Background/Objective: Retirement homes and other gerontology services are frequently criticized due to their lack of flexibility and tailored attention, leading to homogeneous treatment which compromises patients’ control of their lives. This study aims to develop and validate the first Spanish instrument for healthcare professionals to assess the degree of person-centered attention delivered by senior care centers. Method: A total of 844 healthcare professionals (mean age=39.94 years old; SD=10.56) with a mean of 6.56 years (SD=6.15) of work experience participated in the study. The psychometric properties of the questionnaire developed were analyzed using both classical test theory and item response theory models. Results: The internal structure was unidimensional with an explained variance of 55.23%. Reliability was outstanding: internal consistency (α=.96, ω=.96) and test-retest (r=.88; ICC=.93). The total score was significantly correlated with two similar questionnaires, with associated variance of 58.83% and 55.20% respectively. Conclusions: The new instrument allows healthcare professionals to assess the level of person-centered care provided by gerontology centers with excellent reliability and validity.
Antecedentes/Objetivo: Las residencias y otros servicios gerontológicos son frecuentemente criticados por su falta de flexibilización y personalización en la atención, conduciendo a un trato uniforme que dificulta el control sobre sus vidas. El objetivo del trabajo es desarrollar y validar el primer instrumento de medida español que permite a los profesionales de la salud evaluar en qué medida se lleva a cabo en su centro una atención centrada en la persona. Método: Participaron en el estudio 844 profesionales de la salud (edad media=39,94; DT=10,56) con una experiencia media de 6,56 años (DT=6,15). Las propiedades psicométricas del instrumento desarrollado se analizaron mediante modelos de Teoría Clásica de los Test y de Teoría de Respuesta a los Ítems. Resultados: La prueba resultó esencialmente unidimensional, con un primer factor que explica el 55,23% de la varianza. La fiabilidad es excelente, tanto la consistencia interna (α=0,96, ω=0,96) como la estabilidad (r=0,88; ICC=0,93). La puntuación total correlacionó significativamente con dos cuestionarios similares, obteniéndose una varianza asociada de 58,83% y 55,20%, respectivamente. Conclusiones: El nuevo instrumento desarrollado permite a los profesionales de la salud evaluar con excelente fiabilidad y validez el nivel de atención centrada en la persona de los centros gerontológicos.
The aging of the population requires the provision of various care services to dependent individuals, leading to a growing concern about the quality of these services (Brandolim et al., 2018; Zubritsky et al., 2013). Retirement homes and other gerontology services are frequently criticized due to their excessive focus on the “illness”, lack of tailored attention, lack of privacy, lack of significant activities, or lack of integration into the community (Colomina et al., 2018; Koren, 2010; Sapranaviciute-Zabazlajeva et al., 2018; Schürmann & Margraf, 2018). The person-centered care approach (PCC) has recently become considered fundamental to improving the quality of health services and care for older people. The World Health Organization has underlined the need to move toward comprehensive, person-centered care, considering it a central approach to improving the quality and efficacy of care of elderly people (World Health Organization WHO, 2015).
PCC comprises two dimensions widely supported by the literature: (1) care and priority objectives (e.g., respect and appreciation of each person as a unique, valuable individual, knowledge of each individual's history and lifestyle, support of people's autonomy), and (2) the enabling environment that promotes or hampers these objectives (e.g., individualized care, physical space design, organizational-related variables) (Edvardsson & Innes, 2010; White, Newton-Curtis, & Lyons, 2008). However, due to the lack of consensus about the definition of PCC (Edvardsson & Innes, 2010; McCormack, 2004) various instruments have been developed to assess it (de Silva, 2014; Edvardsson & Innes, 2010; Martínez, Suárez-Álvarez, & Yanguas, 2016; Ree, Wii, Manse, & Storm, 2019). These instruments can be classified in three groups: (1) systematic observation of the care delivered, (2) surveys targeting service users, and (3) surveys targeting health professionals (de Silva, 2014). The most widely-used instrument in the first group is Dementia Care Mapping (DCM) (Brooker & Surr, 2007; Wylie, Madjar, & Walton, 2002), which has been adapted to Spanish retirement homes (Vila, Villar, Celdrán, & Fernández, 2012). The instruments assessing users’ views have had limited development due to the presence of cognitive impairments and dementias in users, which have hampered participants’ involvement. Thus, to date there is a lack of Spanish adaptations of any instrument assessing users’ views of PCC. Finally, the most widely-used questionnaires for healthcare professionals are The Person-centered Care Assessment Tool (P-CAT) (Edvardsson, Fetherstonhaugh, & Gibson, 2010), and The Staff Assessment Person Directed Care (White et al., 2008), both with available adaptations to Spanish elderly care centers and day care centers (Martínez, Suárez-Álvarez, Yanguas, & Muñiz, 2016a, 2016b).
Despite the existing instruments, there are still several limitations and challenges to consider, such as the lack of an operative definition of PCC (Ree et al., 2019) and its multidimensionality, which calls for a combination of assessment instruments and approaches (Bowman & Schoeneman, 2006; de Silva, 2014; van Haitsma et al., 2014). Moreover, the key roles of users, relatives and staff make it necessary to develop comprehensive surveys to collect their views (de Silva, 2014). The paucity of Spanish validations in the field poses an important obstacle to research assessing the implementation of PCC in retirement homes and other senior centers. The new measurement instrument developed seeks to evaluate exhaustively the ten components of person-centered care (Martínez, 2017, 2018), thus overcoming a serious limitation of the tools available in Spanish (Martínez, Suárez-Álvarez, Yanguas et al., 2016a, 2016b).
