Telemedicine has helped to make health care more efficient. However, to date no studies have measured its impact on infertility and fertility healthcare. We assessed the potential care benefits and clinical advantages of an initiative implementing electronic patient portal (EPP) for patients scheduled to undergo assisted reproduction treatment, to reduce waiting times for medical consultation and treatment.
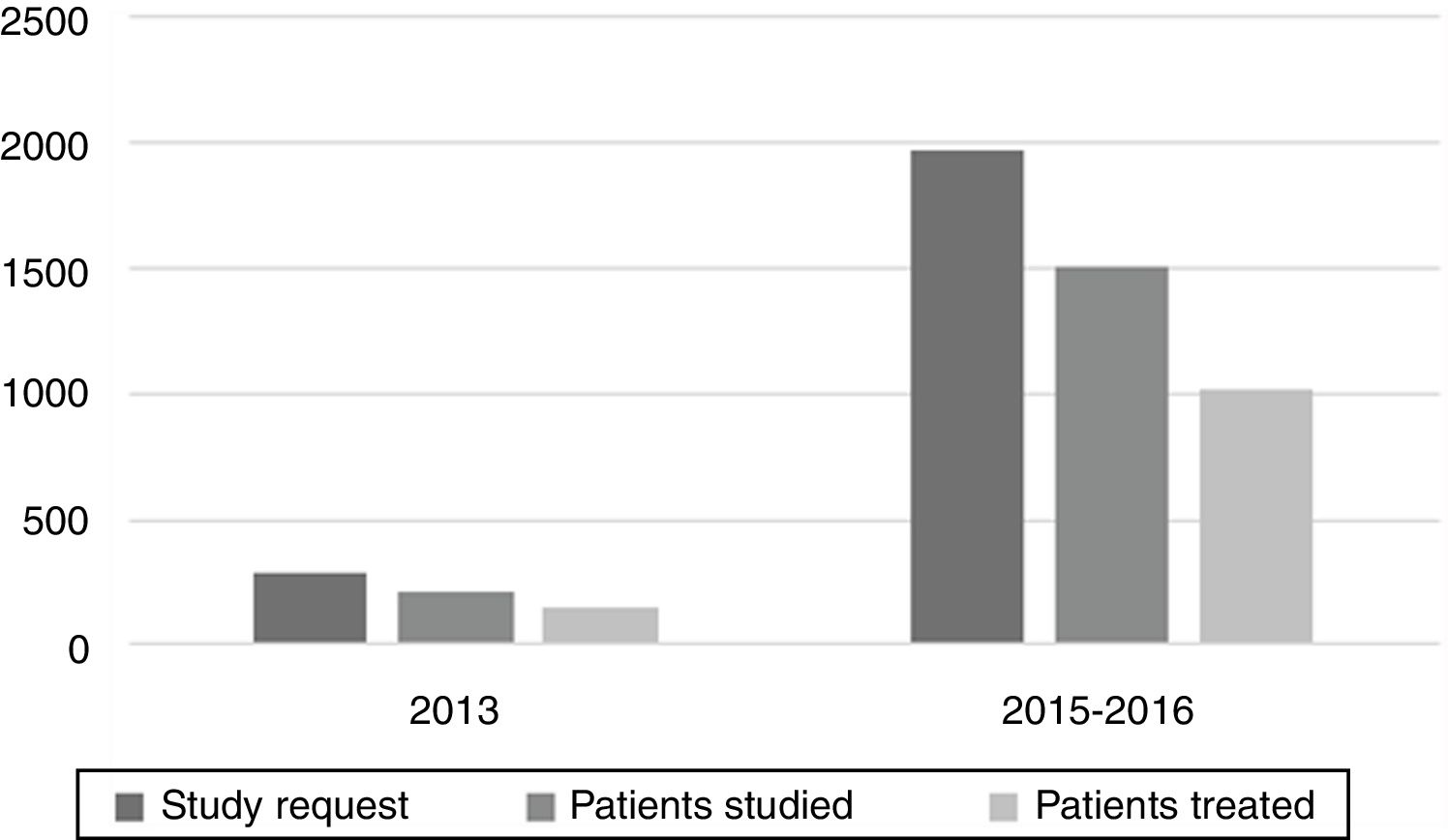
MethodsThis was designed as a retrospective cohort study. The experimental group comprised 1972 referral requests received by the assisted reproduction unit of our institution between 2015 and 2016, which were included in the group receiving telemedicine, while the control group was defined by 283 requests received in 2013, all of which were assigned face-to-face care.
