The aim of the present study was to examine obsessive beliefs and intolerance of uncertainty differences among patients Obsessive compulsive disoreder (OCD), trichotillomania, excoriation, generalized anxiety disorder (GAD) and a control group healthy.
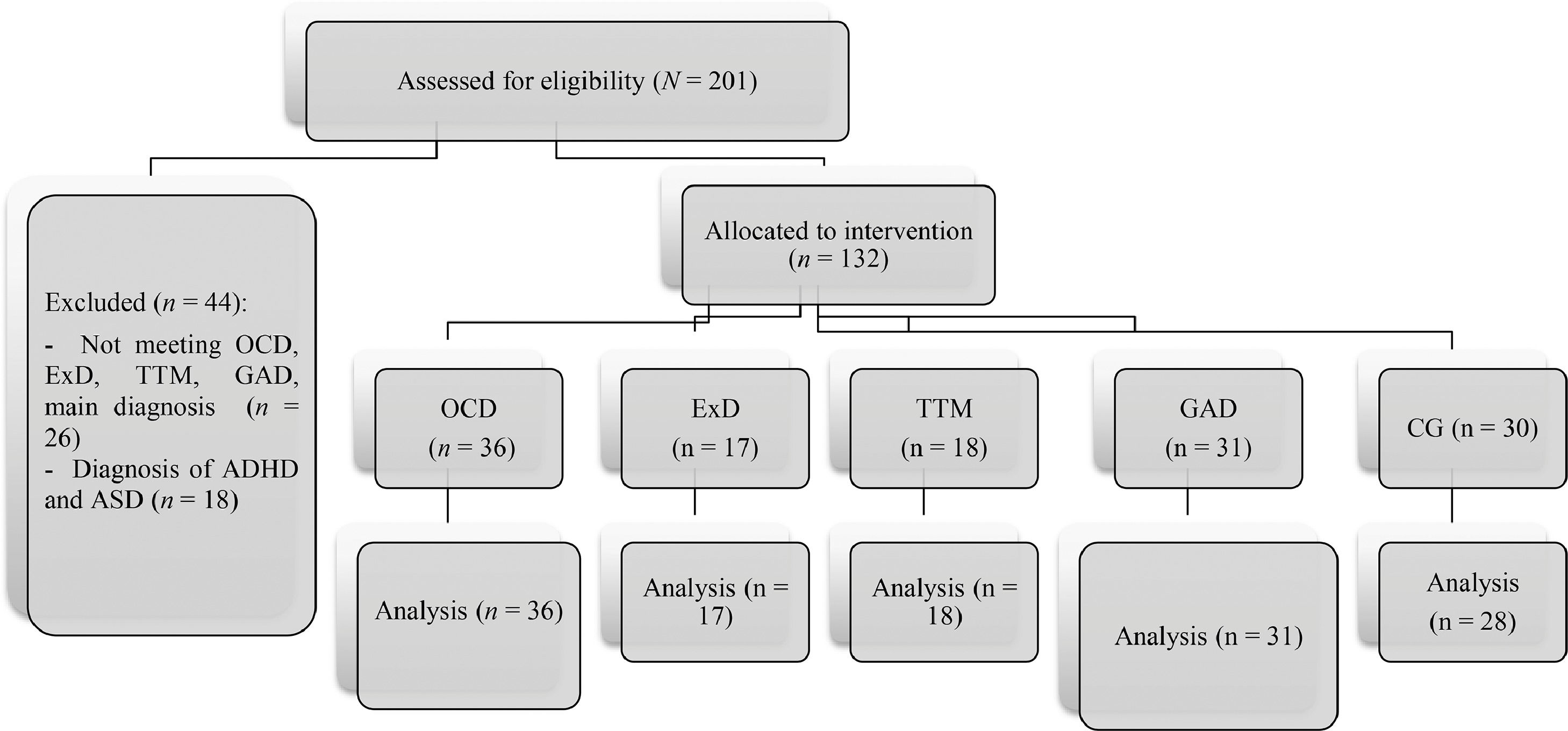
Method130 participants between the ages of 17 and 62 years (Mean = 29.56, SD = 11.81) diagnosed with OCD (n = 36), trichotillomania (n = 18), excoriation (n = 17), GAD (n = 31) and a healthy control group (n = 28) were evaluated by Obsessive Beliefs Spanish Inventory-Revised and Intolerance of Uncertainty Scale.