The PCC-gerontology model (Martínez, 2017, 2018) aims to overcome existing limitations and provide instruments adapted to Spanish residential services that allow the performance of both research and quality assessment of services provided. To achieve this goal, based on the assessment model proposed by White et al. (2008), the PCC-gerontology model defines the construct of PCC using ten components organized into two dimensions: person-centered practice (activities organized by staff and informal daily communications), and PCC enabling environment (key elements facilitating/hindering person-centered practices). The first dimension comprises the following components: Knowledge, Autonomy, Communication, Personalization/wellness, and Privacy. The components in the second dimension are: Daily activity, Physical space, Family and friends, Community, and Organization. The definition and structure of these ten components were validated by a group of 22 national experts in gerontology and PCC. On a scale of 0 to 10, the experts scored the relevance of each of the ten components of the PCC model, obtaining excellent scores, whose averages ranged from 8.57 for the Community component, and 9.91 for Knowledge and Organization (Martínez, 2017, 2018). Based on the proposed model, a group of six experts, three in psychometrics and three in PCC, generated the corresponding items for the ten dimensions. The PCC-gerontology model integrates the views of users, relatives, staff and supervisors through a set of standardized instruments, allowing the comparison of independently collected information: (a) A guide for participating in internal reviews ‘Move Forward in PCC’, (b) PCC-G questionnaire for external evaluation, and (c) PCC-G view surveys in four versions: elderly people, relatives, director of the center, and staff.
The main goal of this study is to present the first instrument developed in Spain to assess the views of staff about the level of implementation of person-centered care in their workplaces. This new measurement tool was developed following the most recent psychometric advances in test development (American Educational Research Association, American Psychological Association, & National Council on Measurement in Education, 2014; Downing, 2006; Downing & Haladyna, 2006; Drasgow, 2016; Irwing, 2018; Lane, Raymond, & Halayna, 2016; Muñiz & Fonseca-Pedrero, 2019; van der Linden, 2016). The psychometric properties of the instrument were explored in detail, including reliability and validity evidence, using the classical test theory approach (CTT), and item response theory models (IRT). The new instrument allows detailed data to be gathered about the views of healthcare staff on the level of person-centered care provided, which represents a milestone for the implementation of the PCC-gerontology model in Spain and other Spanish-speaking countries.
MethodParticipantsA total of 844 healthcare professionals (mean age=39.94 years old; SD=10.56), with a mean of 6.56 years (SD=6.15) of work experience, participated in the study. Most worked as elderly care providers (n=576, 68.3%), followed by interdisciplinary team technicians (n=267, 31.7%). They were from various Spanish regions: Asturias (n=230, 27.3%), Castilla and León (n=156, 18.5%), The Canary Islands (n=140, 16.6%), The Basque Country (n=123, 14.6%), Galicia (n=93, 11%), Castilla-La Mancha (n=40, 4.7%), Andalucía (n=39, 4.6%) and Aragón (n=23, 2.7%). These data indicate that the study participants are a nationally representative sample so potential findings can be generalizable to the community.
MeasuresDemographic and work-related characteristics. Data were collected about age, residence, job, working experience, job satisfaction and quality of care provided by their center.
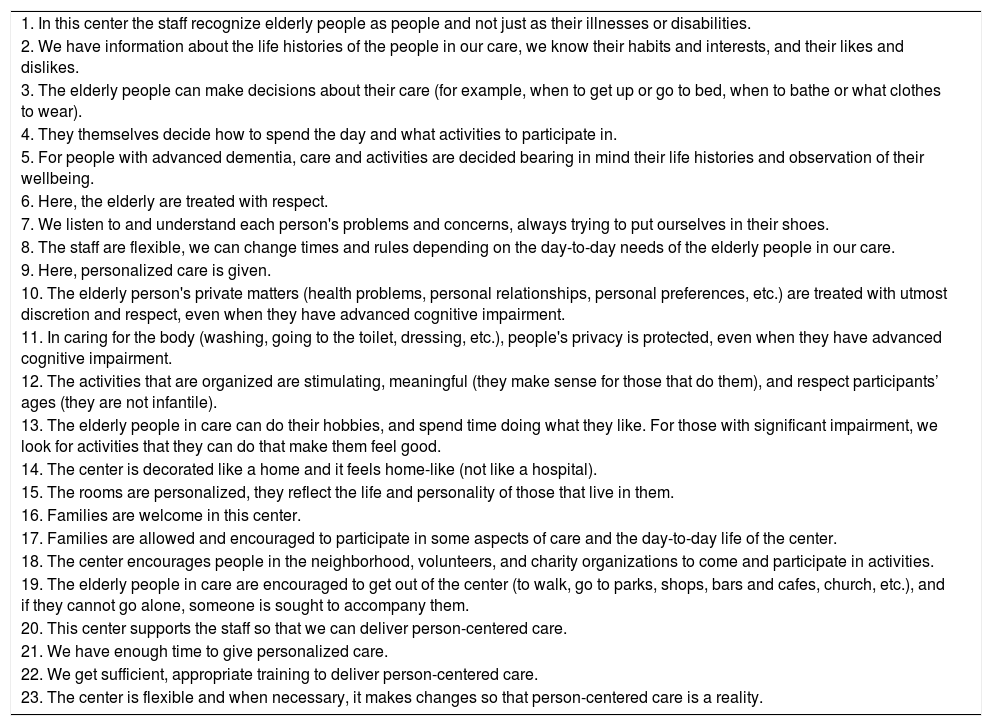
Person-centered Care Gerontology Staff questionnaire (PCC-G-Staff). The questionnaire was developed following the guidelines of recent psychometric advances (American Educational Research Association et al., 2014; Downing, 2006; Downing & Haladyna, 2006; Drasgow, 2016; Irwing, 2018; Lane et al., 2016; Muñiz & Fonseca-Pedrero, 2019; Suárez-Álvarez et al., 2018; van der Linden, 2016). Two items were developed for each of the ten components of the PCC model previously described (Martínez, 2017, 2018; White et al., 2008). A group of six experts, three psychometricians and three PCC experts, carried out the selection and writing of the items, initially proposing two for each component of the hypothetical model. Due to the lack of items assessing indirect autonomy in individuals with advanced cognitive impairment, a third