ResultsWe found a statistically significant reduction in the experimental group in terms of the days elapsed between the receipt of the assessment request and the first outpatient visit (68 days vs. 180 days, p<.001). Time to initiation of treatment was also significantly lower in this group (169 days vs. 229 days; p<.001). The experimental group contained around 7 times as many patients receiving treatment as the control group. No differences were observed in the pregnancy rate (29.9% vs. 31.1%; p=.77) or in the complication rate (3.2% vs. 0%; p=.16).
ConclusionsUse of telemedicine in electronic portal patient form reduces the total waiting time involved in patient requests for infertility treatment and indirectly increases the number of patients treated, causing no negative impact on treatment outcome.
La telemedicina ha contribuido a incrementar la eficiencia de la atención sanitaria. Sin embargo, ningún estudio ha medido hasta la fecha su impacto en los tratamientos de infertilidad y fertilidad. Evaluamos los beneficios sanitarios y las ventajas clínicas potenciales de una iniciativa encaminada a introducir un portal de pacientes electrónico (PPE) para pacientes programados para reproducción asistida, en aras de reducir los tiempos de espera de las consultas y tratamientos médicos.
MétodosEstudio de cohorte retrospectiva. El grupo experimental incluyó 1.972 solicitudes de derivación recibidas por la unidad de reproducción asistida de nuestra institución entre 2015 y 2016, que fueron incluidas en el grupo que recibió telemedicina, mientras que el grupo control fue definido con las 283 solicitudes recibidas en 2013, a quienes se asignó una atención cara a cara.
ResultadosEncontramos una reducción estadísticamente significativa en el grupo experimental en términos de días transcurridos entre la recepción de la solicitud de valoración y la primera visita consulta externa (68 vs. 180 días; p<0,001). El tiempo hasta la iniciación del tratamiento fue también significativamente inferior en este grupo (169 vs. 229 días; p<0,001). El grupo experimental incluyó alrededor de 7 veces más pacientes que recibían tratamiento que el grupo control. No se observaron diferencias en términos de tasa de embarazos (29,9 vs. 31,1%; p=0,77) o de tasa de complicaciones (3,2 vs. 0%; p=0,16).
ConclusionesEl uso de la telemedicina en el PPE reduce el tiempo de espera total correspondiente a las solicitudes de los pacientes para el tratamiento de la infertilidad, e incrementa indirectamente el número de pacientes tratados, no causando ningún impacto negativo en el resultado del tratamiento.
The World Health Organization defines infertility as a disease of the reproductive system in which a woman fails to achieve a clinical pregnancy after 12 or more months of regular unprotected sexual intercourse.1 A common problem with a wide range of causes, infertility has a prevalence of approximately 15% among individuals of reproductive age, that is, 1 out of every 7 couples, and it affects an ever-growing number of people.2
Recent years have seen an increased number of new cases requesting care for this problem in gynaecology departments of the Spanish National Health System, particularly in the assisted reproduction units that form part of these departments. This spike in demand stems from a number of socioeconomic factors, especially, on the one hand, a shift in women's career goals and outlook, leading many women to postpone motherhood and thus negatively affecting their reproductive health, and on the other, the advent of new models of family and parenthood (single and same-sex parents) receiving full coverage under the Spanish welfare state. Though assisted reproduction services are available in private health-care facilities, for many the cost is prohibitive.