ResultsThe trichotillomania group presented one of the highest obsessive beliefs highlighting over-importance of thoughts, thought action fusion-moral, importance of controlling one's thoughts. The OCD group also had higher scores in inflated responsibility and thought action fusion-likelihood. The GAD group excelled in inhibitory and prospective uncertainty. The level of depression influenced obsessive beliefs while anxiety affected inhibitory and prospective uncertainty.
ConclusionsCognitive variables such as obsessive beliefs and Intolerance of Uncertainty should be considered in the prevention and intervention of obsessive and anxiety disorders.
Obsessive beliefs have been considered central to the onset and development of obsessive-compulsive disorder (OCD). The cognitive-behavioral model (Rachman, 1998; Salkovskis, 1985) postulates that clinical obsessions arise from maladaptive dysfunctional beliefs, such as overestimation of threat and responsibility, importance and need to control intrusive thoughts and perfectionism and intolerance of uncertainty. These beliefs lead to wrongly interpreting intrusive thoughts, causing anxiety-reducing behaviors and thus maintaining the problem. The Obsessive Compulsive Cognitions Working Group (OCCWG, 1997, 2003) identified six domains that confer vulnerability to the presence of clinical obsessions: inflated responsibility, overestimation of threat, perfectionism, intolerance of uncertainty, exaggerated importance of thoughts, and importance of controlling thoughts. Reuman et al. (2018) evaluated 92 people with OCD and indicated that obsessive beliefs remained significant predictors even after taking depressive symptoms into account and that cognitive fusion was a unique individual predictor of responsibility for damage and dimensions of unacceptable thoughts.
One of the main questions has been to analyze whether the central obsessive beliefs were specific to OCD or if they might be part of other disorders. Specifically, Tolin et al. (2006) compared OCD patients, anxiety disorder patients, and non-clinical controls, concluding that OCD presented higher means in threat estimation, uncertainty, perfectionism, and thought control. Controlling level of anxiety and depression, the belief of thought control was greatest in OCD patients. Olatunji et al. (2019) evaluated the symptoms and beliefs of OCD in this clinical group compared to other participants with anxiety and non-clinical disorders. They found that erroneous beliefs regarding one's own thoughts are at the core of OCD, which may provoke the use of compulsions to alleviate the anguish associated with such thoughts. Haseth et al. (2019) proposed that thoughts and beliefs about worry contributed to the development and maintenance of GAD.
As for disorders related to obsessions and compulsions, cognitive-behavioral models have suggested that some cognitions and beliefs are functionally related to trichotillomania (TTM). Several authors have identified different beliefs linked to hair pulling episodes such as negative beliefs about oneself and about control, low self-efficacy regarding coping skills and a tendency to perfectionism (Rehm et al., 2015, 2019).
Excoriation disorder (ED) has also been the subject of research. Houazene et al. (2021) identified that shame mediated the relationship between perfectionism and symptoms of body-centered behaviors, whereas self-criticism was not a significant mediator.
Within the group of obsessive beliefs, intolerance to uncertainty has been considered the main factor responsible for both basic anxiety and obsessive-compulsive symptoms (Citkowska-Kisielewska et al., 2019). According to Dugas et al. (2001), uncertainty intolerance is the excessive tendency to consider unacceptable the possible occurrence of future negative events, regardless of their likelihood. The OCCWG (1997) refers to this as the set of beliefs about the need for certainty, the ability to cope with unpredictable changes, and proper functioning in ambiguous situations.
Although intolerance to uncertainty has been classically related to GAD, there are studies that have confirmed the important role of this variable in OCD, concluding that it may be a central factor in both disorders (Holaway et al., 2006). Along these lines, Carleton (2016) identified uncertainty intolerance as a transdiagnosis risk factor for emotional disorders in general. Some research has attempted to relate this variable to other types of obsessive beliefs. Thus, Bragdon & Coles (2017) found a subgroup of individuals with OCD that obtained low scores in beliefs of inflated responsibility and overestimation of threat, while having high scores in beliefs reflecting perfectionism and uncertainty.
Various factors have been related to dysfunctional cognitions in patients, such as depressive symptoms or trait anxiety (Rosa-Alcázar et al., 2020; Tolin et al., 2006). Kertz et al. (2015) found that a reduction in repetitive negative thoughts was associated with an improvement in symptoms of anxiety and depression. The relationship between obsessive beliefs and severity of symptoms has also been pointed out, highlighting that symptomatic improvement is accompanied by more adaptive beliefs (Kyrios et al., 2015).