item was included in the “Autonomy” component. Also, due to the importance of the organizational component and the variety of aspects to be considered (e.g., training, time, support), two additional items were included in the “Organization” component. The first version comprised 23 Likert-type items (1=totally disagree, 10=totally agree). In order to ensure that the professionals at whom the measurement instrument was aimed understood the items perfectly and unambiguously, a pilot study was carried out. For this purpose, the first version described was applied to a sample of seven professionals specialized in healthcare. They were asked to comment on potential comprehension difficulties of the items by the professionals, and to make, where appropriate, suggestions to improve the wording. Following the suggestions of Wilson (2005), after conducting the test the seven professionals were interviewed individually, and all of them confirmed that all the items were easy to understand. However, based on their suggestions some minor corrections of grammatical order were made to some items, although these modifications did not affect the substantive content of the items. After the pilot study, the final version of the test was created, which was to be subjected to validation (see Table 1).
Items in the new tool (PCC-G-Staff).
| 1. In this center the staff recognize elderly people as people and not just as their illnesses or disabilities. |
| 2. We have information about the life histories of the people in our care, we know their habits and interests, and their likes and dislikes. |
| 3. The elderly people can make decisions about their care (for example, when to get up or go to bed, when to bathe or what clothes to wear). |
| 4. They themselves decide how to spend the day and what activities to participate in. |
| 5. For people with advanced dementia, care and activities are decided bearing in mind their life histories and observation of their wellbeing. |
| 6. Here, the elderly are treated with respect. |
| 7. We listen to and understand each person's problems and concerns, always trying to put ourselves in their shoes. |
| 8. The staff are flexible, we can change times and rules depending on the day-to-day needs of the elderly people in our care. |
| 9. Here, personalized care is given. |
| 10. The elderly person's private matters (health problems, personal relationships, personal preferences, etc.) are treated with utmost discretion and respect, even when they have advanced cognitive impairment. |
| 11. In caring for the body (washing, going to the toilet, dressing, etc.), people's privacy is protected, even when they have advanced cognitive impairment. |
| 12. The activities that are organized are stimulating, meaningful (they make sense for those that do them), and respect participants’ ages (they are not infantile). |
| 13. The elderly people in care can do their hobbies, and spend time doing what they like. For those with significant impairment, we look for activities that they can do that make them feel good. |
| 14. The center is decorated like a home and it feels home-like (not like a hospital). |
| 15. The rooms are personalized, they reflect the life and personality of those that live in them. |
| 16. Families are welcome in this center. |
| 17. Families are allowed and encouraged to participate in some aspects of care and the day-to-day life of the center. |
| 18. The center encourages people in the neighborhood, volunteers, and charity organizations to come and participate in activities. |
| 19. The elderly people in care are encouraged to get out of the center (to walk, go to parks, shops, bars and cafes, church, etc.), and if they cannot go alone, someone is sought to accompany them. |
| 20. This center supports the staff so that we can deliver person-centered care. |
| 21. We have enough time to give personalized care. |
| 22. We get sufficient, appropriate training to deliver person-centered care. |
| 23. The center is flexible and when necessary, it makes changes so that person-centered care is a reality. |
Person-Centered Care Assessment Tool (P-CAT). The Spanish version of P-CAT (Martínez, Suárez-Álvarez, Yanguas, & Muñiz, 2016a) was used to examine validity evidence for the PCC-G-Staff questionnaire. The P-CAT is a 13 item Likert type questionnaire (1=totally disagree, 5=totally agree) designed to assess environmental and organizational preconditions for patient involvement in quality improvement. The Spanish validation of the P-CAT (Martínez et al., 2016a) has shown good reliability (α=.88). In the present study, the internal consistency was also good (α=.85).