With demand increasing beyond the capacity of assisted reproduction units, treatment often follows a lengthy wait time, thus causing worry and uncertainty among patients and making a favourable reproductive outcome less likely. In addition, this situation triggers increased consumption of indirect care resources as a result of the burden placed on patients and their partners, including anguish, repeated hospital visits, feelings of uncertainty, and increased absenteeism. In some cases, prolonged wait times may disqualify potential patients from publicly-funded treatment if, at the end of the wait time, they are above the age limit for such treatments.
Average wait times for initial infertility-treatment consultations vary substantially across different regions of Spain, with residents of some areas of the country waiting as long as 18 months for their first visit. Similar variation is seen when initiating treatment, as patients of public facilities may wait anywhere between 12 and 18 months to have their first in vitro fertilization (IVF) cycle.3
The emergence of electronic medical records has brought about advances in data access and has improved the way we store and safeguard these data. Further, use of electronic medical records provides care professionals with more efficient workflows and improves interaction and communication not only between professionals, but also in doctor–patient relationships, as technological advances have enabled patients to easily and transparently access their data.4–6
Information and Communications Technology (IT) has become a mainstay in almost all areas of contemporary life. The use of this IT in all its forms in health care is called e-health. The term telemedicine refers to the use of lCT to deliver clinical services7,8 and this includes electronic patient portals (EPP).
In recent years, evidence has emerged on the benefit of telemedicine in different health fields.9–15 In case of gynaecology and obstetrics, e-health has been applied in medical management of abortion with good results16,17 and in the case of breast cancer survivors to improve their quality of life.18
In the field of assisted reproduction, telemedicine has been applied to evaluate the clinical results and the economic advantages of the telemonitoring of ovarian stimulation in IVF cycles, finding the same results as with traditional monitoring but showing greater patient satisfaction and her partner, a greater sense of empowerment, less stress and greater savings. Despite these results, the authors recognize the difficulty of bringing this to clinical practice due to limited evidence and reluctance to be implemented by healthcare providers.19,20
Specifically, the use of the EPP has been shown to be useful in the management and follow-up of chronic patients,21,22 and in the framework of primary care, Zhong describes a decrease in medical office visits and appointment no-show with the implementation of the EPP although he found no changes in the rate of cancellation of appointments.23 To our knowledge, there are no studies on the use of EPP in patients undergoing assisted reproduction treatments.
The primary aim of this study was to measure the extent to which the introduction of the EPP in assisted reproduction within the public health system had an impact on waiting times for consultation and treatment. Our secondary objectives were to study the increase in the number of patients treated, noting differences in reproductive outcome in both the experimental and control groups, and to determine whether any increase in complications was seen among the group of female patients receiving care via telemedicine service.
MethodsStudy design and settingWe carried out a retrospective observational study of patients who visited the Fundación Jiménez Díaz hospital assisted reproduction unit for treatment of infertility. All patients had been referred by either a primary-care physician or specialist, met all inclusion and exclusion criteria, and later underwent either intrauterine insemination (IUI) or IVF treatment.
