The approach to Acute Coronary Syndrome from a gender perspective is relatively recent. Research is extensive at epidemiological and clinical levels. However, available evidence, besides neglecting the social dimensions of the disease, has made women invisible. The objective of this review was to analyze the inequalities and gender biases in Acute Coronary Syndrome, from the beginning of the disease process to the final resolution.
MethodsAn exhaustive review of the literature of the entire health care process, from risk factors to rehabilitation and recovery, was carried out. The search for articles on gender, gender inequalities, or gender bias was conducted in indexed journals of social and health sciences. Also, a specific search was performed for each stage of the process, such as risk factors, prehospital phase, diagnosis, treatment, and rehabilitation.
ResultsResults showed the presence of gender biases throughout the entire health care process in Acute Coronary Syndrome. It is shown gender inequalities in the access to medical care, including a poor recognition among women themselves as well as among health professionals; longer prehospital delays; inadequate diagnoses and treatments; or less assistance to cardiac rehabilitation programmes. These biases occurred at the different levels of the health services involved. Finally, this review included recommendations proposed or arising from the revised papers.
ConclusionsReducing gender biases in Acute Coronary Syndrome implies developing strategies to raise awareness among women, improve training of professionals serving at the different levels of health services, reduce delays, develop health management measures, and promote a research agenda.
El abordaje del síndrome coronario agudo desde una perspectiva de género es relativamente reciente. La investigación es extensa a nivel epidemiológico y clínico. Sin embargo, la evidencia disponible, además de descuidar las dimensiones sociales de la enfermedad, ha hecho que las mujeres sean invisibles. El objetivo de esta revisión es analizar las desigualdades y sesgos de género en el síndrome coronario agudo, desde el inicio del proceso de la enfermedad hasta la resolución final.
MétodosSe realizó una revisión exhaustiva de la literatura de todo el proceso asistencial, desde los factores de riesgo hasta la rehabilitación y recuperación. La búsqueda de artículos sobre género, desigualdades de género o sesgos de género se realizó en revistas indexadas del ámbito social y de la salud. Asimismo, se realizó una búsqueda específica para cada etapa del proceso, como factores de riesgo, fase prehospitalaria, diagnóstico, tratamiento y rehabilitación.
ResultadosLos resultados muestran la presencia de sesgos de género a lo largo de todo el proceso asistencial en el síndrome coronario agudo. Muestran desigualdades de género en el acceso a la atención médica, incluido un escaso reconocimiento entre las propias mujeres y entre los profesionales de la salud, retrasos prehospitalarios más prolongados, diagnósticos y tratamientos inadecuados o menos asistencia a los programas de rehabilitación cardíaca. Estos sesgos ocurren en los diferentes niveles de los servicios de salud involucrados. Finalmente, esta revisión incluye recomendaciones propuestas o derivadas de los documentos revisados.
ConclusionesReducir los sesgos de género en el síndrome coronario agudo implica desarrollar estrategias para sensibilizar a las mujeres, mejorar la formación de los profesionales que atienden los diferentes niveles de los servicios de salud, reducir las demoras, desarrollar medidas de gestión en salud y promover una agenda de investigación.
Cardiovascular disease (CVD) remains the leading cause of morbidity and mortality for both women and men.1 Acute Coronary Syndrome (ACS) is the main form of CVD, accounting for 19% of all deaths among men, and 20% among women, each year. In total, 1.7 million deaths in Europe are due to ACS. ACS is the leading cause of death in 44 countries among men and in 30 countries among women, among the 50 countries of Europe.2 It is the leading cause of death in women worldwide, yet, for many years, women have been underdiagnosed and undertreated.3 From the first classic description, it was interpreted that angina pectoris was a disease of man. When it was described more than 200 years ago, the diagnosed cases were basically men, which was logical, given the average life expectancy of the time and the delay of the onset of coronary disease in women, which is now well known.4,5 What is striking is that given current knowledge, it has not yet been able to dismantle and eradicate this historical bias.
Bernadine Healy, former director of the National Institutes of Health of the USA, called this phenomenon as Yentl syndrome,6 meaning that it is not recognized that women are having an ACS, unless they present a typically male pattern of pain and chest symptoms.7 On the other hand, although there has been a decrease in deaths from ACS in both men and women, since 2000 the rates are decreasing more in men than in women.3 In addition, recent studies have shown a higher level of early mortality among women.3,8–10 A comprehensive review of evidence on the presentation, pathophysiology, treatment, and outcomes of women with Acute Myocardial Infarction (AMI),3 pointed to the multifactorial explanation about the excess mortality in female patients on the basis of: research is incomplete, with women making up only about 20% of patients enrolled in clinical trials that might help to close knowledge gaps; women are under-treated with guideline-based recommended treatments; and women's adherence to evidence-based recommendations is sub-optimal.