Person-directed Care (PDC). The Spanish staff assessment version of the PDC (Martínez, Suárez-Álvarez, Yanguas et al., 2016b was also used to gather validity evidence for the PCC-G-Staff questionnaire. It comprises 50 Likert-type statements (1=never or almost never to 5=Always or nearly always) to evaluate the level of person-centered care provided by different facilities. Data from the Spanish validation of the questionnaire (Martínez, Suárez-Alvarez, Yanguas et al., 2016b) showed excellent internal consistency (α=.96). In the present study, the reliability was very good in both the total score (α=.96), and the Person-centered and Environmental subscales (α=.95 and α=.91, respectively).
ProcedureContact was made with the management of various private and public residential care centers, as well as organizations in the sector, informing them about the study and inviting their participation. They were also sent a letter outlining the study objectives, methodology and the obligations of all involved in the study. The inclusion criteria were: (a) that the center appeared in the register of residential care centers authorized by the relevant autonomous community, (b) that it was a center dedicated to long-term care due to situations of dependence, and (c) that they accepted the stipulated obligations of participation in the study. Exclusion criteria were: (a) centers which exclusively offered care to those with a high level of independence and autonomy, (b) palliative care, acute care or convalescent units, and c) exclusively short-stay or temporary care centers.
Following this first contact, we confirmed the participation of 40 residential centers in the autonomous communities mentioned above. In the interests of good data collection and high participation, each center designated a member of staff who was responsible for coordinating the data collection process. A total of 1,200 test booklets were sent and 844 were returned (response rate=70%).
In order to ensure the awareness and consistency of the process, we prepared an instruction document describing the data collection process. These instructions were sent to the director of each center along with the designated coordinating staff member. We maintained contact by telephone and email to answer any questions prior to test application. We also maintained contact with each member of staff responsible for the application of the tests in the 40 centers, as well as the managers of each center. Responding to the questionnaires was done individually; they were distributed by each center coordinator to the various members of staff who had agreed to participate. The instructions indicated that the responses should be completed and returned within two days.
All of the staff directly caring for patients in a center were invited to participate. These were elderly care staff who, regardless of their weekly hours, always give direct care to users of the service. Indirect staff such as cleaners, caretakers or administrators did not take part, nor did staff in services such as the cafeterias, hairdressing or chiropody. Staff who had been working at the center for less than one month were also excluded. Data collection lasted 10 months, between May 2017 and March 2018. A total of 176 staff (in 8 centers) did two applications of the ACP-G questionnaire 7 days apart in order for us to be able to analyze test-retest reliability. Participation was anonymous, voluntary and entirely confidential. Staff did not receive any remuneration or compensation for participating. The coordinators were sent a certificate accrediting their collaboration following data collection. In addition, each director was sent a letter summarizing the results from their center, fulfilling one of our obligations to them.
The study was not explicitly reviewed by an ethics committee given that the participants evaluated were adults, the evaluation was voluntarily agreed to and the data treated anonymously and confidentially. Additionally, all the recommendations established in the ISO-10667 standard for the evaluation of people and the International Test Commission (ITC) Guidelines on Test Use (International Test Commission ITC, 2013) were strictly followed.
Data analysesOf the 844 participants, 23 (2.7%), 38 (4.5%) and 159 (18.8%) presented missing data in at least one item of the PCC-G-Staff, P-CAT and PDC, respectively. Only one participant of the 176 completing the PCC-G-Staff re-test presented missing data in one item. Due to the high percentage of missing data in some questionnaires, imputation of missing values was performed. A linear regression method was used to impute missing data, under the assumption of data missing completely at random. This imputation method was used for its good functioning in psychometric contexts such as this study, in both situations of data that are missing completely at random (MCAR) and missing at random (MAR) (Cuesta & Fonseca-Pedrero, 2014; Cuesta, Fonseca-Pedrero, Vallejo, & Muñiz, 2013).
To analyze the factorial structure of the test, we proceeded in three phases, dividing the total sample into three random subsamples. The first subsample, composed of 244 participants, was used to perform an exploratory factor analysis. The second, composed of 300 participants, was used to fit a confirmatory factorial model, and the third subsample, also of 300 participants, was used to verify the stability of the confirmatory model that was fitted in the previous phase. In the first subsample, an exploratory factor analysis was carried out on the matrix of polychoric correlations. Unweighted Least Squares (ULS) was used as an extraction method, and the number of factors to be retained was determined by the optimal implementation of parallel analysis (Timmerman & Lorenzo-Seva, 2011), the percentage of variance explained, and the model fit indices based on the study of residuals (GFI and RMSR), as these analyses are the most suitable regardless of the method of estimation (Ferrando & Lorenzo-Seva, 2017). Model fit is considered adequate when GFI is greater than 0.09 and RMSR is less than 0.08 (Kline, 2011). Indices of closeness to unidimensionality were also used, Unidimensional Congruence (UniCo), Explained Common Variance (ECV) and Mean of Item Residual Absolute Loadings (MIREAL). Data can be treated as essentially one-dimensional when UniCo>.95, ECV>.85 or MIREAL<.30 (Ferrando & Lorenzo-Seva, 2018). In the second subsample, a confirmatory factor analysis was carried out with a single factor. Modification indices were used to select the items in which the correlation between errors was allowed, in order to achieve a better fit. The items were treated as categorical variables and the estimation method used was WLSMV. As fit indices, χ2/df, and CFI were used. In the third subsample, the model that was fitted in the previous phase was tested, in order to check the stability of the solution reached.
