerance of uncertainty. Results remained the same in CF but no differences were found between the OCD-CG groups in Errors of omission and Stroop words. The GAD-CG group comparison maintained previous results, while differences in Errors of omission between both clinical groups ceased to exist, the results remained the same. It therefore appears that Nonverbal Reasoning and Tolerance of uncertainty specifically affect reading speed and attention. These results are consistent with research by Kim et al. (2018).
The third aim was to verify whether duration of disorder and intensity of anxiety and depression influenced results between the two clinical groups (OCD-GAD). As anxiety and depression levels were equal in clinical groups, no further analysis was performed. Duration of disorder was different in each clinical group, so it was included as a covariate, observing that results remained the same, the OCD group having lowest CF scores, supporting findings by Geller et al. (2018). However, the relationships between these variables and the years of duration of the problem were not significant, coinciding with Kim et al. (2019).
The fourth aim was to analyze if there were EF differences within each clinical group (OCD and GAD) due to comorbidity and medication use. No differences were found in the OCD group regarding EF performance assessed among participants with and without comorbidity. In the meta-analysis by Snyder et al. (2015) the same results were seen, unlike the GAD group where comorbidity influenced a lower number of errors and less Interference. Likewise, medication use influenced CF and motor Inhibition. Participants who did not take medication committed fewer errors. In conclusion, the OCD group findings are consistent with previous studies indicating that neither medication nor comorbidity influence executive performance (Hallion et al., 2017; Snyder et al., 2015). Regarding the GAD group, Kim et al. (2018) also observed that medication and severity affected CF results. Thus, when controlled, these results improved (Wersebe et al., 2018).
The final aim was to analyze the relationship between CF and Inhibition with Obsessions and Worry. The OCD group only presented significant relationships between OCI-R and Errors of commission. The higher the score in obsessions, the lower motor inhibition was seen to be. These results are consistent with those of Abramovitch et al. (2018). The GAD group achieved significant correlations between scores in Worry and Stroop colors and Cognitive inhibition. This raises the question why obsessions were related to a Go/NoGo task and Worry with a Stroop task. This is perhaps due in part to subtle differences in task demands and underlying neural circuits. While the Go/NoGo task only requires participants to inhibit motor responses, the Stroop task includes an element of cognitive inhibition.
As clinical implications, we can highlight that including CF within the treatment would perhaps allow more effective interventions, being a novel approach to treating both OCD and GAD patients. The inclusion of specific modules on flexibility would enhance the effectiveness of exposure with response prevention, improving adherence to treatment and avoiding abandonment. Another aspect to take into account is that perhaps we are facing a transdiagnostic process, although there is a greater or lesser involvement in patients. An important variable to work on these patients would be tolerance of uncertainty in order to restructure the beliefs that ambiguous situations are exhausting and disturbing, that unexpected events are negative and should be avoided since they influence the performance of some executive functions. Therefore, cognitive therapy is used together with exposure within the treatment of these disorders. Based on the results, we can ask whether we are facing specific domains of OCD and GAD, or before processes common to other disorders.
This study has some limitations, such as non-random selection of participants, small sample size preventing us from analyzing results according to obsession / compulsion subtypes, design type (cross-sectional), use of only one evaluation tool for each variable. In future studies, other aspects of cognitive functions could be analyzed and assessed with different instruments and tasks. It is recommended that with a larger sample size, studies be performed on types of obsessions / compulsions and EF performance.
FundingThis article was supported by the Ministerio de Economía and Competitividad of the Spanish Government (Project PSI2016-78185-P).