ACS severity and prevalence in women are underestimated because of specific gender biases,11 a systematically erroneous approach dependent on the social construction of gender, which incorrectly considers women and men as similar and/or different. In a systematic review about the presence of gender bias in healthcare professionals’ attitudes, diagnoses, and treatment decisions,12 a positive and significant association was found between the level of implicit bias and the lower quality of care, taking into account professionals varying degrees of implicit gender bias.11
Treatments that are applied in these pathologies are influenced by traditional clinical studies, made with samples of male subjects, and based on the incorrect assumption that the results of these studies can be applied to both sexes indistinctly, ignoring the biological differences between men and women. Historically considered a ‘man's disease’, the basic research and clinical trial evidence that underpins treatment of CVD is largely based on males.13,14 Biological differences between sexes have also been used to maintain social inequality, e.g., looking for psychosomatic components in women's complaints but not in men's.15
As reflected in the available literature, the gender bias in ACS refers to the attribution of the same risk factors, symptoms or clinical presentation to women and men, use of different therapeutic approaches, greater difficulty in diagnosis, lower percentage of pharmacological treatment, or the delay of interventions and treatment among women with respect to men.16,17 In addition, women have ACS at later ages, and with greater comorbidities, all of which can hinder access to certain treatments, due to their risks. Also, women consistently present a higher burden of symptoms and comorbidities as compared with men and experience worse outcomes, more frequent hospitalizations, and a worse prognosis compared to men.1 Moreover, there are also gender differences in classic risk factors.18 This is in part due to biological variations in pathophysiology between the two sexes, and in part related to inadequate understanding of these differences, subconscious referral bias, and suboptimal application of existing women-specific guidelines.19
Another dimension of gender bias is the “universalisation” of the concepts of “woman” and “man”, when actually we are referring to a white, heterosexual, middle-class, Western woman and her male counterpart. Actually, race and gender disparities have been proved to persist when approaching assistance for heart affections.20,21
Although clearly harmful to women, gender bias in ACS treatment can also have a negative impact on men. Stereotyping “masculinity” as positive, favourable or healthy, and assuming that men are in a better situation is another bias that should be considered. Thinking of masculinity as universal also leads to problems understanding men's vulnerability.22,23
These manifestations of gender inequalities in health are considered to be systematic, unnecessary, avoidable and unfair, and specific to different political, economic and social contexts.24,25
At a theoretical level, gender inequalities “stem from sociocultural and historical constructs that translate sexual differences into discrimination, expressed in the division of labour by sex and in differential and hierarchical access to material and symbolic resources and to power in all its manifestations”.26
Linked to gender inequalities, gender stereotyping represents the process by which people make assumptions about others’ characteristics based on their gender, along specific trait dimensions,27 like the traditional consideration of men being physically and mentally stronger or more likely to take risks or women perceived to be more emotional and focused on caring for others than men.28 In addition, political, cultural, and economic differences also influence within countries.
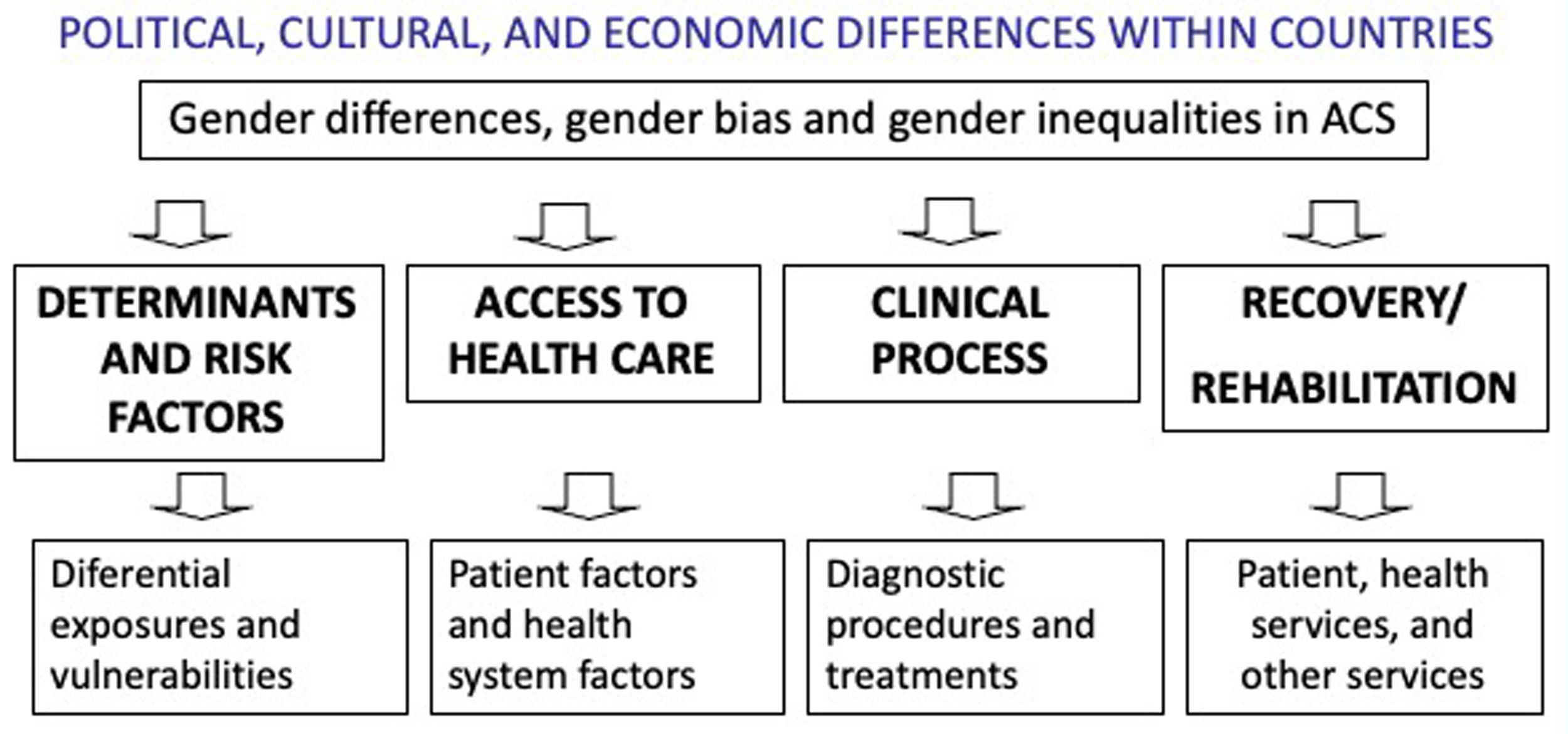
Given the need to address the ACS with a gender perspective, the objective of this article was to review the current evidence on the differences, inequalities and gender biases related to ACS in women. The social determinants and risk factors of the syndrome has been also examined, as well as the process that goes from the onset of symptoms (prehospital phase) to diagnosis and treatment (hospital phase), and to recovery and rehabilitation.