Reliability was estimated by procedures of internal consistency (Cronbach's alpha, McDonald's omega), calculated using the polychoric correlation matrix, thus making use of the ordinal properties of the data (Oliden & Zumbo, 2008). Temporal stability (test-retest) was estimated using the Pearson correlation and the intra-class correlation coefficient (ICC). Pearson correlations between the total scores of the PCC-G-Staff, the P-CAT, the PDC and its two subscales were performed in order to obtain evidence of validity in relation to other variables.
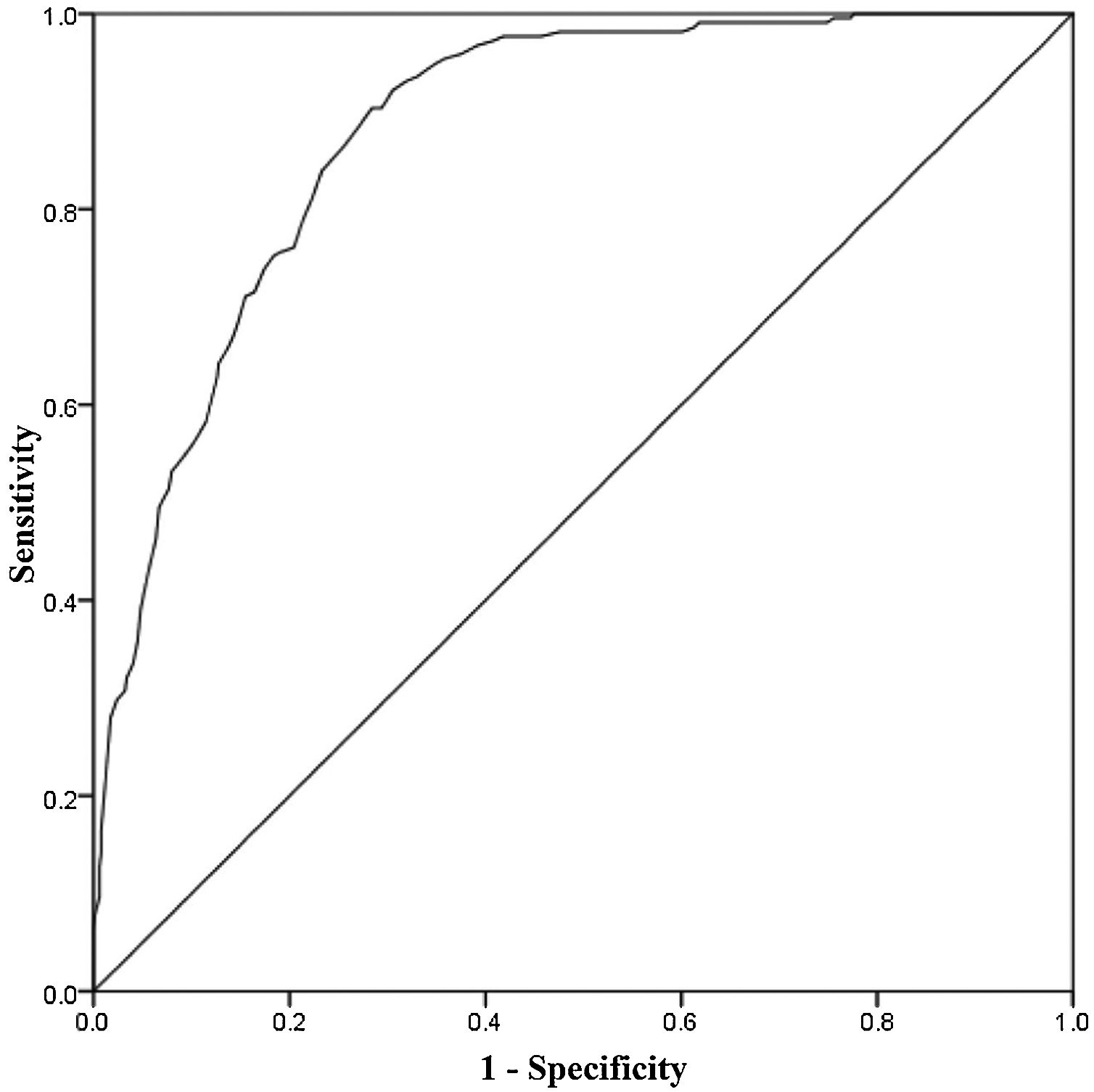
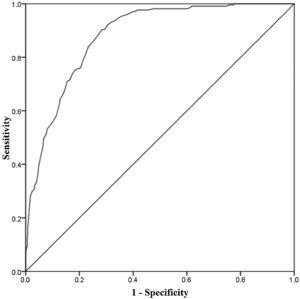
With the aim of providing useful information for clinical practice, the receiver operating characteristic curve (ROC) was used to provide the optimum cut-off point for maximizing both sensitivity and specificity in detecting person-centered care practices. We used a composite measure combining both P-CAT and PDC total scores as the validity criterion, with the cut-off established at the 75th percentile. The Youden Index was used to calculate the PCC-G-Staff cut-off, following the formula:
Equation (1) shows the relationship between the optimum cut-off (Y) and its associated sensitivity (S) and specificity (Sp). In addition, percentiles associated with each PCC-G-Staff direct score were calculated.