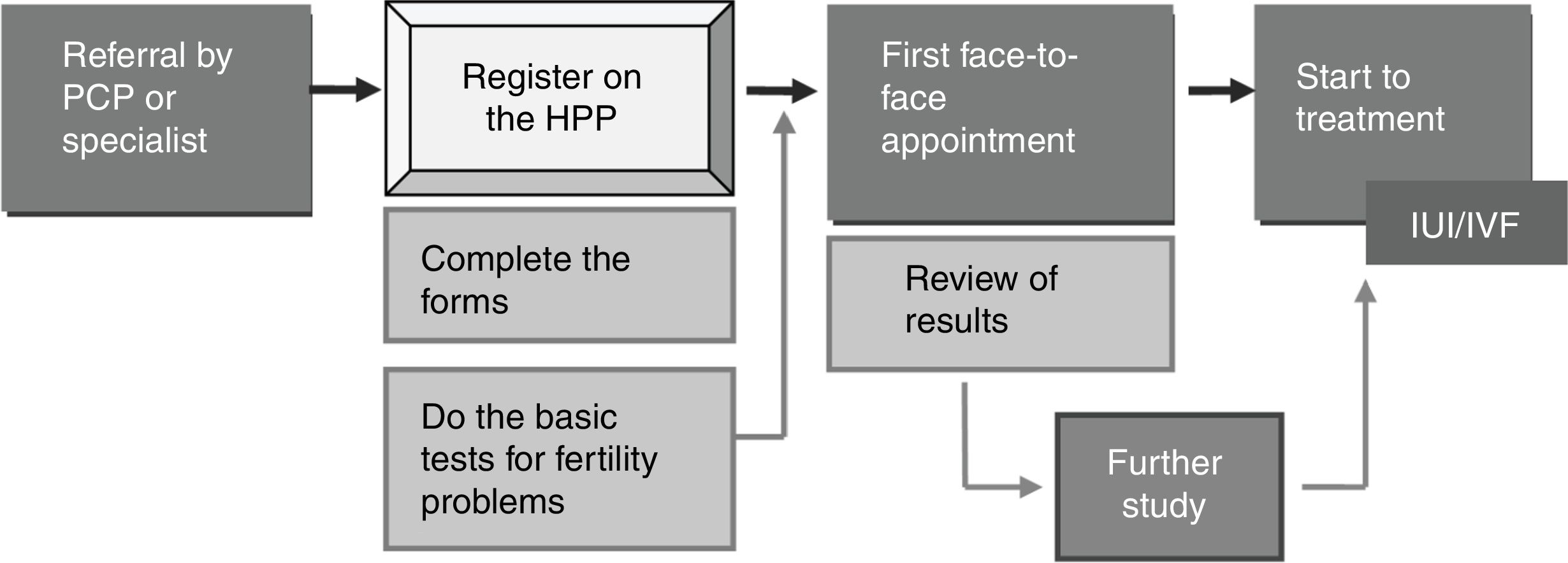
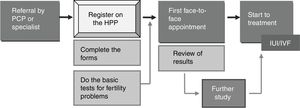
Inclusion and exclusion criteriaThe experimental group comprised patients who had requested evaluation in 2015 and 2016 and who accepted the use of telemedicine services. The mechanism for including patients in our study population via the e-health systems is as follows: The patient is referred to the assisted reproduction unit from her primary-care physician or from a specialist in gynaecology. The patient is informed that she must register on the hospital patient portal, a digital tool used in the institution. In addition to the verbal explanation by her health provider, the steps to follow to register in the patient portal are given in writing. After logging on to the portal, the patient and, where applicable, her partner, must complete the forms that will guide them through their medical records and provide them with personalized instructions on the tests they must undergo. Once the care team receives and studies these data, they enter all necessary tests in the patient portal, instructing the patient on the necessary procedures and appointments and scheduling hospital visits. This way, initial hospital visits are devoted to completing the patient's clinical history and reviewing the results of the completed tests; at this point, it is possible to indicate the reproductive treatment or complete full study if necessary (Fig. 1).