MethodsThe methodological approach has been based on a narrative review of the last 10 years of the literature available in the main repositories of scientific literature in the social and health fields. In September 2018, a search was carried out with a strategy designed for MEDLINE (Ovid), Science Direct, ProQuest, Embase, Scopus and Web of Knowledge databases. In addition, selected sources of grey literature were searched.
To execute the review, the following terms were used:
- •
To identify gender inequalities: “gender”, “women”, “gender inequality”, “gender bias”.
- •
To identify inequalities in the risk factors, treatment, diagnosis and rehabilitation: “risk factor”, “clinical decision”, “treatment”, “diagnosis”, “management”, and “rehabilitation”.
- •
To identify ACS: “Cardiovascular disease”, “CVD”, “ACS”.
The combination of the previous terms gave rise to the following searches:
- •
(“gender”) OR (“gender inequality”) OR (“gender bias”) OR (“women”)) AND (“cardiovascular disease”) OR (“cardiovascular risk factor”))
- •
“Gender bias” and “clinical decision” and “cardiovascular disease” or “acute coronary syndrome”
- •
((“Gender bias”) AND ((“cardiovascular diagnosis”) or (“cardiovascular treatment”) OR (“management of CVD”)
A summary of the methodology it is illustrated in Fig. 1.
The search of the databases identified 7152 documents. These documents were screened independently by three authors and in three steps. Firstly, based on the title and/or abstract, we select those articles that meet the following inclusion criteria: (a) only full-length articles published in English or Spanish languages were included in this review; (b) articles that reported “gender biases” in risk factors, symptoms, diagnosis, treatments, rehabilitation programmes or any other aspects of health care; and (c) articles or reviews that included proposals and recommendations to reduce gender biases.
We excluded case reports, news, book chapters, conference proceedings, and editorial letters. Secondly, based on a reading of the abstract, those articles relevant to the objective of the work were selected (gender inequality, gender bias, etc.). Finally, articles were examined according to the inclusion criteria, by carefully reading the full texts. Discrepancies were solved by discussion among authors.
No patient and public involvement: This research was done without patient involvement. Patients were not invited to comment on the study design and were not consulted to develop patient relevant outcomes or interpret the results. Patients were not invited to contribute to the writing or editing of this document for readability or accuracy.
Results and discussionRisk factors from a gender perspectiveTraditionally, the enrollment of women in experimental studies has been minimal, resulting in a lack of gender-specific analysis of clinical trials data and, therefore, the absence of specific risk factors assessment among women.29 Since the first studies on ACS, the factors classically considered are age, cholesterol, diabetes, hypertension, smoking, heredity, stress, obesity, and heart rate.30 The model of hegemonic masculinity and other types of masculinity and personality profiles have also been considered risk factors associated with working conditions and with specific exposures.31 based on the assumption that unhealthy behaviours tend to be more socially acceptable in men than in women.32
Scientific progress in the past decade has identified that these “traditional” cardiac risk factors play an important role in the development and progression of ACS in both men and women. However, there are important sex differences in some of these factors.33 In particular, it has been documented that diabetes and smoking increase the risk of CVD more in women than in men and that hypertension,13 which occurs more frequently in men before 50 years and in women after 50, leads to more strokes and heart failure in women than in men.34,35 Additionally, there are also gender differences in classic risk factors, so that cardiovascular diseases develop on average 7–10 years later in women than in men.18
In addition, a spectrum of risk factors that may be specific to women have been identified, such as menopause, hypertension of pregnancy, depression and stress, or autoimmune and rheumatic diseases.29,36 Other risk factors also include a higher severity of diabetes in women, phosphorus levels, vitamin D and C-reactive protein, hormonal contraceptives and hormone replacement therapy during menopause.37 Recently, different studies show the different effects of hostile and benevolent sexism for women's cardiovascular responses that indicate an increased risk of disease.38,39
Despite the evidence on how unhealthy behaviours contribute to increasing the risk of ACS, they do not fully explain that increase, and there are relevant results on how cardiovascular risk factors should be addressed differently for men and women.40 In recent years, researchers have questioned the lack of evidence and invisibility of women in epidemiological and clinical research.41 According to the American Heart Association guidelines for CVD prevention in women,42 the risk factors to take into account in order to maintain ideal cardiovascular health in women are cholesterol levels, blood pressure, fasting blood glucose, body mass index, cigarette smoking, physical activity and diet.