The transdiagnostic hypothesis has gained relevance in recent years, highlighting different phenomena such as repetitive negative thoughts (Wahl et al., 2019), intolerance to uncertainty (Gillett et al., 2018) and cognitive intrusions (Pascual-Vera & Belloch, 2018), and vulnerability factors can be considered in different disorders. Therefore, these variables could represent a more general correlation with those characterized by negative affect (Gentes & Ruscio, 2011) than with specific disorders.
The different data bring the need to research the role of dysfunctional beliefs in a group of anxiety and obsessive-compulsive spectrum disorders, as well as possible influencing factors. This would enable us to observe whether obsessive beliefs are domains affected differentially in the disorders studied, or are homogeneously affected, thus supporting the transdiagnostic hypothesis (Pascual-Vera et al., 2017).
The aim of the present study was: (1) To examine OB (obsessive beliefs) and IU (intolerance uncertainty) differences among patients (OCD, TTM, ED, GAD) and a healthy control group. (2) To analyze if OB and IU can be influenced by anxiety and depression. (3) To assess the relationship between sex and phamacological consumption and OB and IU among a clinical group, and (4) To study the relationship between OB and IU and severity symptoms in clinical groups.
MethodParticipantsThe study comprised 130 participants between the ages of 17 and 62 years (Mean = 29.56; SD = 11.81) diagnosed with OCD, GAD, ED and TTM and a healthy control group (CG).
Inclusion criteria were as follows: (i) diagnosis of OCD, TTM, ED and GAD (APA, 2013). (ii) OCD participants were required to obtain ≥ 16 scores in Y-BOCS (Goodman et al., 1989). (iii) GAD participants had to reach ≥ 56 in the Penn State Worry Questionnaire (PSWQ; Meyer et al., 1990). (iv) ED participants had to reach Milwaukee Inventory for the Dimensions of Adult Skin Picking scores ≥ 13 (MIDAS; Walther et al., 2009). (v) TTM participants had to reach ≥ 12 on the Massachusetts General Hospital Hair-pulling Scale (MGH-HS; Keuthen et al., 1995). Exclusion criteria included: (i) comorbidity with Schizophrenic Spectrum Disorders, Personality Disorders, Anorexia, Bulimia, substance abuse disorders and Neurocognitive Disorders, and (ii) being under 15 or over 65 years of age. Participants in the control group were excluded if: (i) they presented a current psychopathological disorder, (ii) had experienced or been diagnosed with any of the aforementioned disorders at some point in their life.
Sample characteristics are presented in Table 1.
Sample measures.
n = number; SD: Standard deviation; OCD: Obsessive-compulsive disorder; ED: Excoriation; TTM: Trichotillomania: GAD: Generalized anxiety disorder; CG: Control group; BAI: Beck Anxiety Inventory; BDI: Beck-II Depression Inventory.
The study meets the ethical standards of the Declaration of Helsinki and has been approved by the Ethics Committee of the University of Murcia, Spain (code: 1296/2016; code: 2123/2018). All families provided written informed consent after which participants engaged in an individual diagnostic interview based on the DSM-5, conducted by three clinical psychologists. The test presentation order was the same for all participants. Two patients in the control group withdrew as they did not wish to continue being assessed. Recruitment is shown in Fig. 1
Clinical measures- -
Yale Brown Obsessive Compulsive Scale (Y-BOCS; Goodman et al., 1989) is comprised of 10 items assessing the severity of OCD. It contains two subscales, obsessions (range = 0–20) and compulsions (range = 0-20) and a total score (range = 0–40). The scale has a high internal consistency (α = .87–.90) and good convergent validity (r = .47–74). Cronbach's alpha in this study was .87.
- -
Penn State Worry Questionnaire (PSWQ; Meyer et al., 1990). A 16-item self-report scale that assesses the general tendency to worry especially present in GAD. The cut-off point for detection of GAD is 56. It has been shown to have good psychometric properties. Cronbach's alpha was high (α = .96).
- -
Milwaukee Inventory for the Dimensions of Adult Skin Picking (MIDAS; Walther et al., 2009) is a 12-item self-report questionnaire assessing the extent to which individuals report “focused” (six items) and “automatic” (six items) styles of skin picking. Each item is rated on a Likert-type scale from 1 to 5. Cronbach's alpha was: focused = 0.70, automatic = 0.71, and total = 0.75.