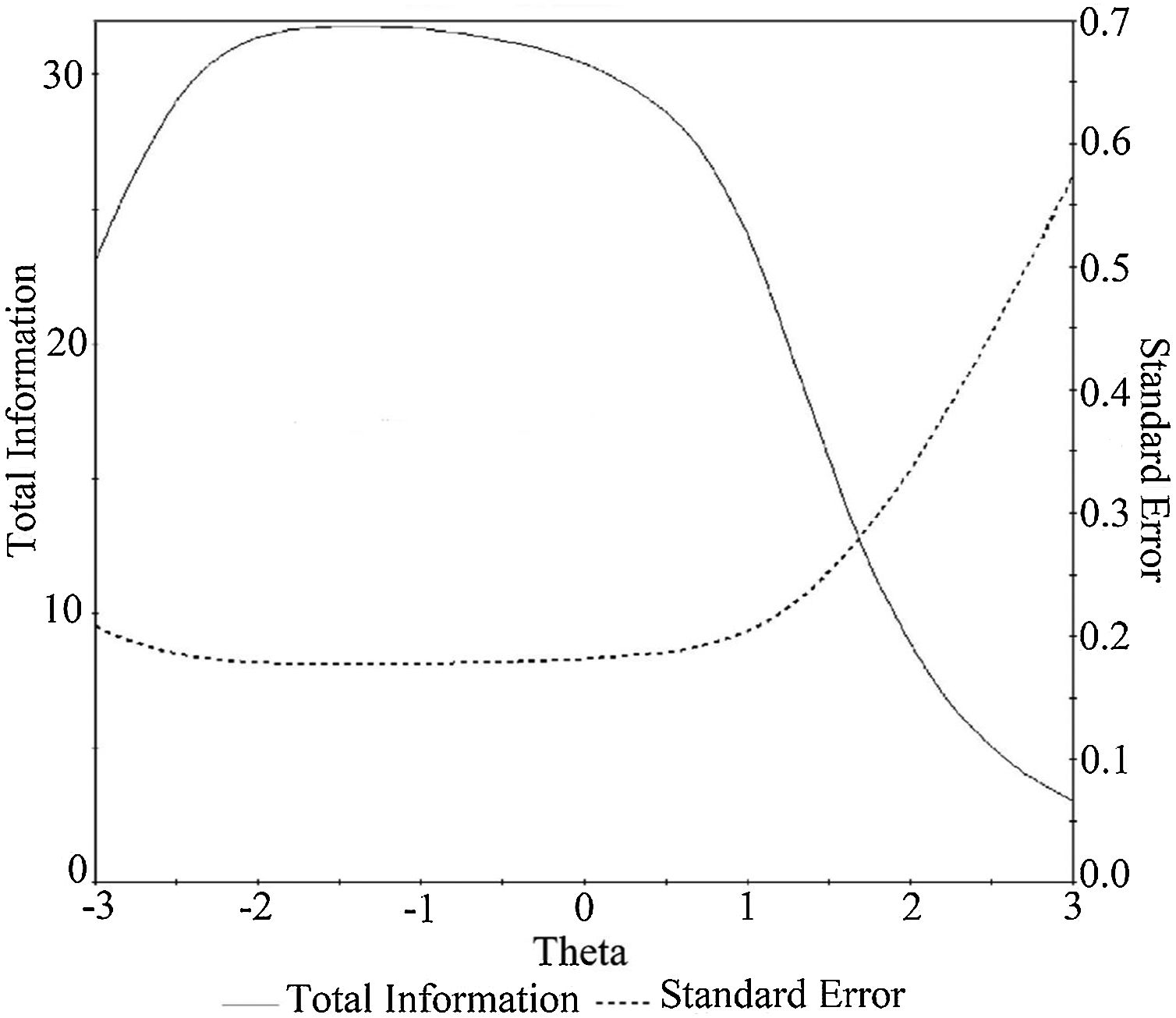
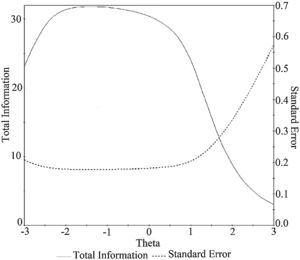
Finally, Samejima's Graded Response Model within the IRT framework (Samejima, 1968) was used to calculate the information function of the PCC-G-Staff. Data analyses were performed using the statistical software packages SPSS 24 (IBMCorp, 2016), FACTOR 10.5.03 (Lorenzo-Seva & Ferrando, 2013), IRTPRO .4.2 (SSI, Inc, 2017), and MPlus8 (Muthen & Muthen, 2017).
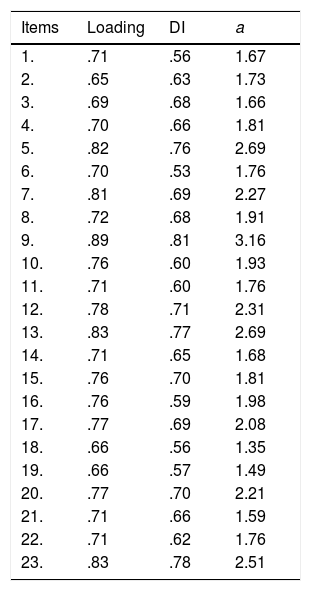
ResultsDescriptive scale dataThe total score had a mean of 176.12 (SD=34.13). Due to the Kolmogorov-Smirnov test's sensitivity to larger sample sizes, normality was examined using the Q-Q plot and values of kurtosis (K) and skewness (S) lower than 7 and 2, respectively (Kim, 2013). The total score exhibited a normal distribution (K=0.036; S=-0.69). Discrimination indices were over .35 (see Table 2).