Today, there is a clear consensus that social and cultural factors have a major influence on health and wellbeing. Over the last few years there has been more research analysing the characteristics of the places where people live, neighbourhoods and their impact on behavioural, psychosocial and biological factors associated with ACS. Positive associations have been found between a neighborhood's socio-economic status and the incidence of heart disease, as well as with physical exercise, obesity and other risk factors.43 The socio-economic status negatively affects ACS risk, and this concerns more women than men.44,45 Young women also have greater prevalence of depression, anxiety, and stress, with higher depression and stress scores at the time of ACS presentation compared with men, as a function of greater comorbidities, family conflict, financial concerns, and caregiving demands.3,46
Some studies also have shown that women put their family needs above their own health needs, so that lack of time and family obligations are major “barriers” to the development of healthy behaviours.47 A study conducted to determine the level of awareness of American women about CVD and its importance found barriers to prevention and difficulties in adopting healthy behaviours among women themselves.48
These difficulties were mainly family responsibilities as caregivers (51%), confusion about what to do (42%), the belief that God or another higher power determines their health (37%), and not having money or health insurance (32%). In a study that used more typical approaches to ethno-epidemiological and mental health research, the construction of coronary vulnerability and the specific fragility of men and women of high and low socioeconomic status were analyzed.49 Although it was traditionally thought that stress was limited to the work and public environment historically occupied by men (male public sphere versus private female sphere), a broader examination of stress as the cause of the ACS was made, considering gender ideals, power relations at work, at home and in interpersonal relationships, and difficulties in connecting different spheres of life, and incorporated subjectivity into the process of health care and illness.49 For example, a specific vulnerability factor for working-class women is the “superwoman syndrome”, they must be all-powerful, and that is a specific stressor for them. European Guidelines include low socio-economic status, lack of social support, stress at work and in family life, depression, anxiety, hostility and the Type D personality as elements that contribute both to the risk of developing ACS and the worsening of the clinical course and prognosis, and include a questionnaire with key questions for evaluating psychosocial risk factors in clinical practice.50 The 2016 actualization of the Guidelines also includes the importance of interventions on environmental health (workplace, school, etc.) and give specific recommendation to women and men.51 The inclusion of elements like socio-economic status or gender roles is indicative of a new awareness amongst the professional and scientific community.
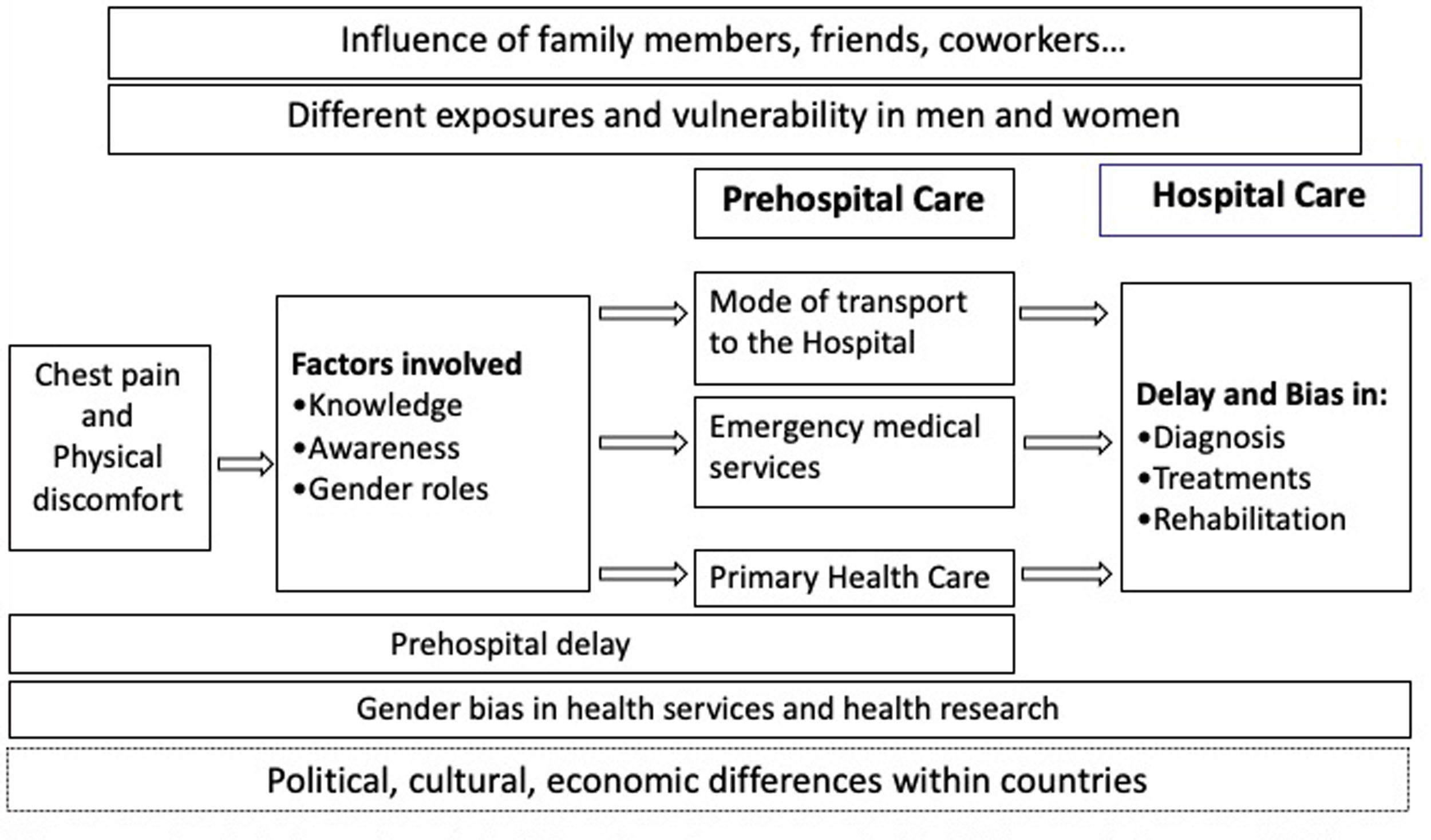
Gender bias and inequalities in health services and health researchFirst, differences in the symptoms of ACS and inequalities in the delay in obtaining health care are presented for the prehospital phase. Then, the gender bias in the diagnosis, treatment and post-coronary recovery is considered.
Inequalities in prehospital delayFig. 2 represents the itinerary of patients from the onset of ACS symptoms up to hospital care. It includes main factors that influence the decision process and determine prehospital delay, and health care, highlighting gender biases during the process.
One of the most analyzed aspects of access to medical care for patients with ACS is what is known as prehospital delay. Prehospital delay is the time interval between the onset of symptoms indicative of ACS and arrival at the hospital.52 In ACS patients, early access to treatment is key to survival. Clinical efficacy of treatment and survival are very closely linked to the time period between the onset of symptoms and receiving treatment. Minimizing the time that passes before diagnosis and treatment is therefore a priority.53