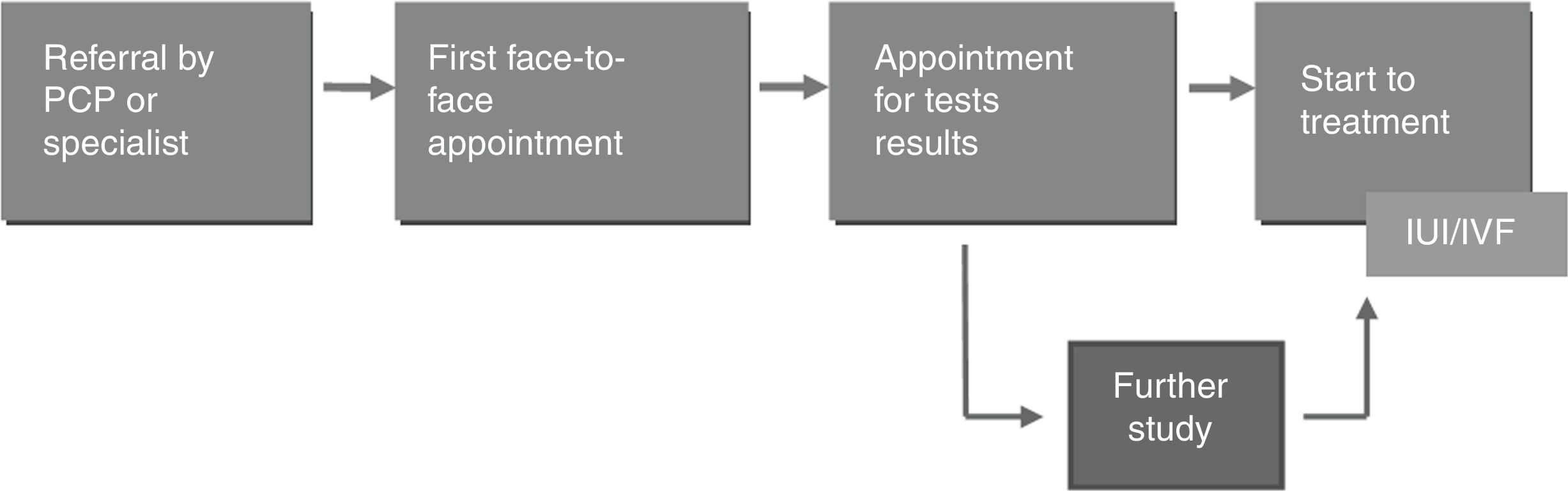
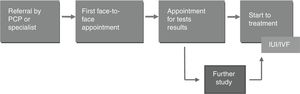
In parallel, a control group was formed, made up of those patients who used face-to-face channels to request a consultation for the same reason in 2013; in these cases, patients were referred to the assisted reproduction unit by their primary-care physician or a specialist in gynaecology. These patients were scheduled for a first face-to-face appointment, during which the anamnesis was carried out and the study of infertility was requested. Later, patients were scheduled to a new face-to-face appointment to receive their test results. Based on these results, patients either began treatment or underwent further study (Fig. 2).
The control group comprised all the patients treated in 2013 since in that year the use of the EPP in the assisted reproduction unit had not yet been launched. The study did not include patients treated in 2014 since this was a year of transition and implantation of the EPP. The experimental group included all the patients treated in the years 2015–2016, of which 91.2% agreed to use the telemedicine service.
Patients who had more than one request for assessment were scheduled for an appointment based on the most recent request. Similarly, those who had received more than one treatment were classified based on the data concerning the first treatment, regardless of whether the procedure consisted of IVF or IUI.
Study was presented and approved by the research ethics committee of the Fundación Jiménez Díaz.
Study population and data analysisData related to these women was taken into account when including patients in the study, as appointments were scheduled based on these data. To be included, patients had to be between 18 and 40 years of age with more than 1 year of infertility and with no other living, healthy offspring in common with their current partner.
We excluded from the study those patients with a history of voluntary sterilization and those for whom assisted reproduction or pregnancy was contraindicated.
The variables studied were as follows:
- •
Patient age at the time of the request for assessment by the assisted reproduction unit;
- •
Wait time for the initial visit, understood as the number of days elapsed between the first request for a fertility study until the day of the actual appointment;
- •
Total wait time for initiation of treatment, or the number of days between the time the request was made and the beginning of treatment;
- •
Number of patients treated;
- •
Dropout rate, that is, the number of patients who discontinued participation prior to the first face-to-face visit;
- •
Pregnancy rate: ongoing clinical pregnancy at 7–8 weeks of gestation;
- •
Complication rate, defined as moderate or severe ovarian hyperstimulation syndrome.
Standard descriptive statistical analyses were used to define the sample characteristics. An analysis of wait times was performed using median values, as the data were not normally distributed. To compare categorical variables we used Pearson's Chi square test, and continuous variables were analyzed using the Mann–Whitney U test for independent samples. Student t test was used for independent samples to compare dichotomous qualitative variables and quantitative variables.