Factor loadings of the PCC-G-Staff items, discrimination indices and discrimination parameter a of IRT.
| Items | Loading | DI | a |
|---|---|---|---|
| 1. | .71 | .56 | 1.67 |
| 2. | .65 | .63 | 1.73 |
| 3. | .69 | .68 | 1.66 |
| 4. | .70 | .66 | 1.81 |
| 5. | .82 | .76 | 2.69 |
| 6. | .70 | .53 | 1.76 |
| 7. | .81 | .69 | 2.27 |
| 8. | .72 | .68 | 1.91 |
| 9. | .89 | .81 | 3.16 |
| 10. | .76 | .60 | 1.93 |
| 11. | .71 | .60 | 1.76 |
| 12. | .78 | .71 | 2.31 |
| 13. | .83 | .77 | 2.69 |
| 14. | .71 | .65 | 1.68 |
| 15. | .76 | .70 | 1.81 |
| 16. | .76 | .59 | 1.98 |
| 17. | .77 | .69 | 2.08 |
| 18. | .66 | .56 | 1.35 |
| 19. | .66 | .57 | 1.49 |
| 20. | .77 | .70 | 2.21 |
| 21. | .71 | .66 | 1.59 |
| 22. | .71 | .62 | 1.76 |
| 23. | .83 | .78 | 2.51 |
Note. DI: discrimination index items; a: IRT parameter a.
The factorial structure of the scale was studied in three phases. An EFA was applied to a subsample of 244 subjects. The Kaiser-Meyer-Olkin index had a value of .93 and the Bartlett test was statistically significant (χ2(253)=4186.70, p<.001), which indicates that the data were adequate for the analysis to be performed. The parallel analysis suggested a single factor with an explained variance of 55.23%. GFI=. 979 and RMSR=.084 suggested a reasonably good fit. The indicators of closeness to unidimensionality had adequate values: UniCo=.978, ECV=.877 and MIREAL=.227, also indicating an essentially one-dimensional structure. In a second sample of 300 participants, a CFA with a single factor was proposed. Since the fit was not entirely satisfactory (χ2/df=6.93, CFI=.92), the parameters corresponding to the correlations between the errors of some items were released, according to the modification indices (item 3 with item 4; 6 with 10 and 16; 10 with 11; 14 with 15; 20 with 21 and 23). After these modifications, the fit reached adequate values (χ2/df=4.83, CFI=.95), with factorial weights ranging between .65 and .89 (Table 2). In the third subsample, in order to carry out a cross-validation, the last model fitted in the previous phase was replicated. The results showed a slight worsening of the fit, as expected, (χ2/df=5.13, CFI=.93), but the differences were small enough for the solution reached to be considered as stable. Taking into account the numerical results obtained, as well as the theoretical and substantive aspects derived from the field of study, the structure of the scale can be considered as essentially one-dimensional (Calderón, Navarro, Lorenzo-Seva, & Ferrando, 2019).
ReliabilityThe PCC-G-Staff showed excellent internal consistency (αordinal=.96; ωordinal=.96). In participants assessed at follow-up (n=176), the test-retest (r=.88, p<.001) correlation and the intra-class correlation (ICC=.93, p<.001) indicated excellent temporal stability.
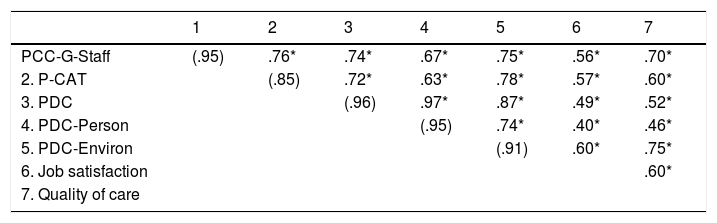
Validity evidence based on relationships with other variablesPearson correlations between the three questionnaires assessing person-centered care (i.e., PCC-G-Staff, P-CAT, PDC) are shown in Table 3. The results showed that all instruments converged in the expected direction. The total score of the PCC-G-Staff significantly correlated with both P-CAT and PDC and the percentage of associated variance between PCC-G-Staff and the two questionnaires was 58.83% and 55.20%, respectively. The associated variances in both PDC subscales were 49.97% for the person-centered subscale and 56.40% for the environmental subscale. PCC-G-Staff was also significantly correlated with job satisfaction and quality of care, with associated variances of 31.58% and 49.84%, respectively (see Table 3).
Pearson correlations between PCC-G-Staff, P-CAT, PDC, job satisfaction and quality of care.
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | |
|---|---|---|---|---|---|---|---|
| PCC-G-Staff | (.95) | .76* | .74* | .67* | .75* | .56* | .70* |
| 2. P-CAT | (.85) | .72* | .63* | .78* | .57* | .60* | |
| 3. PDC | (.96) | .97* | .87* | .49* | .52* | ||
| 4. PDC-Person | (.95) | .74* | .40* | .46* | |||
| 5. PDC-Environ | (.91) | .60* | .75* | ||||
| 6. Job satisfaction | .60* | ||||||
| 7. Quality of care |
Note. PCC-G-Staff: Person-Centered Care-Gerontology-Staff version; P-CAT: Person-Centered Care Assessment Tool; PDC: Person-directed Care; PDC-Person: Person-centered subscale of the PDC; PDC-Environ: Environmental subscale of the PDC. (Cronbach's α).