- -
The Massachusetts General Hospital Hair-pulling Scale (MGH-HS; Keuthen et al., 1995) is a seven-item self-report measure of TTM severity. Items are ranked on a 5-point Likert scale resulting in total scores ranging from 0 to 28. Higher scores indicate greater TTM severity. Internal consistency was α = .94.
- -
Beck-II Depression Inventory (BDI; Beck et al., 2011) is a 21-item self-report scale that assesses depression severity. Classification of scores was as follows: minimal (0 to 13), mild (14 to 19), moderate (20 to 28) and severe (>29). Cronbach's alpha was .91.
- -
Beck Anxiety Inventory (BAI; Beck & Steer, 1996) is a 21-item self-report scale that measures anxiety severity. Classification of scores was as follows: minimal (0 to 7), mild (8 to 15), moderate (16 to 25) and severe (26+). The internal consistency coefficients varied between .85 and .93. Cronbach's alpha was .92.
- -
Obsessive Beliefs Spanish Inventory-Revised (OBSI-R; Belloch et al., 2010) is a 50-item self-report questionnaire (from 1, strongly disagree, to 7, strongly agree) with eight scales: Inflated responsibility, over-importance of thoughts, thought action fusion-likelihood, thought action fusion-moral, importance of controlling one's thoughts, overestimation of threat, intolerance of uncertainty, and perfectionism. This has been shown to have adequate psychometric properties. Cronbach's alpha was 0.92.
- -
Intolerance of Uncertainty Scale (IUS; Freeston et al., 1994). Comprising 27 items with five types of response which evaluates the tendency to react negatively on an emotional, cognitive and behavioral level to uncertain situations and events. It is divided into two factors: Inhibitory uncertainty and prospective uncertainty. The internal consistency coefficient was .91 and test-retest reliability .78. Cronbach's alpha in this study was 94.
Chi-square and one-factor ANOVA were used to examine potential group differences in clinical and demographic (age/gender) variables at pretreatment. Subsequently, ANOVA and post-hoc comparisons (Tukey or Games-Howel) of OBSI-R and IUS were carried out. An analysis of covariance was performed when there were significant differences between clinical groups in anxiety and depression. Independent samples Tests (Kruskal Wallis H test) were performed within each clinical group taking into account the sex and medication use. The Pearson correlation was used to analyze the relationship between variables. All participants were included in analyzes. SPSS Statistic 22.00 was used for statistical analysis.
ResultsEquivalence of groups in pretestThe groups were not equivalent in any sociodemographic or clinical variable. See Table 1
A comparison of clinical group and CG in OB and IUTable 2 shows the results of ANOVA on all variables, except in OBSI-R-P.
ANOVA and post-hoc analysis.
OCD: Obsessive-compulsive disorder; ED: Excoriation; TTM: Trichotillomania; GAD: Generalized anxiety disorder; CG: Control group, OBSI-R-IR: Inflated responsibility, OBSI-R-IT: over-importance of thoughts, OBSI-R-TAF: thought action fusion-likelihood, OBSI-R-TAFM: thought action fusion-moral, OBSI-R-CT: importance of controlling one's thoughts, OBSI-R- OT: overestimation of threat, OBSI-R-IU: intolerance of uncertainty, OBSI-R-P: perfectionism, Inhibitory IUS: Inhibitory Intolerance of Uncertainty, Prospective IUS: Prospective Intolerance of Uncertainty. *** < .001; **< .01; *< .05.
The TTM group reported one of the highest obsessive beliefs, highlighting OBSI-R-IT, OBSI-R-TAFM, OBSI-R-CT and OBSI-R-OT. OCD group also presented higher scores in OBSI-R-IR and OBSI-R-TAF. GAD group excelled in Inhibitory and prospective IUS (Table 3).
ANCOVA controlling depression and anxiety.
OCD: Obsessive-compulsive disorder; ED: Excoriation; TTM: Trichotillomania; GAD: Generalized anxiety disorder; CG: Control group, OBSI-R-IR: Inflated responsibility, OBSI-R-IT: over-importance of thoughts, OBSI-R-TAF: thought action fusion-likelihood, OBSI-R-TAFM: thought action fusion-moral, OBSI-R-CT: importance of controlling one's thoughts, OBSI-R- OT: overestimation of threat, OBSI-R-IU: intolerance of uncertainty, OBSI-R-P: perfectionism, Inhibitory IUS: Inhibitory Intolerance of Uncertainty, Prospective IUS: Prospective Intolerance of Uncertainty. *** < .001; **< .01; *< .05.