All analyses were carried out using the SPSS statistical package, and p values <0.05 were considered statistically significant.
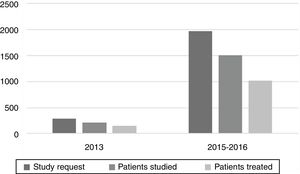
ResultsA total of 1972 requests for assessment were included in the experimental group, all received in 2015 or 2016. Of these, 76.4% (n=1507) were processed using EPP, after which they had a hospital visit to review their results. 283 requests received in 2013 were included in the control group, 208 of which (73.5%) received face-to-face care beginning with an initial outpatient consultation.
Four hundred eighty-five patients in the experimental group (32.2%) and 57 individuals in the control group (27.4%) did not receive treatment and were discharged by the unit despite having had an initial visit. The reasons these patients did not undergo treatment varied: some only wished to have a study of their ability to reproduce but did not want treatment, while others were advised against assisted reproduction due to a diminished ovarian reserve or because they were over 40 years of age at the time they were evaluated as candidates. No statistically significant differences were observed in the number of patients who did not undergo treatment for any of these reasons (p=0.165).
Patient ageThe average age of patients in the experimental group was 34.95±3.6 years, and 35.15±3.6 years was the average age for the control group. A comparison of both means failed to evidence statistically significant differences between the two groups (difference in mean values, 0.2 years; 95% confidence interval (CI): −0.36 to 0.74).
Number of patients treatedAmong the patients in the experimental group who had a visit to review their preliminary test results, 67.8% (n=1022) began treatment. In the control group, 72.6% (n=151) received the treatment. A comparison of the number of patients undergoing treatment in each group had been performed and this difference did not reach statistical significance (p=0.16).
Dropout rateFour hundred sixty-five patients in the experimental group (23.6%) and 26.5% of those in the control group (n=75) failed to report for their first scheduled visit. The result of Pearson's Chi square test was 1.16 (p=0.28), indicating that there were no statistically significant intergroup differences in the dropout rate.
Waiting time until first consultationAn analysis of the time elapsed between requests for evaluation and the initial visit showed that the median number of days for the experimental group was 68, with an interquartile range of 45. The median wait time for the control group, on the other hand, was 180 days, with an interquartile range of 62 days. When these two periods were compared the difference was statistically significant (p<0.001).
Wait time until start of treatmentThis variable measures the number of days between the time the request was made and the beginning of treatment. There was a median wait time of 169 days in the experimental group (interquartile range, 108.5 days). The median wait for the control group, on the other hand, was 229 days, with an interquartile range of 259 days. When these two periods were compared using, the difference was statistically significant (p<0.001). It is important to note that this shortening of time is mainly due to the reduction of days until the first consultation.
Pregnancy rateThe final experimental group comprised 1022 patients, and 151 patients were included as controls. The success rate in the experimental group was 29.9% (n=306), while 31.1% of controls achieved pregnancy (n=47). Pearson's Chi square test was 0.09, and the asymptotic significance value 0.77; as a result, the differences in successful pregnancy between groups did not reach statistical significance.
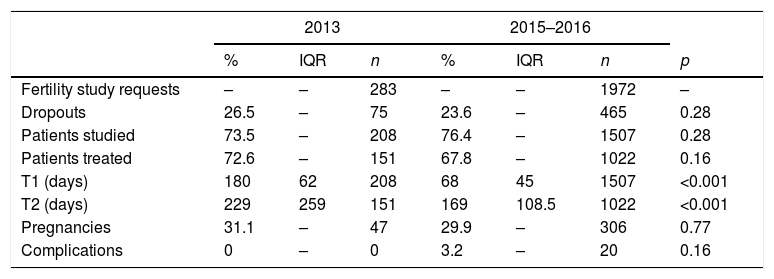
ComplicationsComplications were observed in 3.2% of patients in the experimental group (n=20), and no complications were recorded in the control group. An analysis carried out using Pearson's Chi square test produced a value of 2.0, and the asymptotic significance value was 0.16; despite these results, there were no statistically significant differences found between the two groups studied. Table 1 presents a summary of all these findings.