* p<.001.
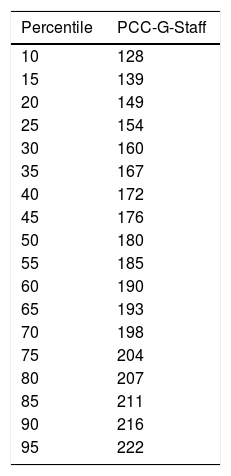
The ROC curve suggested that the PCC-G-Staff questionnaire is very good for discriminating staff who report person-centered care (see Figure 1), with an area under curve (AUC) of .88. The direct score maximizing the questionnaire sensitivity and specificity according to this AUC was 187 (sensitivity=90.4%, specificity=71.6%). Normative data in percentile ranks are shown in Table 4.
Item response theory analysisTo examine the precision of the PCC-G-Staff for different levels of the variable (θ), we estimated the information function. As shown in Figure 2, the highest precision is reached for values of θ between -2.5 and+1. The items’ parameter a (i.e., discrimination) are shown in Table 2.
DiscussionThe aging of the population has led to growing concern about the quality of services (Koren, 2010; Zubritsky et al., 2013), mainly in the area of quality and people's control over their own lives. The PCC approach is of recent interest due to its focus on the improvement of care by reinforcing the importance of considering the preferences, needs and personal identities of users, and following the WHO guidelines (World Health Organization WHO, 2015) advising against the delivery of homogeneous treatment to all users. So far, there has been a lack of instruments adapted to the Spanish context to assess the level of implementation of person-centered care provided by different services from the healthcare professionals’ viewpoints. The present study aimed to develop and validate the first Spanish instrument for the assessment of healthcare staff views on PCC.
The items making up the questionnaire cover all ten components in the PCC-gerontology model, with at least two items per component. The final instrument is easy to apply, and its psychometric performance is excellent. The internal structure is essentially unidimensional (Calderón et al., 2019; Villegas, González, Sánchez-García, Sánchez-Barba, & Galindo-Villardón, 2018), providing a total score for the level of implementation of the PCC approach from the staff point of view. Following the European model for test quality assessment (Muñiz & Fonseca-Pedrero, 2019) the reliability of the questionnaire is excellent if we look at both the internal consistency (α=.96, and ω=.96), and test-retest reliability (r=.88, and ICC=.93).
The PCC-G-Staff questionnaire also demonstrated validity evidence in relation to other variables assessing the same construct (r=.76 and r=.74 with P-CAT and PDC, respectively). In line with the aforementioned European model, these correlations represent excellent validity evidence criteria. Moreover, the questionnaire discriminates with considerable precision between the centers that follow the PCC-approach and those that do not, as shown by the area under the ROC (AUC=.88). Specifically, the total score maximizing the questionnaire sensitivity and specificity according to this AUC was 187 (Sensitivity=90.4%, Specificity=71.6%). The IRT models used also provided a reliability assessment with the staff score showing the highest precision for values of θ between -2.5 and+1.
It is worth noting that the PCC-G-Staff questionnaire included items specifically to assess PCC for individuals with advanced dementia for the first time. Also, and consistent with previous studies (Edvardsson, Sandman, & Borell, 2014; Røn et al., 2018; Zimmerman, Shier, & Saliba, 2014; Van de Pol-Grevelink, Jukema, & Smits, 2012), the level of implementation of the PCC approach as measured by the total score was highly associated with staff job satisfaction and the perceived quality of care provided by the center. This represents a key aspect of the PCC-approach, as it highlights the benefits of person-centered delivery not only to the elderly people being cared for but also to the staff in maintaining their motivation and quality of care, which may prevent mental health issues reported in caregivers (Jütten, Mark, & Sitskoorn, 2019).
The findings of this study should be interpreted in the context of its limitations. Despite using two of the most widely-used questionnaires to evaluate evidence of validity, to date there is no gold standard or external criteria against which to check the scores provided by the PCC-G-Staff questionnaire. We are currently working with several specialists in the PCC-gerontology model to overcome this issue. Also, there is no available data regarding users’ and relatives’ views to explore the convergence between assessments and views.
In summary, the first Spanish instrument is now available to assess the level of person-centered care provided by senior centers from the staff viewpoint with excellent reliability and validity. From a practical standpoint it represents a milestone for the implementation of the PCC-model in Spanish-speaking countries and it encourages research to include users’ and relatives’ views, as well as information provided by center supervisors to allow comprehensive assessment of the PCC-gerontology model (White et al., 2008; Edvardsson & Innes, 2010; Martínez, 2017, 2018).
FundingThis study was supported by the Ministry of Economy and Competitiveness [grant number PSI2017-85724-P]; a postdoctoral grant funded by the National Agency of Research of the Spanish Ministry of Science, Innovation and Universities [grant number BES-2015-073327]. The funding entities played no role in the study design, data collection, analysis or interpretation of the results.