Correlation between sociodemographic variables, anxiety and depression with OB and IU was corried out. In addition, we carried out a comparison of independent means with the gender variable. Results indicated that only the anxiety and depression variables correlated with OB and IU. These variables (anxiety and depression) obtained statistically significant differences among groups, an analysis of covariance was carried out. BDI influenced all OBs except OBSI-R-OT and inhibitory and prospective IUS. BAI influenced OBSI-R-CT, OBSI-R-OT and inhibitory and prospective IU. Once these variables were controlled, the TTM group mean was increased in OB and UIS; OCD and GAD group decreased in all variables, and ED group increased in OB and decreased in inhibitory and prospective IUS.
Intragroup comparisons based on sex and use of pharmacotherapyThe OCD group did not present significant differences in sex (p > .05). Pharmacotherapy type influenced in the OBSI-R-IT (p = .050) and OBSI-R-TAFM (p = .021). Patients who were taking antipsychotics+ antidepressives presented the worst scores. ED participants not taking medication achieved lower scores in OB and IU (p < .001). The women in the GAD group achieved higher scores in OBSI-R-IR (p = .001). OBSI-R- OT (p = .001), inhibitory (p < .001) and prospective IUS (p = .002). Men achieved higher scores in OBSI-R-IT (p = .037).
Correlation between OB and IU and severity symptom in clinical groupsThe OCD group presented significant relationships between scores in compulsions YBOCS and OBSI-R-IR (r = .32, p = .041), OBSI-R-IT (r = .34, p = .041). OBSI-R-TAF (r = .392, p = .018). OBSI-R-CT (r = .40, p = .015) and OBSI-R- OT (r = .35, p = .034). Obsessions Y-BOCS was related to OBSI-R-CT (r = .36, p = .031). The ED group presented a relationship between MIDAS automatic scratching and OC (r = .81 to 61, p > .01). TTM group presented a significant relationship between MGH-HS and all OB and IU (r = .56 to .81, p < .01), except in OBSI-R-IR and OBSI-R-TAFM.
GAD group presented a relationship between PSWQ and Inhibitory IUS (r = .62, p = .001) and prospective IUS (r = .63, p = .001).
DiscussionOur main aim was to analyze differences in OB and UI between participants from different clinical groups and healthy CG. Our results indicate the presence of more OB and IUS in all clinical groups, coinciding with previous studies (Olatunji et al., 2019; Rizvi et al., 2020). According to Romero-Sanchiz et al. (2017), the difference between clinical patients and healthy subjects would lie not so much in the presence but in how the former process the underlying thoughts and beliefs.
TTM and OCD achieved highest scores in OB while the GAD and OCD groups stood out in UI. The relevant role that cognitions seem to play in the phenomenology of TTM was reported by Rehm et al. (2015, 2019), and as in our case highlighted negative beliefs about controlling one´s, over-importance of thoughts, moral thought-action fusion, importance of controlling one's thoughts and overestimation of threat. The OCD group scored higher in inflated responsibility and likelihood thought-action fusion-. This finding agrees with Reuman et al. (2018) about the fact that experiencing likelihood thought-action fusion could influence the increase of inflated responsibility thinking, leading to the belief that it can cause harm to others unless certain preventive measures are taken. The ED group presented the highest results in UI (OBSI-R) and perfectionism, considering error to be something as very negative which partly coincides with Houazene et al. (2021).
Regarding uncertainty, the GAD and OCD groups found higher scores, with no significant differences between groups. UI deficits in anxiety disorders have been widely reported, specifically in GAD (Counsell et al., 2017). However, it has also been shown to be relevant in other disorders, such as OCD (Fradkin et al., 2020; Williams & Levinson, 2021). This has been related to the control behaviors of the disorder, such as compulsive rituals, which might respond to the demand to alleviate anxiety related to uncertainty (Inozu et al., 2021). Nevertheless, we must stress that uncertainty was measured with two different instruments: OBSI-R-IU and IUS. The first focuses on beliefs and the second on paralyze action (inhibition) and uncertainty that generate great discomfort and bewilderment (prospective), closer to the concern of generalized anxiety. Therefore, the results in groups are different.