Research into the gender-specific factors associated to delays in ACS is more recent. The studies carried out have generally found that the delay is longer than desired in both men and women. However, one of the most studied aspects more recently is the longer delay in women seeking help. It has been argued that “non-specific” or “atypical” symptoms are the reason why women fail to recognize the disease. But, it has also been found that even when they experience “typical” symptoms, many women may ignore them or not recognize them, as women underestimate their risk of ACS.42
Some studies have found that this longer delay in women is due to older age. A link between gender and age has also been found, so the differences between the delays in men and women are greater in older men and women than in younger men and women, especially in 65–75-year-olds.54,55
After a 2004 meta-synthesis on the factors that reduce or increase delay in seeking treatment, a recent review has found that women delayed longer in 24 of 44 studies analyzed, while 14 studies found no differences between women and men.56,57 Among the factors reported that increase the delay, were: women contacted their GP more, were more likely to be widowed and living alone, and tended to manage their illness by themselves. Furthermore, it has been also observed that differences between expected symptoms and actual symptoms were also associated with a longer delay.58
Although it appears that pre-hospital delays are longer in women than in men, both men and women delay before seeking medical help. In a review of the literature on ACS in men, it was found that discourses associated with hegemonic masculinity, and stoicism, endurance and self-control, were factors associated with longer delays in men. Some men considered health to be a “female domain”, stating that women (usually their wives) asked for help, while they delayed; or, that they were only persuaded to act for their wives or partners, although these discourses were not shared by all the men in the study. In some cases, it was clear that men did not feel personally at risk of the disease because they did not see themselves as a “coronary candidate”. In other cases, they did not recognize the symptoms because they were not “classic” or “typical”, while some men who had previously suffered an ACS believed they were “protected” by medication or their new healthier “lifestyle” (e.g., exercising or quitting smoking).59
Additional to gender-related aspects, other factors associated with the health system itself must also be taken into account when considering gender inequalities in these delays. A study in the United States found that women who used emergency medical services were more likely than men to experience a delay between the time the call was made and the arrival at the hospital.60 These results indicate that a longer prehospital delay in women may be due in part to the health system and not to the women themselves. Further research is needed on this part of the process, since many different factors could influence the results of emergency services during response time, on-scene time and transport time.61,62
Researchers interest in the mode of transport used by ACS patients is caused by the fact that the main objective of out-of-hospital emergency services (when they exist) is to provide medical care, through rapid diagnosis and treatment, in all emergency situations. At the onset of symptoms indicative of ACS, patients are advised to use emergency medical services that can be contacted by telephone, and the use of private vehicles is not recommended. Although patients can get to the hospital more quickly if they use their own vehicle, when emergency services perform the transport, access to an adequate diagnosis and treatment is faster, so its use is recommended.58 Anyway, these recommendations have been the subject of debate, because of difficulties in measuring the different time periods and the complexity of the factors involved in each situation.