Results of a comparative study variables among groups.
| 2013 | 2015–2016 | ||||||
|---|---|---|---|---|---|---|---|
| % | IQR | n | % | IQR | n | p | |
| Fertility study requests | – | – | 283 | – | – | 1972 | – |
| Dropouts | 26.5 | – | 75 | 23.6 | – | 465 | 0.28 |
| Patients studied | 73.5 | – | 208 | 76.4 | – | 1507 | 0.28 |
| Patients treated | 72.6 | – | 151 | 67.8 | – | 1022 | 0.16 |
| T1 (days) | 180 | 62 | 208 | 68 | 45 | 1507 | <0.001 |
| T2 (days) | 229 | 259 | 151 | 169 | 108.5 | 1022 | <0.001 |
| Pregnancies | 31.1 | – | 47 | 29.9 | – | 306 | 0.77 |
| Complications | 0 | – | 0 | 3.2 | – | 20 | 0.16 |
T1: median wait time (days) until first consultation. T2: median wait time (days) until start of treatment. IQR: interquartile range.
In this study, we have found statistically significant differences between the experimental and control group with regard to wait times for both initial visits and for start of treatment. In the case of the time until the start of treatment (understood as the days elapsed from the request for assessment until the start of the treatment), the reduction occurs mainly due to the decrease in the days until the first consultation. As in any company, including the health sector, the resources available are limited. In the control group, the sterility study is requested in the first face-to-face consultation, citing patients to a new appointment to evaluate the test results. These result appointments occupy gaps in the patients schedule that could be used for new patients.
When using the EPP, patients not only filled out a questionnaire giving data about their medical history, the basic sterility study was also requested, whose request sheets were loaded in the patient's portal with the intention of having it completed before the first consultation face-to-face, so when they arrived at this, the medical history was completed, the tests were reviewed and the treatment was indicated in that same consultation, leaving free appointments to be able to schedule new patients. After this action, it was possible to go from an average waiting time of 180 days to 68 days while maintaining the same resources used in the control group.
The increase in new patients (about 7 times more) had an impact on other processes such as laboratory work that had to be reorganized so that it could absorb new beginnings of fertility treatments which increased the time between the indication of treatment until the completion of this. Despite this increase, the average time to start treatment since the patient was referred to the assisted reproduction unit was significantly shorter in the experimental group (169 days vs. 229 days; p<0.001).
Use of telemedicine in EPP form enables the initial consultation and review of test results to be accomplished in a single face-to-face visit, giving all patients the opportunity to have an updated basic fertility study as recommended by clinical practice guidelines. Further, this approach optimizes subspecialist time and facility resources, making this a more efficient approach to patient care, which, as seen in the satisfaction surveys administered to users of telemedicine services, translates into greater patient satisfaction.
These forms filled out by the patients are a help when conducting the clinical interview with the patients but are always verified during the development of them. Problems have rarely been detected when requesting the basic sterility study through the EPP because the analytical requests were not loaded correctly in the EPP, usually due to a system error or because the health provider did not know how to include the patients in the telemedicine circuit. Another problem detected was that having been correctly registered in the EPP and with the requests correctly made, the patients did not perform the requested medical tests. This was more frequent in non-Spanish-speaking patients and with less access to technologies. Therefore, it is important not only to consider the characteristics of the technology, but also the characteristics of the end user.24
In the field of assisted reproduction, efforts to reduce wait times take on added importance given that the older the patient, the greater the difficulties they encounter in achieving pregnancy.25 In addition, public-system reimbursement for these procedures is limited to patients between the ages of 18 and 50 years.26,27 Despite this difference in wait times, our results reveal no significant difference in average patient age between both groups. In fact, had the 2013 mean wait times for initial assessment remained unchanged, 2.8% of the patients in our study sample who requested fertility evaluation in 2015 and 2016 would have reached age 40 without having begun the process of assessment and subsequent treatment.