Focusing on comparisons between clinical groups, differences between TTM and OCD were observed only in over-importance of thoughts, being higher in the first group, while in inhibitory and prospective IUS, the OCD group reached higher averages. Differences between the TTM and GAD groups were seen in over-importance of thoughts, thought action, moral-fusion and importance of controlling one's thoughts, being greater in the TTM group, while the GAD group stood out in inhibitory and prospective IUS. The ED group presented significantly lower scores in inhibitory and prospective IUS compared to the OCD and GAD groups. These data could indicate that the TTM group has highest obsessive beliefs, followed by the OCD group. Furthermore, the GAD and OCD group presented higher UIS (inhibition and prospective) in comparison to the other two clinical groups. Therefore, we could indicate that the GAD and OCD groups are close in terms of uncertainty variables, while the TTM and OCD groups would be close in as regards OB. As indicated by Besharat et al. (2019) OB and IUS could be deemed possible transdiagnostic factors, though with specific variabilities in each disorder.
The second aim was to analyze whether differences between clinical groups varied when controlling for anxiety and depression. After controlling for anxiety and depressive symptoms, the TTM and OCD groups presented higher obsessive beliefs. The influence of anxiety and depression has also been reported in different studies (Capobianco et al., 2020). Following Purdon (1999) it may be that patients with obsessive spectrum disorders are more likely to repress thoughts, due to the egodystonic nature of obsessions. This would contribute to an increase of obsessive beliefs, compared to cognitive processes such as worries and negative automatic thoughts more typical of anxiety disorders.
After controlling for anxiety, the groups with the greatest uncertainty were GAD and OCD, therefore both groups who consider uncertainty intolerable and that worry helps to cope with it (Aktar et al., 2017). This leads us to conclude, following Tümkaya et al. (2018), that anxiety and depression appear to play a relevant role in OB and IUS. These variables could be transversal in the investigation of cognitive processes in these disorders.
The third aim analyzed the influence of sex and use of psychotropic drugs on obsessive beliefs and uncertainty.
We only found significant differences in the GAD group regarding sex, with women having higher scores in inflated responsibility and overestimation of threat and inhibitory and prospective IUS, while men scored higher in over-importance of thoughts. We consider these differences might be due to social and cultural factors, rather than differences of the sex itself (Hofmann et al., 2010).
A positive relationship was also found between the consumption of psychotropic drugs (antipsychotic vs antidepressant) and OB (OBSI-R-IT and OBSI-R-TAFM) in the OCD group. This could be explained by the possible greater severity of the disorder in patients taking antipsychotic drugs. These results may be in line with those by Park et al. (2020) on the predictive capacity of worry beliefs in response to psychopharmacological treatment in OCD.
The final aim was to check for a relationship between OB and UI and the severity of the disorder. In our study, it was found that in obsessive groups, the greater the severity of the disorder, the greater the presence of obsessive beliefs. In the GAD group, the positive relationship was between severity and uncertainty, coinciding with other authors (Rehm et al., 2019; Toffolo et al., 2016). These results could strengthen the thought that obsessive beliefs play an important role in maintenance and evolution of these psychopathological conditions.
As clinical implications, we can highlight that cognitive variables such as OB and UI should be considered not only in the intervention of obsessive and anxiety disorders, but even in their prevention. This is in line with some studies on the importance of dysfunctional beliefs and uncertainty in the development, maintenance and treatment of psychopathology (Shihata et al., 2016). In addition, levels of anxiety and depression have proven to be relevant factors to take into account, therefore it would be convenient to carry out adequate assessment and treatment of these variables to improve the psychological intervention of cognitive processes which patients present.
This study has some limitations, such as non-random selection of participants, small sample size, use of only self-reports for evaluation of key variables and evaluation in a single time point.
Future studies could include a larger sample size in order to generalize results and analyze these according to different subtypes of obsessions and compulsions. In addition, longitudinal research would help to observe how interventions focused on the cognitive field can improve the psychopathology of patients and its maintenance over time.
Despite these limitations, to our knowledge, this is the first study to compare OB and UI in four clinical samples (OCD, TTM, ED and GAD), clarifying some of the most important differences and indicating the possibility that it is transdiagnostic variables that could influence the vulnerability and maintenance of these disorders.
FundingThis article was supported by the Ministerio de Economía and Competitividad of the Spanish Government (Projects No.PSI2016-78185-P) and Project 20902/PI /18 financed by the Autonomous Community of Murcia (Spain) through the Grants for projects for the development of scientific and technical research by competitive groups, included in the Regional Program for the Promotion of Scientific and Technical Research (Action Plan 2018) of the Seneca Foundation-Science and Technology Agency of Murcia Region (Spain).
We thank Professor Amparo Belloch and her team for allowing us to have their OBSI assessment instrument.