The studies carried out have shown that people generally travel to the hospital in their own vehicles, in taxis or in another type of public transport. Awareness of the importance of quickly seeking medical care and calling for an ambulance is also more frequent in patients who have recognized that their symptoms are of cardiac origin.57 Furthermore, when symptoms first appear, women are more likely to seek out relatives and medical care other than that available in the hospital emergency department, while men are more likely to use the emergency services and go directly to the hospital.63
Some studies have found that more women are taken to hospital in ambulances than men, regardless of factors like age or severity of symptoms.64 However, other researchers have not found any differences between men and women's use of ambulances, considering that beliefs and clinical or demographic characteristics determine whether or not an ambulance is used.57,65
Gender biases in diagnosticsAs previously argued, ACS has different signs and symptoms in men and women, with a greater variety of symptoms in women. However, in the past, because women were not routinely included in the studies conducted, these differences have remained invisible, and so the “typical” symptoms in men (chest tightness and radiated pain) became the “rule”. In fact, talking about “atypical” symptoms in women is another example of how men are seen as the norm and women as the exception. Currently there is a large amount of scientific literature on the specific symptoms of ACS in women. Some studies have found that women with ACS have a greater variety of symptoms than men, have less chest pain (“typical” pain) and more headaches or back pain.66 The precordial pain that accompanies or precedes the ACS radiates more towards the jaw in women and not as much towards the left arm as it does in men. Women also experience nausea, vomiting, abdominal discomfort, fatigue and shortness of breath more frequently.14,67
The ECG is the key test to establish the diagnosis of ACS. However, women show changes in the ECG more frequently than men, generally linked to other factors. In addition, because women have a relatively lower exercise tolerance than men, stress tests are less sensitive.68,69 In relation to this, it has been demonstrated that the use of high sensitivity troponins and specific thresholds for each sex improves the diagnosis of myocardial infarction in women70–72; and that coronary angiography should not be used as the first test to diagnose myocardial ischaemia in young or middle-aged women who have few risk factors.73 Instead, the ESC guidelines recommend more modern imaging techniques and radiation-free imaging in the case of younger women with suspected myocardial ischaemia.68
With respect to the attitude towards male and female patients during the diagnostic process, there are gender biases in the way that doctors evaluate male and female patients and listen to their symptoms. Doctors are more attuned to the way that patients of their own sex present their history, and are more likely to use different interview styles depending on whether they are women or men.74 In some studies, when talking about the symptoms during the consultation, participating women reported that the doctors who attended them exhibited poor communication skills, and addressed them in a condescending and inattentive manner, feeling treated as hypochondriacs, and their symptoms attributed to stress, panic attacks or the menopause.75 In relation to this, women are more likely to be referred for diagnostic tests, to be diagnosed later, and to be misdiagnosed.76
Gender bias in treatmentsThe interest of researchers in the differential use of therapeutic procedures in men and women hospitalized due to ACS, increased in the early 1990s. Research on health care for women with cardiovascular disease has shown that they must have the same risk factors, symptoms, etc., than men, to receive the same level of treatment. “Being like a man” has historically been the price that women have had to pay for equality, according to some experts.6 The awareness of the gender bias in the treatment of ACS and CVD in general has increased since the nineties. Despite this greater awareness of these differences, they continue to be maintained over time, and are especially acute for young women.77 During the first decade of the 21st century, the Yentl syndrome was theoretically developed as the “cost of gender” in medical care.49 This increased awareness about the costs related to the detection and treatment of a patient who develops a disease that is not expected in their population group. At the same time, it became evident how the patriarchal society takes men's problems more seriously, so that women must be ill in the same way as men to receive quality care.
In addition, the “cardiac syndrome X” was developed,37 to explain the evidence that complaints of “typical” pain of heart disease in women may not find confirmation when diagnostic tests are used, as these are more appropriate to identify the disease in men than in women. This was also linked to the fact that men and women may be receiving the same treatment when that treatment was developed based on studies carried out in men, and significantly fewer women may be receiving treatments which have proven benefits in both sexes.9 Additionally, women admitted to hospitals with chest pain, undergo fewer exploratory tests, diagnostic and therapeutic procedures such as catheterizations or coronary by-passes.8
Therefore, according to recent studies, treatment of ACS should be performed according to the current guidelines for women and men, taking into account that women obtain the same benefits from bypass surgery and percutaneous coronary intervention as men.68
Post-coronary event recoveryThe experience of patients in the hospital, the information they receive from health personnel, and the participation of the patient in the decision-making process during the hospital phase, all this influences the recovery of patients with ACS and their subsequent quality of life.