Though a number of published studies have demonstrated the efficiency and financial benefits of telemedicine in other fields of medicine,28–34 none has specifically addressed the reduction in wait times that results from the introduction of this new technology within reproductive medicine. Nonetheless, the Madrid regional government, in its 2016–2019 Comprehensive Plan to Improve Waiting Times for Surgical Interventions, has included measures aimed at driving the use of new information-technology systems to improve clinical care and administration of waiting lists for surgery, consultations, and diagnostic testing.35
The main obstacles to change appearing in the literature are the failure to understand the system, the lack of sufficient technological means, patient mistrust and worry at the prospect of foregoing face-to-face visits, and the absence of physician-patient rapport underlying a positive working relationship.36 A sufficient empirical basis on the adoption of mobile technologies in medicine is lacking, particularly with regard to the acceptance of such tools as the EPP, and most of the research that has been conducted on this issue has focused on primary care and has sought to determine user volumes and their demographic characteristics.37–39
In previous studies conducted in the United States, it has been described that sex, age, race, language and the insurance are the most important conditions to register in the EPP noting that young white women with private insurance were those that did it more frequently.40–42 Once registered in the EPP, the frequency of use also seems to be different, women and those over 65 years old being the ones who used the portal most frequently. In the case of the elderly this was due to a higher incidence of chronic diseases, but in the case of women the cause is less clear.43
The implementation of the EPP in our unit did not present major acceptance problems among other reasons because the patients included in the research tended to be young, highly motivated and a large percentage of them were women, thus increasing their likelihood to adopt new technologies that bear a close resemblance to those they use in other aspects of their lives. The percentage of patients who decided not to use the patient portal in the experimental group was 8.8% and was generally due to linguistic problems or due the lack of knowledge of the health provider about how include the patient in the telemedicine circuit.
Once enrolled in the EPP, patients showed good adherence and satisfaction with it, which is reflected in the fact that no statistically significant differences were detected in the drop-out rate between both groups. When this phenomenon occurs, it may be driven by spontaneous pregnancy, lengthy wait times, feelings of uncertainty, lost hours of work, and the stress that accompanies the experience44–46; therefore, use of these technologies may lower the number of patients and couples who discontinue treatment.
One of the aspects not accounted for in this study is the degree to which the institution of this system impacts upon other related care services. It is reasonable to expect that the increased patient flow triggered when e-health systems are used will increase referrals to other hospital departments, possibly surpassing the capacity of these services if this spill-over effect is not taken into consideration. Proper roll-out and use of the system, therefore, requires adaptation and coordination with all other departments.
Although in our study the experimental group is composed of the requests received in 2 years, it is evident the increase of requests for assessment respect to the control group (1 year). It is likely that this increase is due in large part to the reduction in the times of study and treatment in itself, which allows us to serve more requests, as well as the preference of patients by our assisted reproduction unit with respect to others for the same reason. Thus, the fact that the experimental treated group comprised around 7 times the number of patients as did the control group (Fig. 3) is an indication of the degree to which the system has been integrated as one of the components of the public health system and adopted as such by patients. This use of care resources could be validated by other assisted reproduction units belonging to the Spanish National Health System that seek to bolster their efficiency.
To conclude, use of telemedicine in EPP form in public-sector reproductive care leads to reduced wait times for patients requesting infertility treatment, limiting delays for initial assessment visits and initiation of treatment. Implementing this approach enables services to provide care for a greater number of patients without sacrificing treatment efficacy or patient satisfaction, optimizing the use of physical hospital resources and making assisted reproduction treatment more accessible.
FundingThis study was carried out independently by the coordinating researcher, who worked with no outside funding. Neither the collaborating researchers nor the patients included in the study received compensation of any kind for participating.
Conflict of interestThere are no conflict of interest.