In relation to gender and the management of ACS, a recent study shows that cardiovascular rehabilitation after myocardial infarction does not reach women and men equally.78–80 Women have more complications and more residual chest pain after coronary interventions for myocardial ischemia81,82; and a higher mortality and worse quality of life related to health after elective surgery of coronary bypass.83–85 In addition to differences in the therapeutic procedures, other disparities have also been found in the advice and recommendations on lifestyles, which are given to patients with ACS during their stay in the hospital. Older women are less satisfied with their participation in the decision-making process during the hospital phase and report that they have received prevention recommendations less frequently than men.86
Also important is to take into account the fact that the recovery process is different in men and women, with harmful outcomes for women. When patients return home, traditional gender roles might have a negative impact on women's recovery, as the sexual division of labour assigns them the role of primary caregivers of dependents and the family as a whole.87 During the early 2000, a systematic review had already suggested that married men attended rehabilitation more, and that married women attended less frequently because they need to fulfil their family responsibilities.88
The design and organization of rehabilitation programmes could also be criticized from a gender perspective, because they are not well adapted to women. Although it is assumed that cardiac rehabilitation can also have a positive impact on women's health, evidence of its benefits is mainly based on men, because men account for the majority of participants. In a study carried out in Sweden, women who took part in a cardiac rehabilitation programme were more likely to experience increases in angina, surgical procedures and readmission to hospital than those who did not take part. Some studies suggest that more comprehensive programmes are required, going beyond the traditional male-orientated ones.88
Conclusions and recommendationsThe belief that CVD is a male disease has led to a historical lack of clinical and epidemiological research. This review highlights how, during the last 10 years, research on CVD is still leading to diagnostic and treatment biases throughout the health care process. The belief that women are not susceptible to heart disease has also led to a lack of awareness of the disease amongst women and even medical personnel, resulting in gender inequalities in access to healthcare, including longer pre-hospital delays or lower attendance at cardiac rehabilitation programmes.
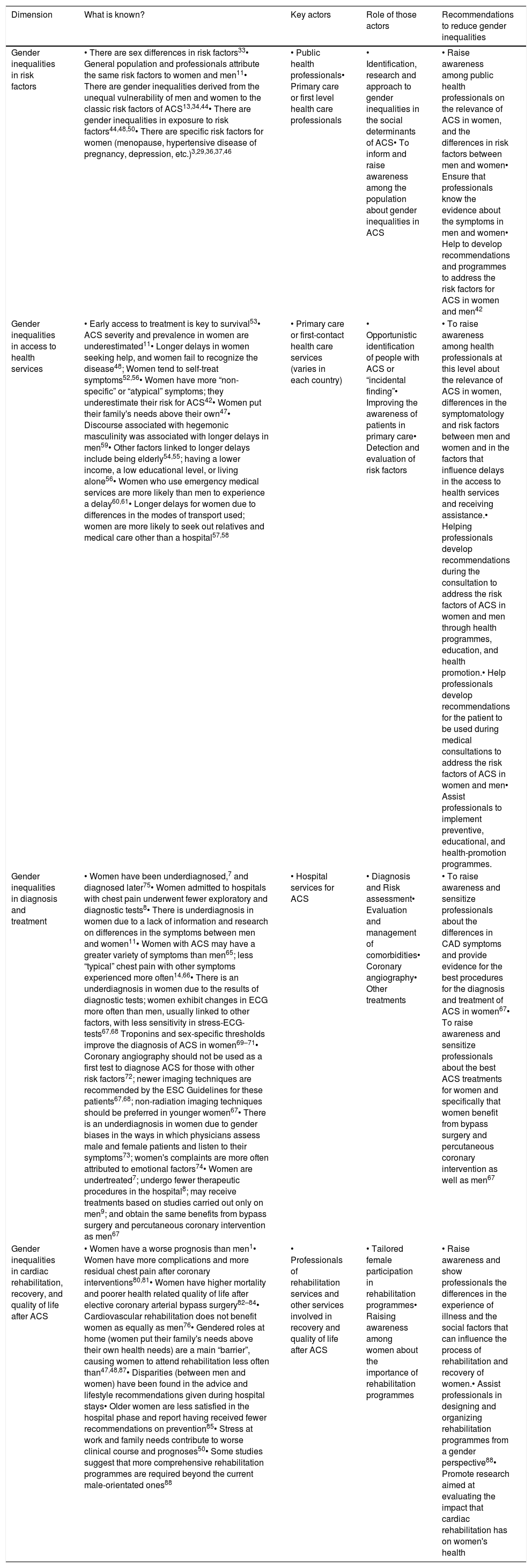
Table 1 includes the key points for gender inequalities in the ACS, from the perspective of health services. This table summarizes current knowledge, key professional actors in health care, the role of these actors, and recommendations to reduce gender inequalities at that level. These are the aspects to be taken into account when establishing health management decisions aimed to reduce gender inequalities in ACS among men and women.
Key points for gender inequalities in Acute Coronary Syndrome from the perspective of health services.
| Dimension | What is known? | Key actors | Role of those actors | Recommendations to reduce gender inequalities |
|---|---|---|---|---|
| Gender inequalities in risk factors | • There are sex differences in risk factors33• General population and professionals attribute the same risk factors to women and men11• There are gender inequalities derived from the unequal vulnerability of men and women to the classic risk factors of ACS13,34,44• There are gender inequalities in exposure to risk factors44,48,50• There are specific risk factors for women (menopause, hypertensive disease of pregnancy, depression, etc.)3,29,36,37,46 | • Public health professionals• Primary care or first level health care professionals | • Identification, research and approach to gender inequalities in the social determinants of ACS• To inform and raise awareness among the population about gender inequalities in ACS | • Raise awareness among public health professionals on the relevance of ACS in women, and the differences in risk factors between men and women• Ensure that professionals know the evidence about the symptoms in men and women• Help to develop recommendations and programmes to address the risk factors for ACS in women and men42 |
| Gender inequalities in access to health services | • Early access to treatment is key to survival53• ACS severity and prevalence in women are underestimated11• Longer delays in women seeking help, and women fail to recognize the disease48; Women tend to self-treat symptoms52,56• Women have more “non-specific” or “atypical” symptoms; they underestimate their risk for ACS42• Women put their family's needs above their own47• Discourse associated with hegemonic masculinity was associated with longer delays in men59• Other factors linked to longer delays include being elderly54,55; having a lower income, a low educational level, or living alone56• Women who use emergency medical services are more likely than men to experience a delay60,61• Longer delays for women due to differences in the modes of transport used; women are more likely to seek out relatives and medical care other than a hospital57,58 | • Primary care or first-contact health care services (varies in each country) | • Opportunistic identification of people with ACS or “incidental finding”• Improving the awareness of patients in primary care• Detection and evaluation of risk factors | • To raise awareness among health professionals at this level about the relevance of ACS in women, differences in the symptomatology and risk factors between men and women and in the factors that influence delays in the access to health services and receiving assistance.• Helping professionals develop recommendations during the consultation to address the risk factors of ACS in women and men through health programmes, education, and health promotion.• Help professionals develop recommendations for the patient to be used during medical consultations to address the risk factors of ACS in women and men• Assist professionals to implement preventive, educational, and health-promotion programmes. |
| Gender inequalities in diagnosis and treatment | • Women have been underdiagnosed,7 and diagnosed later75• Women admitted to hospitals with chest pain underwent fewer exploratory and diagnostic tests8• There is underdiagnosis in women due to a lack of information and research on differences in the symptoms between men and women11• Women with ACS may have a greater variety of symptoms than men65; less “typical” chest pain with other symptoms experienced more often14,66• There is an underdiagnosis in women due to the results of diagnostic tests; women exhibit changes in ECG more often than men, usually linked to other factors, with less sensitivity in stress-ECG-tests67,68 Troponins and sex-specific thresholds improve the diagnosis of ACS in women69–71• Coronary angiography should not be used as a first test to diagnose ACS for those with other risk factors72; newer imaging techniques are recommended by the ESC Guidelines for these patients67,68; non-radiation imaging techniques should be preferred in younger women67• There is an underdiagnosis in women due to gender biases in the ways in which physicians assess male and female patients and listen to their symptoms73; women's complaints are more often attributed to emotional factors74• Women are undertreated7; undergo fewer therapeutic procedures in the hospital8; may receive treatments based on studies carried out only on men9; and obtain the same benefits from bypass surgery and percutaneous coronary intervention as men67 | • Hospital services for ACS | • Diagnosis and Risk assessment• Evaluation and management of comorbidities• Coronary angiography• Other treatments | • To raise awareness and sensitize professionals about the differences in CAD symptoms and provide evidence for the best procedures for the diagnosis and treatment of ACS in women67• To raise awareness and sensitize professionals about the best ACS treatments for women and specifically that women benefit from bypass surgery and percutaneous coronary intervention as well as men67 |
| Gender inequalities in cardiac rehabilitation, recovery, and quality of life after ACS | • Women have a worse prognosis than men1• Women have more complications and more residual chest pain after coronary interventions80,81• Women have higher mortality and poorer health related quality of life after elective coronary arterial bypass surgery82–84• Cardiovascular rehabilitation does not benefit women as equally as men76• Gendered roles at home (women put their family's needs above their own health needs) are a main “barrier”, causing women to attend rehabilitation less often than47,48,87• Disparities (between men and women) have been found in the advice and lifestyle recommendations given during hospital stays• Older women are less satisfied in the hospital phase and report having received fewer recommendations on prevention85• Stress at work and family needs contribute to worse clinical course and prognoses50• Some studies suggest that more comprehensive rehabilitation programmes are required beyond the current male-orientated ones88 | • Professionals of rehabilitation services and other services involved in recovery and quality of life after ACS | • Tailored female participation in rehabilitation programmes• Raising awareness among women about the importance of rehabilitation programmes | • Raise awareness and show professionals the differences in the experience of illness and the social factors that can influence the process of rehabilitation and recovery of women.• Assist professionals in designing and organizing rehabilitation programmes from a gender perspective88• Promote research aimed at evaluating the impact that cardiac rehabilitation has on women's health |
Despite our improved understanding of sex-specific differences in presentation, risk factors, pathophysiology, diagnostic testing, and management strategies of ACS, women with ACS continue to experience worse outcomes than men. This disparity underscores the need for improved research and understanding of biological sex differences, elimination of subconscious gender bias in referral patterns, and improved application of existing research into clinical practice.19
There is an opportunity here for health systems to design and implement strategies and campaigns to raise awareness of ACS in women, reduce average delays in both sexes and lay out a research and management agenda to respond to these gaps. All developments must be tackled from a gender perspective, and healthcare services must play a key role in this respect. As patients’ first point of call, primary care is key to promoting cardiovascular health, raising awareness and improving early identification of the various risk factors and determinants of CVD in both men and women. Gender research and training of staff in hospitals would lead to better diagnosis, risk assessment and treatment for both sexes.
FundingSupported by the Grant PI19/00561 from the Ministry of Science, Innovation and Universities, Madrid, Spain.
Conflict of interestsThe authors declare that they have no conflict of interest.